Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.3 Lisboa jun. 2019
https://doi.org/10.1159/000490922
ENDOSCOPIC SNAPSHOT
Avoiding Stent-in-Stent Retrieval Strategy for Partially Covered Stents in Anastomotic Leakages: An Innovative Approach
Evitando a estratégia de remoção “stent-in-stent” para próteses parcialmente cobertas em deiscências de anastomoses: uma abordagem inovadora
Gonçalo Nunesa, Marta Patitaa, Pedro Pinto-Marquesa,b
aGastroenterology Department, Hospital Garcia de Orta, Almada, Portugal; bGastroenterology Department, Hospital da Luz, Lisbon, Portugal
* Corresponding author.
Keywords: Anastomotic leakage, Dehiscence, Self-expandable metal stent
Palavras-Chave: Anastomose, Deiscência, Prótese metálica autoexpansível
Anastomotic leakage is still one of the most feared surgical complications with an incidence of 3–25% [1]. The endoscopic placement of self-expanded metallic esophageal stents has become the preferred primary treatment with an 85% clinical success [2]. Fully covered metal stents (FCMS) are prone to migration due to its reduced anchoring capacity and partially covered metal stents (PCMS) cause tissue ingrowth as early as 1 week after placement, impairing its removal with risk of bleeding and perforation [2]. The stent-in-stent technique requires placement of an FCMS inside the PCMS during 10–14 days to induce pressure necrosis of the overgrowing and ingrowing mucosa, allowing further safe removal [3].
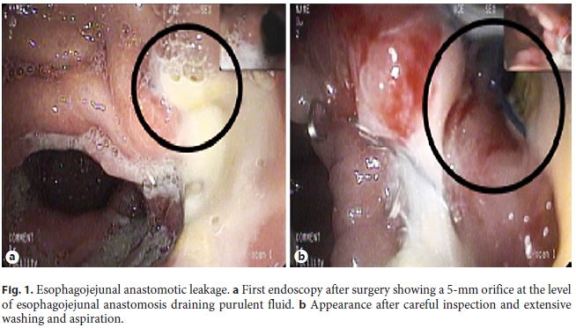
An 82-year-old woman previously submitted to total gastrectomy due to gastric adenocarcinoma was newly diagnosed with a colorectal adenocarcinoma. A left hemicolectomy was performed but an incidental laceration of a proximal jejunal loop complicated the procedure and a new esophagojejunal anastomosis had to be accomplished. Few days after surgery, signs of sepsis developed and an esophagojejunal anastomosis leakage was confirmed. Gastroenterology consultation was requested for stent placement. In the upper gastrointestinal endoscopy, a 5-mm orifice with a milky draining fluid was detected 32 cm from the incisors. A PCMS 23 × 120 mm was placed and fixed with endoscopic clips after extensive cauterization of the tissue surrounding the fistula orifice (Fig. 1). Two weeks later, a follow-up outpatient endoscopy showed a 2-cm distal migration, albeit the orifice was still covered. Overgrowing tissue was present but the stent could be easily repositioned. The stent remained in place for two additional weeks and later was easily removed without complications. The orifice was completely sealed at this time and the patient remained asymptomatic (Fig. 2).
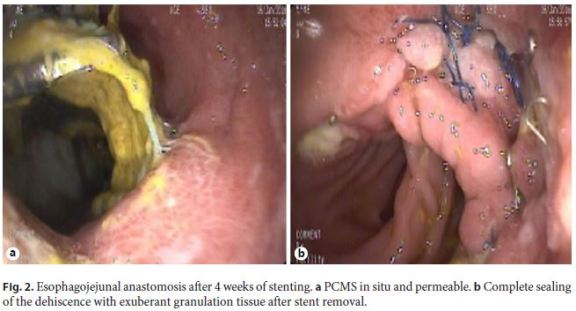
Anastomotic leakages are associated with high mortality. A conservative approach with stent placement avoids surgical re-intervention. Although the stenting period should be individualized, 6–8 weeks is the period described for an effective sealing in most studies [3]. In the present report, an innovative approach to manage anastomotic leakages, not previously reported in the literature, is exemplified as an alternative to the stent-in-stent technique when PCMS are applied. This strategy was developed after the incidental stent migration observed in this patient and taking into account the obtained good results. The authors propose PCMS placement in patients with upper gastrointestinal anastomotic leakage leaving the stent for 2 weeks. Endoscopy should be repeated at this time and the stent moved a few centimeters proximally to avoid extensive ingrowth/overgrowth through the mesh. These steps should be repeated every 2 weeks until 6–8 weeks, the mean time described for successful sealing of most dehiscences. This simple and safe approach may be more convenient to patients and medical staff, avoiding the risks and cost of placing a new stent and being less time-consuming and easily performed by all endoscopists even by those who are not completely trained with fluoroscopic equipment. Further studies are desirable to confirm the cost-effectiveness of this method.
References
1 Persson S, Rouvelas I, Kumagai K, et al: Treatment of esophageal anastomotic leakage with self-expanding metal stents: analysis of risk factors for treatment failure. Endosc Int Open 2016;4:E420–E426. [ Links ]
2 van Boeckel PG, Sijbring A, Vleggaar FP, et al: Systematic review: temporary stent placement for benign rupture or anastomotic leak of the oesophagus. Aliment Pharmacol Ther 2011;33:1292–1301. [ Links ]
3 Spaander MC, Baron TH, Siersema PD, et al: Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016;48:939–948. [ Links ]
Disclosure Statement
There are no conflicts of interest regarding this paper and its publication.
* Corresponding author.
Dr. Gonçalo Nunes
Gastroenterology Department, Hospital Garcia de Orta
Av. Torrado da Silva PT–2805-267 Almada (Portugal)
E-Mail goncalo.n@hotmail.com
Received: May 1, 2018; Accepted after revision: June 1, 2018














