Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.4 Lisboa ago. 2020
https://doi.org/10.1159/000503454
CLINICAL CASE STUDY
A Case of Brucellosis with Possible Ileal Involvement
Um Caso de Brucelose com Possível Envolvimento Ileal
Joana Rodrigues dos Santos, Ryan Silva, Priscila Nejo, Tânia Vassalo, Alexandra Coimbra, Lígia Peixoto
Serviço de Medicina I, Centro Hospitalar Universitário Lisboa Norte, Hospital de Santa Maria, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Introduction: Brucellosis is a zoonotic disease that can involve different organs and tissues. Fever, fatigue, lymphadenopathy, hepatosplenomegaly, cytopenia, and arthritis are the usual modes of presentation. Gastrointestinal manifestations of human brucellosis are common but documented ileal involvement is extremely rare. Case Description: A 68-year-old female presented with a history of 10 days of intense temporal migraine, photophobia, and phonophobia with partial response to paracetamol. The patient referred night sweats, anorexia, and colicky abdominal pain after her meals for the past 4 months followed by diarrhea. She denied nausea, vomiting, hypersensitivity of the scalp, blurry vision, melena, or rectal bleeding. She denied travelling or contact with animals. Physical examination revealed fever (38.3 ° C) and splenomegaly. Laboratory workup revealed Hb 7.8 g/dL, leukopenia (3.47 × 109/L), C-reactive protein 5.94 mg/dL, and erythrocyte sedimentation rate 23 mm/h. Abdominal ultrasound showed hepatic steatosis and mild homogeneous splenomegaly. Chest radiography was normal. Lumbar puncture; transcranial, carotid, and temporal arteries Doppler, and head computed tomography (CT) did not show any significant changes. Abdominal CT showed diffuse thickening of the ileum and some mildly swollen locoregional lymph nodes. Fecal calprotectin was not elevated. Blood cultures and serologies were positive for Brucella (positive Rose-Bengal test, ELISA IgM-positive, IgG-negative anti-brucella antibody serology and positive Huddleson reaction – titer 1: 320). The patient was started on rifampicin 600 mg/ day and doxycycline 100 mg q. 12 h for 10 weeks with good clinical and analytical response. Upper and lower gastrointestinal endoscopy were normal, although the last was done already under antibiotic treatment. Discussion: Although gastrointestinal manifestations of brucellosis are quite common, ileitis is thought to be extremely rare. In countries where brucellosis is endemic, doctors must consider this diagnosis when faced with patients with systemic symptoms and diarrhea or abdominal pain. Early recognition of brucellosis and institution of appropriate therapy usually leads to a good recovery without complications.
Keywords: Brucellosis, Diarrhea, Ileitis, Huddleson reaction
RESUMO
Introdução: A brucelose é uma zoonose que pode envolver diferentes órgãos e tecidos. A apresentação habitual consiste em febre, cansaço, linfadenopatias, hepatoesplenomegalia, citopenias ou artrite. As manifestações gastrointestinais de brucelose humana são comuns, mas a documentação do envolvimento ileal é extremamente rara. Descrição do caso: Doente de 68 anos, sexo feminino, apresentou-se com quadro com dez dias de evolução de cefaleia temporal intensa, fotofobia e sonofobia, com resposta parcial a terapêutica com paracetamol. A doente referia sudorese noturna, anorexia e dor abdominal tipo cólica após as refeições durante os últimos quatro meses seguida de diarreia. Negava náuseas, vómitos, hipersensibilidade do escalpe, visão turva, melenas ou retorragia. Negava viagens ou contacto com animais. Ao exame objetivo destacava-se febre (38,3 ° C) e esplenomegalia. Os estudos laboratoriais revelaram Hb 7,8 g/dL, leucopenia (3,47 × 109/L), proteína C-reativa 5,94 mg/dL, velocidade de sedimentação 23 mm/h. A ecografia abdominal mostrou ligeiro aumento do fígado (estatose) e esplenomegalia ligeira e homogénea. Radiografia de tórax normal. Punção lombar; Doppler transcraniano, carotídeo e das artérias temporais e tomografia computorizada (CT) craniana sem alterações significativas. A CT abdominal mostrou espessamento difuso do íleon e algumas pequenas adenopatias locorregionais. As hemoculturas e serologias foram positivas para Brucela (Rosa Bengala positivo, serologia anti-Brucela ELISA IgM-positivo, IgG-negativo; reação de Huddleson positiva – título 1: 320). Foi iniciada terapêutica com rifampicina 600 mg/dia e doxiciclina 100 mg de 12 em 12 h durante 10 semanas com boa resposta clínica e laboratorial. Endoscopia digestiva alta e baixa sem alterações, apesar de a última ter sido realizada já sob terapêutica antibiótica. Discussão: Embora as manifestações gastrointestinais de brucelose sejam comuns, pensa-se que a ileíte seja extremamente rara. Em países onde a brucelose é endémica, os médicos devem considerar esta hipótese diagnóstica quando na presença de sintomas sistémicos e diarreia ou dor abdominal. O reconhecimento precoce da brucelose e a instituição de terapêutica adequada levam geralmente a uma boa recuperação sem complicações.
