Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.4 Lisboa Aug. 2019
https://doi.org/10.1159/000493350
CLINICAL CASE STUDY
Hepatosplenic T-Cell Lymphoma: A Rare Complication of Monotherapy with Thiopurines in Crohns Disease
Linfoma T Hepatoesplénico: Uma Complicação Rara da Monoterapia com Tiopurinas na Doença de Crohn
Joana Carvãoa, Vítor Magno Pereiraa, Fernando Jacintob, Carla Sousa Andradea, Luís Jasminsa
aGastroenterology Department, Hospital Central do Funchal, Funchal, Portugal; bHemato-Oncology Department, Hospital Central do Funchal, Funchal, Portugal
* Corresponding author.
ABSTRACT
Hepatosplenic T-cell lymphoma (HSTCL) is an extremely rare and aggressive form of non-Hodgkin lymphoma associated with poor response to treatment and high mortality. There is an increased incidence among patients with inflammatory bowel disease, especially young male patients under 35 years old and on combination therapy (thiopurine and antiTNF-α). We describe a case of HSTCL in a young male patient with stenosing ileal Crohns disease on azathioprine monotherapy for 4.8 years admitted to our hospital with intra- abdominal sepsis. Despite chemotherapy, the patient eventually died 1 month after the diagnosis. Through a literature review, we identified 18 additional cases of HSTCL in Crohns disease patients that had only been treated with thiopurine monotherapy. The authors intend to highlight the rarity of this diagnosis especially with azathioprine monotherapy and the diagnostic challenge in a case that presented with intra-abdominal sepsis.
Keywords: Hepatosplenic T-cell lymphoma, Crohns disease, Thiopurines
RESUMO
O linfoma de células T hepatoesplénico é um tipo raro e agressivo de linfoma não Hodgkin associado a fraca reposta à terapêutica e elevada mortalidade. A sua incidência está aumentada em doentes com doença inflamatória intestinal, particularmente jovens com menos de 35 anos, do sexo masculino e em terapêutica combinada com tiopurinas e inibidores TNF-α. Apresentamos o caso de um linfoma T hepatoesplénico num homem jovem com doença de Crohn ileal estenosante sob monoterapia com azatioprina há 4,8 anos, admitido no nosso hospital num contexto de sépsis de ponto de partida intraabdominal. Apesar da quimioterapia o doente acabou por falecer 1 mês após o diagnóstico. Numa revisão da literatura, os autores identificaram 18 casos adicionais de linfoma T hepatosplénico em doentes com doença de Crohn tratados apenas com tiopurinas em monoterapia. Os autores pretendem destacar a raridade do diagnóstico, especialmente no contexto de azatioprina em monoterapia e o desafio diagnóstico num caso que se apresentou com sépsis intra-abdominal.
Palavras-Chave: Linfoma T hepatoesplénico, Doença de Crohn, Tiopurinas
Introduction
Hepatosplenic T-cell lymphoma (HSTCL) is a very rare (< 1%) and aggressive peripheral T-cell non-Hodgkin lymphoma [1]. Even though the majority of cases arise de novo, approximately 30% of cases occur in the setting of chronic immunosuppression and chronic antigen stimulation, as is the case in inflammatory bowel disease (IBD) [2]. Young men under 35 years with Crohns disease who are treated with thiopurines and anti-TNF for at least 2 years are at higher risk [1].
We report the case of a 25-year-old male with a 5-year history of stenosing ileal Crohns disease on azathioprine monotherapy for 4.8 years and the challenging diagnosis of HSTCL in the setting of intra-abdominal sepsis.
Case Presentation
The subject of this report is a 25-year-old leukodermic male with a diagnosis of stenosing ileal Crohns disease for 5 years (A2 L1 B2 in the Montreal classification). He had a surgical history of a stricturoplasty and segmental enterectomy for a stenosis in 2012 without complications.
The patient had been treated with azathioprine (2.5 mg/kg) for 4.8 years. Prior to initiation of thiopurines, the patient was submitted to EBV screening, which revealed that the patient was immune to EBV (IgG positive, IgM negative). He had also previously taken iron and vitamin B12 supplementation. No other personal, relevant background, medical, or family history was found. On his last medical appointment, before hospital admission, the patient had been asymptomatic and the blood tests had been normal. His last ileocolonoscopy (1 month prior to admission) had demonstrated a small ulceration in the ileocecal valve, and the patient had been started on mesalamine 3 g/day plus budesonide 9 mg/day.
