Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa abr. 2019
https://doi.org/10.1159/000488741
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Symptomatic Duodenal Duplication Cyst Treated Endoscopically
Quisto duodenal sintomático – tratamento endoscópico
Mafalda Sousa, Luísa Proença, Sónia Fernandes
Centro Hospitalar de Vila Nova de Gaia e Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Duodenal duplication cyst, Endoscopic ultrasound, Therapeutic endoscopy
Palavras-Chave: Quisto duplicação duodenal, Ecoendoscopia, Endoscopia terapêutica
A 21-year-old woman with no past relevant clinical history was admitted to the emergency department for acute abdominal pain. Physical examination revealed normal blood pressure, pulse and temperature with mild epigastric tenderness. Laboratory tests showed leukocytosis (16.35 × 103 /μL) and elevated C-reactive protein (20.53 mg/dL) with normal cholestasis and pancreatic tests. An ultrasound and subsequently a computed tomography scan showed a duodenopancreatic cystic inflammatory lesion with 30 × 24 mm in the third portion of the duodenum with edema of the surrounding mucosa and fat. The common bile and pancreatic duct were normal. Antibiotics were initiated and she was discharged asymptomatic after 13 days.
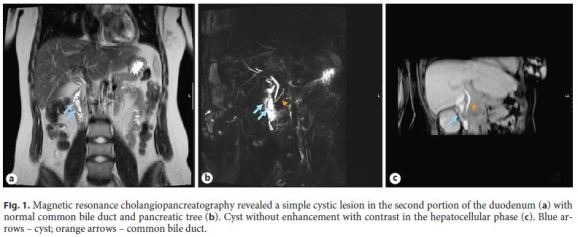
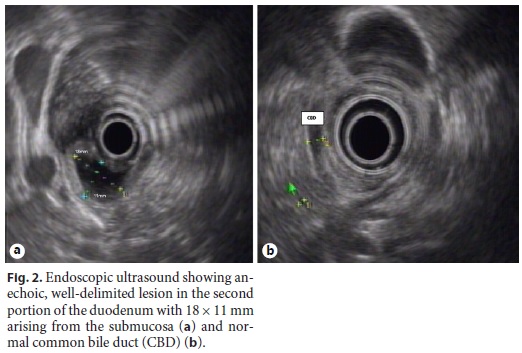
To clarify the diagnosis, a magnetic resonance cholangiopancreatography revealed a simple cystic lesion in the second portion of the duodenum without enhancement with contrast in the hepatocellular phase (Fig. 1) and endoscopic ultrasound showed a subepithelial anechoic, well-delimited lesion in the second portion of the duodenum with 18 × 11 mm arising from the submucosa (Fig. 2), compatible with duodenal duplication cyst. The papilla of Vater was in the base of the lesion and the biliary and pancreatic tree were normal with no communication with the cyst. After multidisciplinary discussion, it was decided to provide endoscopic treatment, which was performed 3 months after the acute episode. The patient was submitted to endoscopically guided fenestration by performing an incision of the cyst with a Mori knife (Fig. 3). A guidewire was placed into the cyst and the cyst wall was deroofed using a sphincterotome. The opening was further widened with a balloon with drainage of transparent fluid.
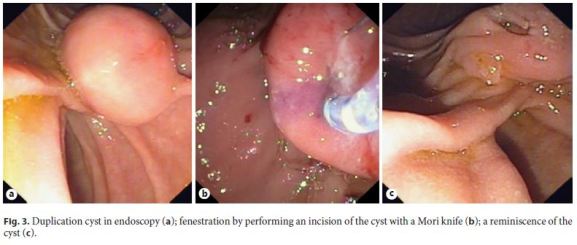
The patient remains asymptomatic after 6 months of follow-up and a reminiscence of the cyst was observed in endoscopy.
Duodenal duplication cysts are rare and usually asymptomatic and incidentally discovered. Cyst infection has been described in few cases [1, 2]. Symptomatic duodenal duplication cyst generally mandates treatment [3]. Surgical therapy is associated with significant morbimortality, so, if possible, endoscopic treatment should be preferred since it is safe and effective [1, 2, 4].
References
1 Roy Liu R, Adler D: Duplication cysts: diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound 2014;3:152–160. [ Links ]
2 Gjeorgjievski M, Manickam P, Ghaith G, Cappell MS: Safety and efficacy of endoscopic therapy for nonmalignant duodenal duplication cysts: case report and comprehensive review of 28 cases reported in the literature. Medicine (Baltimore) 2016;95:e3799. [ Links ]
3 Johnson E, Gopal D: Endoscopic management of symptomatic duodenal duplication cyst. Gastrointest Endosc 2015;82:172. [ Links ]
4 Adler D, Liu R: Duplication cysts: diagnosis, management and role of endoscopic ultrasound. Endosc Ultrasound 2014;3:152–160. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Mafalda Sousa
Centro Hospitalar de Vila Nova de Gaia e Espinho, Vila Nova de Gaia
Rua Conceição Fernandes, s/n
PT–4434-502 Vila Nova de Gaia (Portugal)
E-Mail mafalda_m_p_sousa@hotmail.com
Received: January 3, 2018; Accepted after revision: March 18, 2018