Palavras-Chave: Brucelose, Diarreia, Ileíte, Reação de Huddleson
Introduction
Brucellosis is a zoonotic disease that can involve different organs and tissues [1]. Fever, fatigue, lymphadenopathy, hepatosplenomegaly, cytopenia, and arthritis are the usual modes of presentation [2]. Gastrointestinal manifestations of brucellosis in humans are less common than systemic symptoms and may manifest as anorexia, nausea, vomiting, abdominal pain, diarrhea, or constipation [3]. Abdominal pain is present in 19% of patients with brucellosis [4], and diarrhea has been reported as prominent gastrointestinal symptom in 6 to 16% of patients [5]. To our knowledge, only three cases have been reported of brucellosis with documented ileal involvement [6–8]. Doctors must be alert to the possibility of this diagnosis when faced with these gastrointestinal manifestations, especially in countries where brucellosis is endemic. Early recognition of brucellosis and institution of appropriate therapy usually lead to a good recovery without complications [9].
Clinical Case
Our patient was a 68-year-old woman with a history of high blood pressure since the age of 53, dyslipidemia, gastroesophageal reflux, obesity (BMI 31), and depression. She was medicated with irbesartan 150 mg, fluoxetine 20 mg, sinvastatin 20 mg, esomeprazol 20 mg, and acetylsalicylic acid 100 mg.
The patient presented to our hospital complaining of intense temporal migraine, photophobia, and phonophobia with partial response to paracetamol for the past 10 days. In the past 4 months, she had also complained of post-prandial bloating, non-selective anorexia, pyrosis, heartburn, and weight loss of 10% of her body weight. She had epigastric colicky pain starting approximately 1 h after her meals, followed by diarrhea (without blood, steatorrhea, mucus, or pus) – approximately 4 episodes per day. Also, she had profuse night sweating and occasional low-grade fever and was feeling more depressed than usual. She denied nausea, vomiting, hypersensitivity of the scalp, blurry vision, melena, or rectal bleeding. The patient denied recent travels outside of Portugal and drug consumption other than the prescribed ones referred to above. She reported unpasteurized dairy products consumption during the previous months.
On physical examination, there were no pathological findings except for a tympanic temperature of 38.3 ° C, discoloration of the mucosa, and a mild splenomegaly. Laboratory investigation results were as follows: normocytic hypochromic anemia (Hb 7.2 g/dL; MCV 83.3 fL; MCH 26.8 pg), discrete leukopenia with a leukocyte count of 3.47 × 109/L, neutrophils 1.86 × 109/L, lymphocytes 1.31 × 109/L, platelet count 286 × 109/L, discrete ferritin increase of 209.9 ug/L, normal serum iron, TIBC, and transferrin saturation, low vitamin B12 levels – 175 pg/mL, folates 7.2 ng/mL, haptoglobin 184 mg/dL. Her erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were slightly elevated – ESR 23 mm/h, CRP 5.94 mg/dL, AST 17U/L, ALT 17 U/L, total bilirubin 1.66 mg/dL, GGT 26 U/L, LDH 285 U/L, K+ 2.9 mmol/L. The protein electrophoresis showed a discrete hypogammaglobulinemia. Monospot test was negative. The HBsAg, anti- HBc IgM, anti-HAV IgM, and anti-HCV tests were negative. Electrocardiogram, chest X-ray, and head computed tomography (CT) were normal. Abdominal ultrasound showed a discrete increase in the liver’s dimensions, suggestive of hepatic steatosis and a mild to moderate homogeneous splenomegaly.