The patient presented to the emergency department with a 7-day history of fever and unspecific lower abdominal pain. On physical examination, he was febrile (39ºC) and polypneic and had a blood pressure of 117/70 mm Hg and a heart rate of 60 bpm. Abdominal examination showed tenderness in his lower right abdomen and splenomegaly, but there were no signs of peritoneal irritation. No lymphadenopathies were noted. A complete blood count revealed a normal white blood cell count, anemia (9.4 g/dL), and thrombocytopenia (136,000 µL). Blood chemistry showed elevated C-reactive protein (75.10 mg/dL) and lactate dehydrogenase (LDH) (2,177 U/L). Levels of liver transaminase, bilirubin, urea, and creatinine were normal.
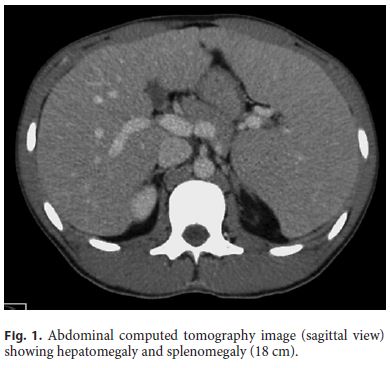
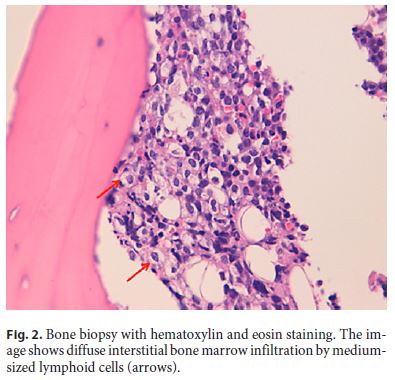
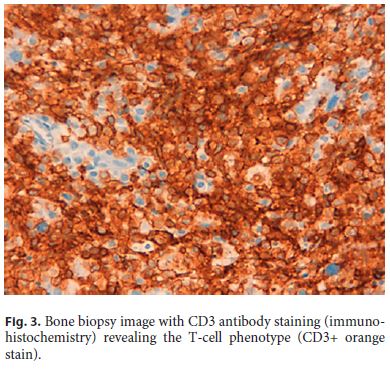
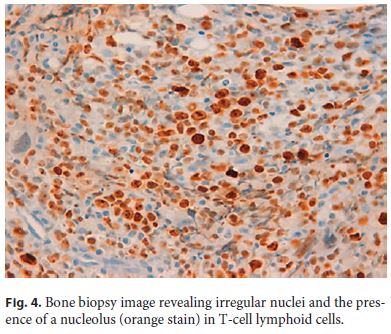
An abdominal computed tomography scan revealed hepatomegaly, splenomegaly (Fig. 1) with infarct, and a 5-cm abscess adjacent to a small bowel surgical suture. No lymphadenopathies were evident. The patient then underwent surgical drainage of the abscess without immediate postoperative complications. Four days after the surgery, the patient was admitted to the intensive care unit with septic shock and multiorgan dysfunction (hematological, renal, hepatic, and respiratory) due to infection of his surgical wound with methicillin-resistant Staphylococcus aureus. Despite directed antibiotic therapy, the patients clinical condition did not improve and he remained febrile with bicytopenia (hemoglobin 6.9 g/dL, platelets 108,000/µL), elevated C-reactive protein levels (164 mg/dL), elevation of aminotransferases (AST 95 U/L, ALT 202 U/L) and LDH (7,472 U/L), hypoalbuminemia (24 g/L), hyperbilirubinemia (3.53 mg/dL), hypertriglyceridemia (247 mg/ dL), hyperferritinemia (> 7,500 ng/mL), and β2-microglobulin (4.94 mg/L). A bone marrow biopsy showed diffuse interstitial infiltration by medium-sized lymphoid cells of the T-cell phenotype (CD3+) with irregular nuclei and presence of a nucleolus (Fig. 2, Fig. 3, Fig. 4). Flow cytometry showed expression of CD2, CD3, CD7, and T-cell receptor-γ/δ. Together, these findings were consistent with γ/δHSTCL.
After resolution of the infectious state, the patient underwent 2 cycles of chemotherapy with cyclophosphamide, hydroxydaunorubicin, vincristine, and prednisolone (CHOP) with no response. A second line of chemotherapy with etoposide, cisplatin, cytarabine, and methylprednisolone (ESHAP) was started, but the patient eventually died as a result of severe bleeding complications only 1 month after the diagnosis.
Discussion
The diagnosis of HSTCL in Crohns disease may be challenging due to the overlap of manifestations of both conditions, especially in immunosuppressed patients. In our case, the diagnosis was further delayed due to the concomitant presentation of sepsis. Until the diagnosis of HSTCL, the patients fever, bicytopenia, and splenomegaly (and infarct) were initially interpreted as related to the septicemia. These findings could also explain high LDH levels. A high level of suspicion is therefore needed in this subset of patients.
