Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.1 Lisboa fev. 2020
https://doi.org/10.1159/000499723
ENDOSCOPIC SNAPSHOT
A Case of Gastric Ischemia: Management and Prognosis
Isquemia gástrica: abordagem e prognóstico
João Carlos Silva, Adélia Rodrigues, Ana Ponte, Ana Paula Silva, João Carvalho
Department of Gastroenterology, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Ischemia, Gastric ischemia, Gastrointestinal bleeding
Palavras-chave: Isquemia, Isquemia gástrica, Hemorragia digestiva
An 85-year-old female presented to the emergency department with coffee ground emesis and abdominal pain. The patient had a medical history of diabetes mellitus, hypertension, and hip replacement 10 years before.
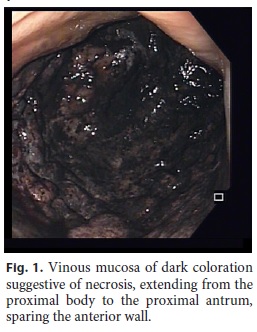
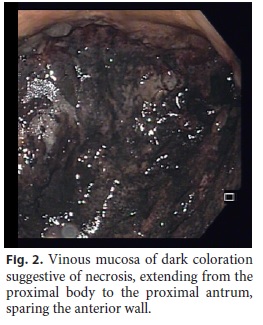
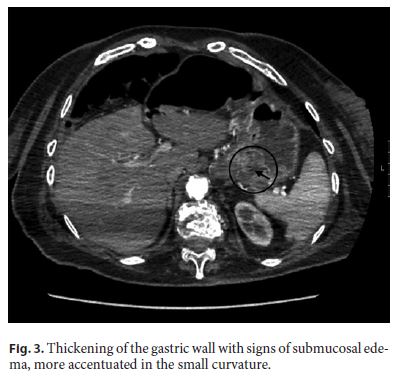
Physical examination revealed abdominal tenderness. The patient was hemodynamically stable and had no fever. The most important laboratory findings were hemoglobin 8.9 g/dL, C-reactive protein 0.03 mg/dL, and lactate dehydrogenase 177 U/L. Esophagogastroduodenoscopy revealed a vinous mucosa of dark coloration suggestive of necrosis and polypoid areas with exudate, extending from the proximal body to the proximal antrum, only sparing the anterior wall of the gastric cavity (Fig. 1, Fig. 2). Abdominal computed tomography revealed thickening of the gastric wall with signs of submucosal edema, more accentuated along the small curvature, in the region of the body, fundus, and in the cardia (Fig. 3). Histology was compatible to the endoscopic suspicion of gastric ischemia.
Considering clinical stability and the absence of complications, namely perforation, sepsis or persistent bleeding, the patient was hospitalized for medical treatment. The patient was treated with parenteral nutrition, intravenous fluids, intravenous proton pump inhibitors, and broad-spectrum antibiotics with favorable clinical outcome. Considering the favorable clinical evolution without evidence of complications, endoscopic reevaluation was not necessary. The patient was discharged after 3 weeks of medical treatment and was reevaluated at 6 months, remaining asymptomatic.
Gastric ischemia is uncommon because of the rich collateral blood supply of the stomach. It is infrequently reported in the medical literature and is likely under-recognized both clinically and histopathologically [1]. Few cases of gastric ischemia have been reported in patients with predisposing factors, such as atherosclerosis, vasculitis, paraesophageal hernia, gastric volvulus, gastric dilation, disseminated intravascular coagulation, shock, and postoperatively [2–4]. There are also reports of gastric ischemia as a complication of endoscopic procedures and secondary to hypoperfusion [2, 5]. Etiopathogenesis, clinical features, endoscopic/radiologic findings, and patient outcomes are not well known due to the rarity of this condition [2]. Patients are usually treated conservatively unless signs of perforation, sepsis, or persistent bleeding (despite endoscopic intervention) are developed, in which case gastrectomy is warranted [3]. In patients treated conservatively, hemorrhagic recurrence is low, although the mortality rate as a direct result of gastric ischemia is approximately 24% within 6 months [2].
Gastric ischemia was previously described in elderly patients of both sexes with risk factors for ischemic events. Most published cases report evidence of vascular occlusion.
In this case, it was possible to endoscopically document ischemic necrosis involving almost the entire gastric cavity in a patient with no evidence of vascular disease. The patient presented important risk factors for gastric hypoperfusion (diabetes and hypertension) in the absence of major vascular abnormalities.
This is an exemplary case of good response and 6-month survival in a patient with extensive gastric ischemic necrosis.
References
1 Tang SJ, Daram SR, Wu R, Bhaijee F. Pathogenesis, diagnosis, and management of gastric ischemia. Clin Gastroenterol Hepatol. 2014 Feb;12(2):246–52.e1. [ Links ]
2 Sharma A, Mukewar S, Chari ST, Wong Kee Song LM. Clinical Features and Outcomes of Gastric Ischemia. Dig Dis Sci. 2017 Dec;62(12):3550–6. [ Links ]
3 Saldaña Dueñas C, Elosua González A, Guerra Lacunza A. Gastric ischemia due to critical stenosis of the celiac trunk. An Sist Sanit Navar. 2018 Apr;41(1):123–7. [ Links ]
4 Ahmad DS, Sahak K, Lazenby AJ, Bhat I. Chronic mesenteric ischemia and gastric ischemia: a bad combination. Gastrointest Endosc. 2017 Sep;86(3):564–5. [ Links ]
5 Papanikolaou IS, Foukas PG, Sioulas A, Beintaris I, Panagopoulos P, et all. A case of gastric ischemic necrosis. Endoscopy [Internet]. 2011;43:E342. [ Links ]
Statement of Ethics
Informed consent was obtained from the patient.
Disclosure Statement
The authors declare no conflicts of interest for this article.
Funding Sources
Grant support was not provided for this article.
* Corresponding author.
João Carlos Silva
Department of Gastroenterology, Centro Hospitalar Vila Nova de Gaia/Espinho, Rua Conceição Fernandes
PT–4434-502 Vila Nova de Gaia (Portugal)
E-Mail joaocarosilva@gmail.com
Received: November 8, 2018; Accepted after revision: March 14, 2019
Author Contributions
João Carlos Silva: Composition and drafting of the article. Evaluation of the patient at admission, endoscopic study, and hospital admission.
Adélia Rodrigues: Evaluation of the patient at admission, endoscopic study, and hospital admission.
Ana Ponte: Critical revision of the article for important intellectual content.
Ana Paula Silva: Critical revision of the article for important intellectual content.
João Carvalho: Critical revision of the article for important intellectual content.














