Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa abr. 2019
https://doi.org/10.1159/000487819
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Endoscopic Management of a Rare Entity: Gastric Calcifying Fibrous Tumor
Tratamento endoscópico de uma entidade rara: tumor fibroso calcificante do estômago
Jaime P. Rodriguesa, Rolando Pinhoa, David Tenteb
aGastroenterology Department, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal; bPathology Department. Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Calcifying fibrous tumor, Submucosal tumor, Stomach,·Endoscopic mucosal resection
Palavras-Chave: Tumor fibrose calcificante, Lesão subepitelial, Estômago, Resseção endoscópica da mucosa
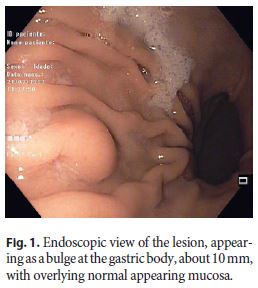
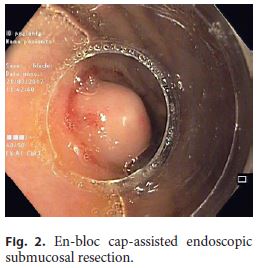
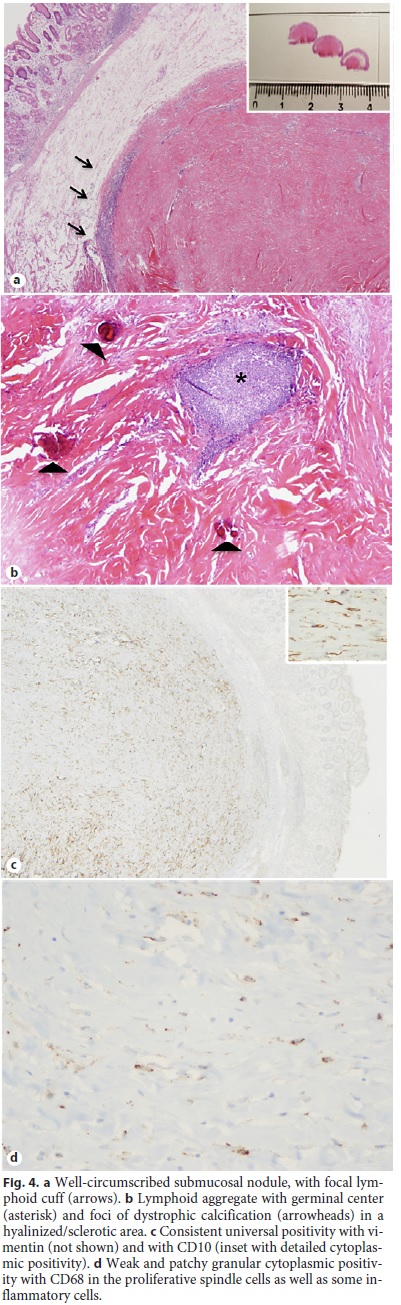
A 55-year-old woman with no relevant past medical history was referred to our department for reevaluation of a gastric lesion detected on a esophagogastroscopy. The lesion was described as a bulge at the gastric body, measuring 10 mm, with overlying normal appearing mucosa (Fig. 1). Endoscopic ultrasound (EUS) revealed a 9 × 12 mm hypoechoic, homogeneous lesion mainly localized within the submucosa, with well-defined and regular limits. Taking into account the reduced lesion size, ultrasonographic characteristics and patient preference, an enbloc cap-assisted endoscopic submucosal resection was performed, with no complications (Fig. 2, Fig. 3). Histologically, a complete (R0) resection was observed with a submucosal sharply delineated hypocellular spindle cell proliferation, haphazardly arranged, set in an abundant collagenous hyalinized stroma. Peripheral lymphoid cuffs, patchy lymphoplasmacytic aggregates frequently associated with small vessels, sometimes with germinal centers and dispersed foci of dystrophic calcification were noticed (Fig. 4). Immunohistochemical staining showed positivity with vimentin and CD10. A patchy, granular positivity with CD68 was also obtained (Fig. 4). Tumor cells were negative for CD34, CD117, DOG-1, BCL2, desmin, SMA, HHF35, S100, AE1/AE3, Cam5.2, ALK-1, and betacatenin. A diagnosis of gastric calcifying fibrous tumor (CFT) was made. Six months after endoscopic resection, the patient presented no signs of tumor recurrence.

