Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.4 Lisboa ago. 2019
https://doi.org/10.1159/000493352
ENDOSCOPIC SNAPSHOT
Going through the Mesh: Argon Plasma Trimming of a Metal Biliary Stent
Atravessando a Malha: Destruição parcial de prótese biliar metálica com Árgon-Plasma
Richard Azevedoa,b, Diogo Libânioa, Pedro Bastosa, Mário Dinis Ribeiroa, Catarina Brandãoa
aGastroenterology Department, Instituto Português de Oncologia do Porto Francisco Gentil, Porto, Portugal; bGastroenterology Department, Amato Lusitano Hospital, Castelo Branco, Portugal
* Corresponding author.
Keywords: Biliary metal stent, Adverse event, Migration, Argon plasma coagulation, Trimming
Palavras-Chave: Prótese biliar metálica, Evento adverso, Migração, Coagulação árgon-plasma, Destruição parcial
Stent migration is a rare cause of biliary stent dysfunction. We present the case of a 63-year-old male with obstructive jaundice due to a stage IV pancreatic ductal adenocarcinoma. As endoscopic biliary cannulation had been attempted without success, a percutaneous transhepatic biliary access with insertion of an uncovered 60 × 10 mm self-expandable metal stent (Wallstent®, Billiary; Boston Scientific) was performed. Six months later, the patient was admitted due to recurrent vomiting and acute cholangitis (abdominal pain, fever, and jaundice; total bilirubin 2.86 mg/dL, direct 1.55 mg/dL). Abdominal ultrasound revealed dilatation of the intrahepatic bile ducts as well as parietal thickening and dilatation of the common bile duct upstream the proximal end of the stent.
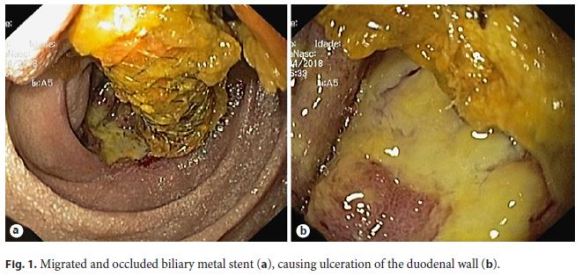
Given the high index of suspicion for biliary stent dysfunction, a duodenoscopy was performed, showing distal migration of the biliary metal stent and its occlusion with debris. The distal end was impacted in the contralateral duodenal wall, causing delayed gastric emptying and mucosal ulceration (Fig. 1).
After 7 days of liquid diet, a new duodenoscopy was performed and stent removal using an endoscopic retrieval basket and a snare polypectomy was unsuccessfully attempted. The placement of another stent to relieve the obstruction was also not possible since cannulation of the biliary tree was precluded due to the impaction of the stent in the duodenal wall.
Therefore, it was decided to perform argon plasma coagulation (APC) trimming of the distal 2 cm of the stent (Fig. 2; online suppl. video; for all online suppl. material, see http://www.karger.com/doi/10.1159/000493352) using an axial probe, power setting of 120 W, and gas flow at 1 L/ min (APC unit VIO 300S, ERBE®). The procedure took 15 min, without immediate complications.

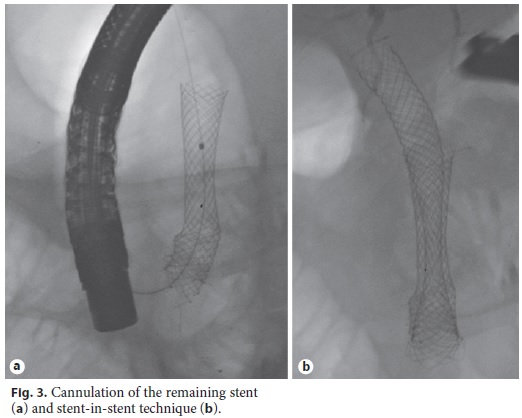
After removal of the trimmed stent with a polypectomy snare, biliary cannulation and subsequent cholangiogram were successfully performed, revealing stenosis of the distal common bile duct. A stent-in-stent technique was then performed with insertion of an uncovered 60 × 10 mm self-expandable metal stent (WallflexTM Biliary; Boston Scientific).
Fluoroscopy and endoscopy confirmed the correct positioning of the stent (Fig. 3).
The patient was discharged after 4 days with complete resolution of cholangitis. Two months after the procedure, he remains asymptomatic and with normal serum bilirubin levels.
Endoscopic stent placement is an established therapeutic option for the palliation of unresectable malignant biliary strictures [1]. Metal stents are generally preferred in patients with expected survival higher than 3 months, although dysfunction still occurs in 20–27% of the patients [2]. Migration, which may occur in 1% [2], causes reocclusion of the biliary tree, duodenal mucosal ulceration, bleeding, and gastrointestinal tract perforation [3]. No standard strategy for the management of migrated metal stents has been established [1], and the removal of uncovered metal stents by simple traction is often impossible due to the embedment of the metal mesh in the biliary wall. Stent trimming with APC was first described in 2001 [4] and has been reported to be a safe, useful, and a technically feasible therapeutic approach [1, 5]. Although few cases are described [5], no standardized parameters for the power setting and gas flow of APC have been established in the literature: the reported power settings ranged from 60 to 85 W, and gas flow from 0.8 to 2L/min, showing great variability between studies [3]. In the case presented herein, we adopted parameters based on the settings described in other reported cases [3] and adjusted them to our personal perception of the effectiveness and safety of trimming at the time of the procedure. With a slightly higher power setting (120 W), the trimming could be done adequately and safely without any major complications.
This case highlights the safety and feasibility of APC stent trimming to solve local complications of a migrated metal stent and to restore endoscopic access to the biliary tree.
References
1 Ito K, Ogawa T, Horaguchi J, Koshita S, Fujita N: Reintervention for occluded biliary metal stent for patients with malignant distal biliary stricture. Dig Endosc 2013;25 Suppl 2:126–131. [ Links ]
2 Dumonceau J-M, Tringali A, Blero D, et al: Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012;44:277–298. [ Links ]
3 Ishii K, Itoi T, Sofuni A, et al: Endoscopic removal and trimming of distal self-expandable metallic biliary stents. World J Gastroenterol 2011;17:2652–2657. [ Links ]
4 Demarquay JF, Dumas R, Peten EP, Rampal P: Argon plasma endoscopic section of biliary metallic prostheses. Endoscopy 2001;33:289–290. [ Links ]
5 Vanbiervliet G, Piche T, Caroli-Bosc FX, et al: Endoscopic argon plasma trimming of biliary and gastrointestinal metallic stents. Endoscopy 2005;37:434-438. [ Links ]
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
* Corresponding author.
Richard Azevedo, MD
Gastroenterology Department, Amato Lusitano Hospital
Avenida Pedro Álvares Cabral
PT–6000-085 Castelo Branco (Portugal)
E-Mail richardazevedo13@gmail.com
Received: July 18, 2018; Accepted after revision: August 27, 2018