We searched the PubMed database using the terms hepatosplenic T-cell lymphoma, inflammatory bowel disease, and Crohns disease. We also reviewed the bibliographies of the most relevant articles.
Including our case, we identified 19 cases of HSTCL in Crohns disease that had only been treated with thiopurines in monotherapy (anti-TNF-naïve patients) (Table 1) [3–13]. Of the 19 patients, 15 were men (79%), 2 were women, and 2 were not specified (NS). The median age at diagnosis was 23.5 years (range 13–72). Of the 10 cases that reported the duration of thiopurine therapy before HSTCL, the median treatment duration was 5 years (range < 1 to 8). Presenting clinical features were specified for 11 patients. Splenomegaly was the most dominant clinical feature, present in all 11 patients (7 also had hepatomegaly), followed by constitutional symptoms (fever, fatigue, and night sweats), which were present in 8 patients (73%). Of the 11 cases, only 7 had reported blood counts, and all presented with cytopenia. Thrombocytopenia was present in all patients, followed by anemia (86%) and leukopenia (71%). Treatment options were available for 16 patients. Different chemotherapy modalities were used aiming for a curative allogenic stem cell transplant; however, due to the fast and aggressive course of the disease, the overall survival rate was very low. An exception is a unique case of a 27-year-old female with Crohns disease on thiopurine for 5 years who was treated for 9 months with interferon-α monotherapy and achieved a 20-month follow-up remission free. In our case, the therapeutic options were remarkably limited due to the patients poor condition and severe cytopenia.
There has been some debate as to whether IBD, by itself, could potentially increase the risk of lymphomas, more specifically of HSTCL. It has been speculated that in HSTCL, underlying immunodysregulatory disorders could lead to excessive antigenic stimulation of γδ T cells and polyclonal γδ T-cell expansion. Further transforming genetic events could culminate in HSTCL [3]. However, no cases of HSTCL in IBD therapy-naïve patients have been reported in the literature [14].
It is well established by now that there is a higher risk of lymphoma in IBD patients on thiopurines [15]. Following absorption, their metabolite – 6-thioguanine – accumulates in bone marrow, immune cells (such as lymphocytes), and epithelial tissue, where they inhibit purine synthesis, cause DNA and RNA damage, and eventually lead to malignant proliferation [16]. Although this cytotoxic effect has been thought to be the main carcinogenic pathway, a thiopurine-specific contribution has been postulated [17].
In a cross-sectional study, there was in vivo evidence that chronic thiopurine treatment was associated with a dose-dependent increase in the frequency of somatic mutations in tissue with a high accumulation of 6-thioguanine [17]. Also, cytogenic changes have been reported in a dose-dependent manner with thiopurines, more specifically with chromosome 7. In a systematic review of cytogenic changes in HSTCL patients with IBD, alterations of isochromosome 7q, aberrations of chromosomes 8 and 13, and deletion of the Y chromosome were found [18]. The last finding is of particular interest, since HSTCL predominantly affects male patients.
The largest population-based cohort study on thiopurine use and lymphoproliferative disorders in IBD patients showed that patients who received thiopurines were 5 times more likely to develop a lymphoproliferative disorder [19]. These findings were also validated in a recent meta-analysis that included 8 population-based studies and 10 referral studies [20]. Combination therapy with anti-TNF further raises the HSTCL risk [15]. In men younger than 35 years, where the risk seems higher, as with our case, the absolute risk is estimated to be 1: 7,404 on monotherapy with thiopurine and 1: 3,534 on combination therapy, with 80% of the cases occurring after 2 years of combination therapy [1]. These findings support the current recommendations to limit the duration of combined treatment to 2 years for young males [15]. No formal recommendations regarding duration limitation of monotherapy with azathioprine exist for this subgroup of patients, even though awareness regarding therapies longer than 1 year has been advised [1].
Conclusions
With this case report, the authors intended to highlight the rarity of this diagnosis, especially for patients on monotherapy with azathioprine, as well as the diagnostic challenge in a patient that presented with intra-abdominal sepsis. Further understanding of the mechanisms that lead to HSTCL might be helpful to minimize the risks of this malignancy in IBD patients.