CFTs are rare benign mesenchymal tumors with a predilection for the soft tissue and the subserosal abdominal cavity that occur mainly in children and young adults. CFTs of the gastrointestinal tract are quite rare and very few cases have been reported in the gastric wall. Gastric CFTs seem different from their soft tissue counterpart in their smaller tumor size, higher age at presentation, and no tendency for local recurrence. No sex predominance has been documented, age of presentation is usually in the fifth or sixth decade, and the majority are located in the gastric body [1–4].
Awareness of CFT and differential diagnosis with other mesenchymal tumors is important but not always straightforward. The main differential diagnosis is probably gastrointestinal stromal tumor (GIST), which is usually more cellular than CFT and lacks the hyaline stroma, the lymphoplasmacytic infiltrate, and lymphoid cuff. More importantly, GIST has typical expression of CD34, CD117, and/or DOG-1, which were negative in this case. Moreover, CD68 is negative in GIST. CD10 positivity was observed in our case and has not yet been reported in the literature since it has never been tested in any published series of CFT. Other tumors can enter the differential diagnosis such as schwanomma, hyalinized leiomymoma, reactive nodular fibrous pseudotumor, solitary fibrous tumor, inflammatory myofibroblastic tumor, and IgG4-related disease. Characteristic findings of these entities were lacking [1–2, 5].
With no specific symptoms or endoscopic or EUS findings, the diagnosis of CFTs relies largely on pathological evaluation. Given its excellent prognosis, differential diagnosis with other mesenchymal tumors is essential. In fact, malignant transformation has never been reported and rare recurrences occur primarily when resection is incomplete. Provided a complete resection can be ensured, endoscopy is a feasible and safe approach not only for diagnosis but also for management of this entity [1–4].
References
1 Agaimy A, Bihl MP, Tornillo L, Wünsch PH, Hartmann A, Michal M: Calcifying fibrous tumor of the stomach: clinicopathologic and molecular study of seven cases with literature review and reappraisal of histogenesis. Am J Surg Pathol 2010;34:271–278. [ Links ]
2 Pezhouh MK, Rezaei MK, Shabihkhani M, Ghosh A, Belchis D, Montgomery EA, Voltaggio L: Clinicopathologic study of calcifying fibrous tumor of the gastrointestinal tract: a case series. Hum Pathol 2017;62:199–205. [ Links ]
3 Larson BK, Dhall D: Calcifying Fibrous Tumor of the Gastrointestinal Tract. Arch Pathol Lab Med 2015;139:943–947. [ Links ]
4 Shi Q, Xu MD, Chen T, Zhong YS, Zhou PH, Wu HF, Yao LQ: Endoscopic diagnosis and treatment of calcifying fibrous tumors. Turk J Gastroenterol 2014; 25(suppl 1):153–156. [ Links ]
5 Bosman FT, Carneiro F, Hruban RH, Theise ND: Tumous of the stomach. In: WHO Classification of Tumours of the Digestive System (4th edition). Lyon. IARC Press, 2010. [ Links ]
Disclosure Statement
The authors do not have any interest which might be interpreted as influential in this report. This report did not receive any support from corporations, industrial or private.
* Corresponding author.
Dr. Jaime P. Rodrigues
Gastroenterology Department, Centro Hospitalar Vila Nova de Gaia/Espinho
Rua Conceição Fernandes
PT–4434-502 Vila Nova de Gaia (Portugal)
E-Mail jaimepereirarodrigues@gmail.com
Received: November 17, 2017; Accepted after revision: February 18, 2018