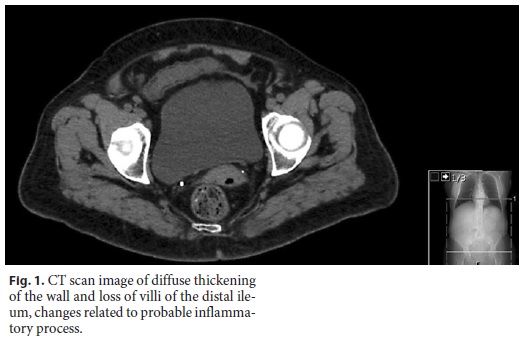
In order to exclude malignancy, a whole-body CT scan was performed, which confirmed the presence of splenomegaly and also showed a diffuse thickening of the wall and loss of villi of the distal ileum and some locoregional mildly swollen lymph nodes associated, unspecific, suggestive of an inflammatory process. Myelogram showed a depletion of iron stores. Bone biopsy was unremarkable. No myelocultures were performed (Fig. 1). Autoimmunity studies were unremarkable. To exclude giant cell arthritis, carotid and transcranial ultrasound and temporal artery ultrasounds were done and were also unremarkable.
Serological studies showed an immunological scar for EBV and CMV and were negative for Q fever, toxoplasmosis, and syphilis. IGRA test was negative. Cytochemical evaluation of liquor was unremarkable and bacterial studies were negative. Brucella spp. was detected in all three blood cultures. ELISA studies also showed a positive IgM anti-brucella antibody and negative IgG. Huddleson’s reaction titer was positive at 1: 320. Rose-Bengal test was also positive.
The patient was diagnosed with subacute brucellosis with hematological and possible ileal involvement. She had started vitamin B12 at admission and 5 days after she started rifampicin 600 mg/day and doxycycline 100 mg b.i.d. for 8 weeks.
During her stay at the hospital, the patient complained of back pain and underwent a spine CT scan, which excluded spondylodiscitis. Also, an echocardiogram was performed and there was no evidence of vegetations nor any other relevant alterations. Upper gastrointestinal endoscopy showed chronic gastritis. Colonoscopy was only performed 21 days after initiation of antibiotics (the patient refused to take this exam before) and was unremarkable. No biopsies were taken.
During the first days after her admission, the patient frequently needed medication for the headache or abdominal discomfort. Thirteen days after her admission, she was discharged. By that time, her hemoglobin levels were already higher (Hb 9.2 g/dL) and leukopenia was less severe (3.88 × 109/L). She did not complain of headache (which was associated with fever spikes) or abdominal pain and the stool consistency increased.
On follow-up after 8 weeks of therapy, the patient presented no headache and no night sweats and was feeling much better, but because she still presented diarrhea, antibiotics were prolonged for another 2 weeks. After this time, the patient became asymptomatic. Huddleson’s titers were positive until 10 months after therapy discontinuation. By this time, her Hb was 10.4 g/dL; she had no leukopenia, ESR 15 mm/h, and no vitamin B12 deficiency.
Discussion
Brucellosis is a systemic zoonotic infection transmitted by contact with fluids of infected animals or ingestion of their unpasteurized dairy products or undercooked meat [10]. It is among the most common zoonoses in the world [11]. The reported annual incidence of brucellosis in Portugal is 0.5 per 100,000 population, higher than in all other European countries except for Greece (1.2: 100,000) [12]. Brucellosis is endemic in Portugal [13].
The diagnosis of brucellosis can be challenging since it can affect any body organ and system and can mimic several infectious and noninfectious diseases [14]. Also, it can range from an asymptomatic disease to a fatal illness, and it can virtually affect any organ or system [9]. Patients may present with systemic symptoms like insidious fever, sometimes with an irregular pattern (which is why this disease is also known as undulant fever), night sweats, myalgia, arthralgia, anorexia, depression, headache, and lethargy [9]. According to the length and severity of symptoms, the disease is arbitrarily classified as acute (less than 8 weeks), subacute (from 8 to 52 weeks), or chronic (more than 1 year). Any organ involvement is often referred to as localized disease [15].
