Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.5 Lisboa out. 2019
https://doi.org/10.1159/000494570
ENDOSCOPIC SNAPSHOT
Fish-Eye Ampulla: A Rare Pathognomonic Sign
Ampola Fish-Eye: um sinal patognomónico raro
Jaime Pereira Rodriguesa, Sónia Fernandesa, Luísa Proençaa, João Carvalhoa
aGastroenterology Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Endoscopy, Endoscopic ultrasonography, Pancreas, Fish-eye ampulla, IPMN
Palavras-Chave: Endoscopia, Ecoendoscopia, Pâncreas, Ampola fish-eye, IPMN
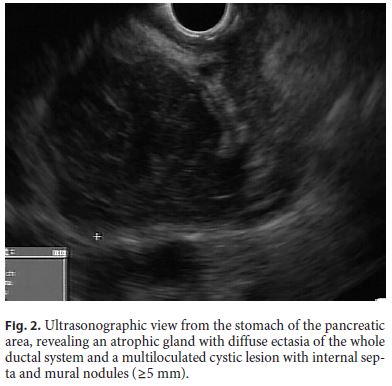
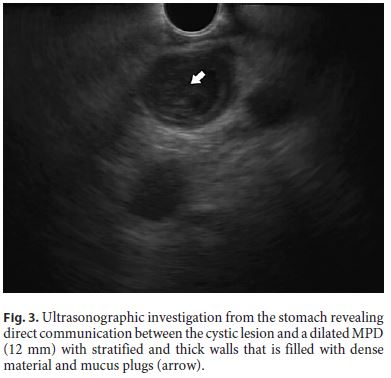
A 74-year-old female patient with no relevant personal or family medical history was referred to our department for reevaluation of a pancreatic cystic lesion detected on a computed tomography scan performed for weight loss and fatigue. Physical examination and laboratory results were unremarkable. Magnetic resonance cholangiopancreatography evidenced an atrophic pancreas with a multiloculated cystic lesion (7.2 × 6.5 cm) with internal septa in the head, accompanied by diffuse main pancreatic duct (MPD) dilatation. Endoscopic ultrasonography was subsequently performed. Endoscopic visualization revealed a patulous major papilla, actively extruding thick mucus, the fish-eye sign Fig. 1a, b). Ultrasonographic evaluation confirmed the previous findings, specifically an atrophic pancreas with diffuse ectasia of the whole ductal system and a multiloculated cystic lesion (Fig. 2) with internal septa and mural nodules (=5 mm). The lesion was in direct communication with a dilated MPD (12 mm), which had stratified and thick walls and was filled with dense material and mucus plugs (Fig. 3, arrow). The overall findings were diagnostic of a mixed-type intraductal papillary mucinous neoplasm (IPMN) with highrisk features. Surgical treatment was proposed, but the patient refused and chose to be maintained on regular surveillance.
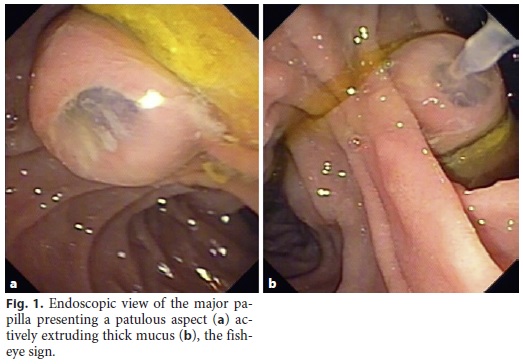
In the past few years, the improved and expanded use of several diagnostic tests, mainly computed tomography and magnetic resonance imaging, led to a surge of interest on pancreatic cystic lesions, including IPMN [1, 2]. Currently, most patients diagnosed with IPMN are asymptomatic and are detected by examinations performed for unrelated problems [2]. The final diagnosis of IPMN is normally achieved by a combination of endoscopic, radiologic, pathological and/or molecular findings [2]. Endoscopically, a diagnosis of IPMN can be established if a patulous papilla with mucin extrusion, referred as the fish-eye ampulla, is visualized. This sign, although rarely present, is pathognomonic for IPMN of the pancreas [3–5]. Taking into the account the high frequency of highgrade dysplasia and invasive carcinoma in main duct IPMN, surgical resection is strongly recommended for all surgically fit patients with MPD > 10 mm, jaundice, or mural nodules [1]. Regarding mixed-type IPMN, clinical and biological characteristics are identical to those of main duct IPMN, so their management is classically based on a similar algorithm [1, 5]. In this context, and according to its high specificity, whenever the fish-eye sign is identified, surgical referral should not be delayed in patients fit for surgery.
References
1 Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017 Sep - Oct;17(5):738–53. [ Links ]
2 Castillo CF. Intraductal papillary mucinous neoplasms of the pancreas: a plea for prospective differentiation between main-duct and side-branch tumors. Ann Surg Oncol. 2005 Feb;12(2):98–9. [ Links ]
3 Asokkumar R, Chin YK. Fish-Mouth Papilla. Clin Gastroenterol Hepatol. 2018 Sep;16(9):A34. [ Links ]
4 Hutchins GF, Draganov PV. Cystic neoplasms of the pancreas: a diagnostic challenge. World J Gastroenterol. 2009 Jan;15(1):48–54. [ Links ]
5 Castellano-Megías VM, Andrés CI, López-Alonso G, Colina-Ruizdelgado F. Pathological features and diagnosis of intraductal papillary mucinous neoplasm of the pancreas. World J Gastrointest Oncol. 2014 Sep;6(9):311–24. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors do not have any interest that might be interpreted as influential in this report. This report did not receive any support from corporations, neither industrial nor private.
* Corresponding author.
Jaime Pereira Rodrigues
Centro Hospitalar Vila Nova de Gaia/Espinho, Gastroenterology Department
Rua Conceição Fernandes
PT–4434-502 Vila Nova de Gaia (Portugal)
E-Mail jaimepereirarodrigues@gmail.com
Received: September 20, 2018; Accepted after revision: October 14, 2018