References
1 Kotlyar DS, Osterman MT, Diamond RH, et al: A systematic review of factors that contribute to hepatosplenic T-cell lymphoma in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2011;9:36–41. [ Links ]
2 Thai A, Prindiville T: Hepatosplenic T-cell lymphoma and inflammatory bowel disease. J Crohns Colitis 2010;4:511–522. [ Links ]
3 Yabe M, Medeiros LJ, Daneshbod Y, et al: Hepatosplenic T-cell lymphoma arising in patients with immunodysregulatory disorders: a study of 7 patients who did not receive tumor necrosis factor-α inhibitor therapy and literature review. Ann Diagn Pathol 2017;26:16–22. [ Links ]
4 Baić Kinda S, Duraković N, Dotlić S, et al: Hepatosplenic αβ T-cell lymphoma arising after long-term azathioprine therapy successfully treated with allogeneic bone marrow transplant. Leuk Lymphoma 2013;54:1334–1335. [ Links ]
5 Subramaniam K, Yeung D, Grimpen F, et al: Hepatosplenic T-cell lymphoma, immunosuppressive agents and biologicals: what are the risks? Intern Med J 2014;44:287–290. [ Links ]
6 Selvaraj SA, Chairez E, Wilson LM, et al: Use of case reports and the Adverse Event Reporting System in systematic reviews: overcoming barriers to assess the link between Crohns disease medications and hepatosplenic T-cell lymphoma. Syst Rev 2013;2:53. [ Links ]
7 Ochenrider MG, Patterson DJ, Aboulafia DM: Hepatosplenic T-cell lymphoma in a young man with Crohns disease: case report and literature review. Clin Lymphoma Myeloma Leuk 2010;10:144–148. [ Links ]
8 Fowler S, Beyak M, Depew WT, et al: W1212 hepatosplenic T-cell lymphoma in Crohns disease. Where does the risk lie? Gastroenterology 2010;138(suppl 1):S-675. [ Links ]
9 Mittal S, Milner BJ, Johnston PW, Culligan DJ: A case of hepatosplenic γδ T-cell lymphoma with a transient response to fludarabine and alemtuzumab. Eur J Haematol 2006;76:531–534. [ Links ]
10 Humphreys MR, Cino M, Quirt I, et al: Longterm survival in two patients with hepatosplenic T cell lymphoma treated with interferon-alpha. Leuk Lymphoma 2008;49:1420–1423. [ Links ]
11 Falchook GS, Vega F, Dang NH, et al: Hepatosplenic gamma-delta T-cell lymphoma: clinicopathological features and treatment. Ann Oncol 2009;20:1080–1085. [ Links ]
12 Navarro JT, Ribera JM, Mate JL, et al: Hepatosplenic T-gammadelta lymphoma in a patient with Crohns disease treated with azathioprine. Leuk Lymphoma 2003;44:531–533. [ Links ]
13 Lémann M, Gérard de La Valussière F, Bouhnik Y, et al: Intravenous cyclosporine for refractory attacks of Crohns disease (CD): long-term follow-up of patients. Gastroenterology 1998;114:A1020. [ Links ]
14 Sifuentes H, Kane S: Monitoring for extra- intestinal cancers in IBD. Curr Gastroenterol Rep 2015;17:42. [ Links ]
15 Annese V, Beaugerie L, Egan L, et al: European evidence-based consensus: inflammatory bowel disease and malignancies. J Crohns Colitis 2015;9:945–965. [ Links ]
16 A-Rahim YI, Farrell RJ: Overview of azathioprine and mercaptopurine use in inflammatory bowel disease. Uptodate 2017. https://www.uptodate.com/contents/overview-ofazathioprine-and-mercaptopurine-use-ininflammatory-bowel-disease. [ Links ]
17 Nguyen T, Vacek PM, ONeill P, et al: Mutagenicity and potential carcinogenicity of thiopurine treatment in patients with inflammatory bowel disease. Cancer Res 2009;69:7004–7012. [ Links ]
18 Kotlyar DS, Blonski W, Diamond RH, et al: Hepatosplenic T-cell lymphoma in inflammatory bowel disease: a possible thiopurineinduced chromosomal abnormality. Am J Gastroenterol 2010;105:2299–2301. [ Links ]
19 Beaugerie L, Brousse N, Bouvier AM, et al: Lymphoproliferative disorders in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Lancet 2009;374:1617–1625. [ Links ]
20 Kotlyar DS, Lewis JD, Beaugerie L, et al: Risk of lymphoma in patients with inflammatory bowel disease treated with azathioprine and 6-mercaptopurine: a meta-analysis. Clin Gastroenterol Hepatol 2015;13:847–858.e4. [ Links ]
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding Sources
No subsidies or grants contributed to this work.
* Corresponding author.
Joana Carvão
Gastroenterology Department, Hospital Central do Funchal
Avenida Luís de Camões nº 57 PT–9004-514 Funchal (Portugal)
E-Mail joanacarvao@hotmail.com
Received: June 16, 2018; Accepted after revision: August 27, 2018
Acknowledgments
We would like to graciously acknowledge Michelle Cordeiro for providing the pathological images.