In about 30% of cases, there is focalization of the infection [9, 16, 17]. Hematological involvement with anemia and leukopenia, like our patient presented, is relatively common [18]. Although gastrointestinal complaints are common in infections by Brucella spp., documented specific ileum lesions caused by Brucella spp. are rare, which might be a reflection of lack of access to CT scan and endoscopic procedures in many of the countries where it is endemic.
To our knowledge, only three cases have been reported of brucellosis with documented ileal involvement. One was an 11-year-old female with radiographic evidence of acute ileitis during an outbreak of infection caused by Brucella melitensis. The diagnosis was made on the basis of blood cultures, and brucella-associated ileitis resolved completely after appropriate antibiotic treatment [6]. Another case was a 15-year-old male patient with probable intestinal brucellosis associated with celiac artery and superior mesenteric artery stenosis verified in CT angiography and with ileum mucosa and submucosa thickening visible on abdominal ultrasound and CT scan of the intestine. Endoscopic examination revealed many irregular ulcers in the narrowed lumen of the terminal ileum, and pathological features of the terminal ileum suggested severe acute and chronic inflammation of the intestinal mucosa. Huddleson’s reaction titer was positive at a dilution of 1: 160 (in two separated samples, and the titer did not rise in the second) and Rose-Bengal test results were also positive. His symptoms, imaging results, history of eating undercooked roast lamb and beef, and serologic tests were highly suggestive of brucellosis. Unfortunately, multiple Brucella spp. blood cultures were undertaken and turned out to be negative [7]. There was a reference to a third case in an epidemiological study of the features of brucellosis in the country of Georgia that included 81 participants, although it is not better described in the article [8]. In our case, the vascular territories were not evaluated.
The diagnosis of brucellosis requires the isolation of Brucella from blood or body tissues, or the combination of suggestive clinical presentation and positive serology [15]. Serological testing does not provide direct evidence for the presence of the pathogen, hence, isolation of Brucella spp. from the clinical specimen is considered to be the gold standard [19]. In our case, blood cultures were positive for Brucella spp., establishing the diagnosis of brucellosis and contributing to the exclusion of other differential diagnoses, such as other causes of infectious diarrhea, inflammatory bowel disorders, or lymphoma. Due to the absence of biopsies, it is impossible to guarantee that ileitis was caused by Brucella spp. Another plausible hypothesis would be that of ileitis caused by Mycobacteria tuberculosis, which would also partially respond to the instituted therapy. However, and according to Occam’s principle, most immunocompetent patients have a single pathology that explains all signs and symptoms. Additionally, IGRA test was negative (having a high negative predictive value) and there was no recurrence of symptoms after treatment discontinuation, substantially reducing the probability of this concomitant diagnosis.
This patient presented as risk factors for the development of brucellosis not only the consumption of unpasteurized dairy products, but also the use of esomeprazole, which may have played a role. Antacids or H2 receptor blockers may increase susceptibility to brucellosis by diminishing the gastric juice pH [15].
This case highlights the importance of considering the diagnosis of brucellosis in patients with systemic symptoms in countries where brucellosis is endemic. Few cases of ileitis caused by Brucella spp. were reported, but it is a serious condition that requires a high index of suspicion. Due to lack of access to CT scan and endoscopy in some of the countries where brucellosis is endemic, it may be an underdiagnosed condition. With the right treatment, this condition can have a favorable outcome.
References
1 Mantur BG, Amarnath SK, Shinde RS. Review of clinical and laboratory features of human brucellosis. Indian J Med Microbiol. 2007 Jul;25(3):188–202.
2 Erduran E, Makuloglu M, Mutlu M. A rare hematological manifestation of brucellosis: reactive hemophagocytic syndrome. J Microbiol Immunol Infect. 2010 Apr;43(2):159–62.
3 Salih SB, Alothman A. Acute Brucellosis Presenting as Gastroenteritis. Case Report. Infect Dis (Auckl). 2013;6:35–7.
4 Dean AS, Crump L, Greter H, Hattendorf J, Schelling E, Zinsstag J. Clinical Manifestations of Human Brucellosis. A Systematic Review and Meta-Analysis. PLoS Negl Trop Dis. 2012 Dec;6(12):e1929. [ Links ]
5 Ablin J, Mevorach D, Eliakim R. Brucellosis and the gastrointestinal tract. The odd couple. J Clin Gastroenterol. 1997 Jan;24(1):25–9.
6 Petrella R, Young EJ. Acute brucella ileitis. Am J Gastroenterol. 1988 Jan;83(1):80–2.
7 Wang M, Zhu Q, Yang Q, Li W, Wang X, Liu W, et al. Intestinal brucellosis associated with celiac artery and superior mesenteric artery stenosis and with ileum mucosa and submucosa thickening: A case report. Medicine (Baltimore). 2017 Jan;96(2):e5893. [ Links ]
8 Akhvlediani T, Bautista CT, Garuchava N, Sanodze L, Kokaia N, Malania L, et al. Epidemiological and Clinical Features of Brucellosis in the Country of Georgia. PLoS One. 2017 Jan;12(1):e0170376. [ Links ]
9 Colmenero JD, Reguera JM, Martos F, Sánchez-De-Mora D, Delgado M, Causse M, et al. Complications associated with Brucella melitensis infection: a study of 530 cases. Medicine (Baltimore). 1996 Jul;75(4):195–211.
10 Khan M, Zahoor M. An Overview of Brucellosis in Cattle and Humans, and its Serological and Molecular Diagnosis in Control Strategies. Trop Med Infect Dis. 2018 Jun;3(2):65. [ Links ]
11 Seleem MN, Boyle SM, Sriranganathan N. Brucellosis: a re-emerging zoonosis. Vet Microbiol. 2010 Jan;140(3-4):392–8.
12 European Centre for Disease Prevention and Control. Brucellosis. ECDC. Annual epidemiological report for 2016. Stockholm:ECDC;2018. [ Links ]
13 Sousa Carvalho M, Barroso MR, Pinhal F, Mota Tavares F. Brucelose. Alguns aspectos epidemiológicos. Med Interna (Bucur). 1995;2(4):259–61.
14 Araj GF. Human brucellosis: a classical infectious disease with persistent diagnostic challenges. Clin Lab Sci. 1999 Jul-Aug;12(4):207–12.
15 Doganay M, Aygen B. Human brucellosis: an overview. Int J Infect Dis. 2003;7(3):173–82.
16 Aygen B, Doganay M, Sumerkan V, et al. Clinical manifestations, complications and treatment of brucellosis: a retrospective evaluation of 480 patients. Med Mal Infect. 2002 Sep;32(9):485–93.
17 Hasanjani Roushan MR, Mohrez M, Smailnejad Gangi SM, Soleimani Amiri MJ, Hajiahmadi M. Epidemiological features and clinical manifestations of 469 adult patients with brucellosis in Babol, Norther Iran. Epidemiol Infect. 2004 Dec;132(6):1109–14.
18 Kaya S, Elaldi N, Deveci O, Eskazan AE, Bekcibasi M, Hosoglu S. Cytopenia in adult brucellosis patients. Indian J Med Res. 2018 Jan;147(1):73–80.
19 Mangalgi S, Sajjan A. Comparison of three blood culture techniques in the diagnosis of human brucellosis. J Lab Physicians. 2014 Jan;6(1):14–7.
Statement of Ethics
The authors testify that this article is according to the World Medical Association Declaration of Helsinki. The patient has given informed consent to publish their case (including publication of images). The patient’s identity was not revealed on this case report.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Joana Rodrigues dos Santos
Serviço de Medicina I, Centro Hospitalar Universitário Lisboa Norte
Hospital de Santa Maria, Avenida Professor Egas Moniz
PT–1649-035 Lisboa (Portugal)
E-Mail joanaorsantos@gmail.com
Received: April 30, 2019; Accepted after revision: September 4, 2019














