Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa abr. 2019
https://doi.org/10.1159/000487550
ENDOSCOPIC SNAPSHOT
Endoscopic Resection of a Rectal Neuroendocrine Tumor: Hybrid Endoscopic Submucosal Dissection
Resseção endoscópica de um tumor neuroendócrino do recto: disseção submucosa endoscópica híbrida
Marta Gravito-Soaresa,c, Elisa Gravito-Soaresa,c, Pedro Amaroa, Inês Cunhaa, João Fragab, Luís Toméa,c
aGastroenterology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; bPathology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; cFaculty of Medicine, University of Coimbra, Coimbra, Portugal
* Corresponding author.
Keywords: Hybrid endoscopic submucosal dissection, Neuroendocrine tumor, Rectum
Palavras-Chave: Disseção submucosa endoscópica híbrida, Tumor neuroendócrino, Recto
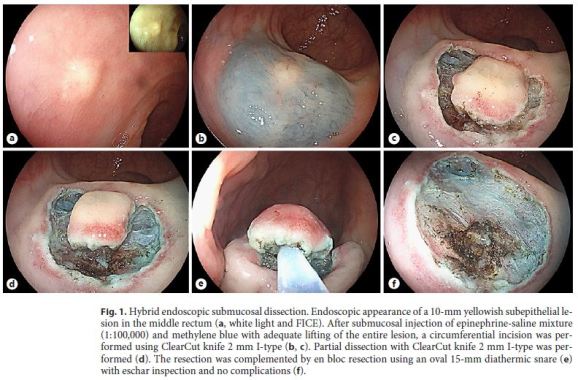
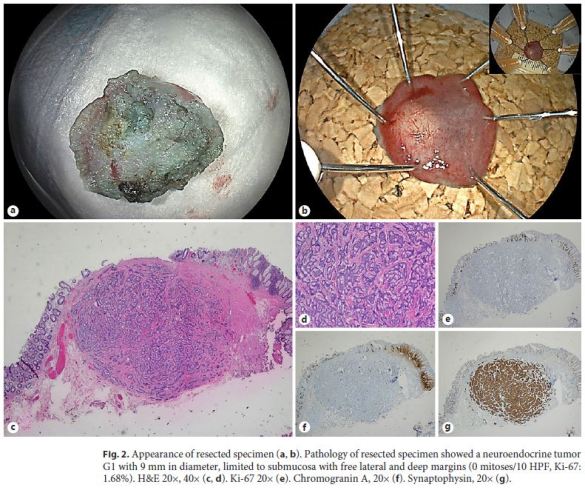
A 67-year-old man was referred to our institution due to a 10-mm yellowish subepithelial lesion in the middle rectum incidentally diagnosed during screening colonoscopy. Conventional biopsies showed a well-differentiated neuroendocrine tumor (NET). Abdominopelvic computed tomography and endoscopic ultrasound showed limited submucosal invasion and no locoregional/distant metastasis. It was decided to perform a hybrid endoscopic submucosal dissection (ESD) technique. First, submucosal injection was performed using methylene-blue-stained saline containing 1: 100,000 epinephrine with adequate lesion lifting; second, a circumferential incision with a 1–2 mm free margin (ERBE VIO 300D: Endocut I, effect-1) was made using a ClearCut knife 2 mm I-type (Finemedix, South Korea); third, a partial submucosal dissection was done, using the same knife and settings; and fourth, an en bloc resection with an oval 15-mm diathermic snare (Olympus, Spain) was performed (Forced Coag, effect-2 80 W) without complications and resection time of 9 min (Fig. 1a–f). Histopathology showed a 9-mm NET G1 (WHO classification, 0 mitoses/10 HPF, Ki-67: 1.8%; pT1a AJCC stage 1), limited to the submucosa with free lateral (1.0 mm) and deep (0.6 mm) resection margins (Fig. 2a–g). Considering R0 resection of a < 10-mm rectal NET (R-NET), no followup was scheduled.
Despite the increasing incidence due to the widespread use of screening colonoscopy, R-NET are relatively rare and often well differentiated [1–5]. Endoscopic resection plays a central role in the resection of small well-differentiated R-NET (< 10 mm) and selected cases measuring 10–20 mm, given the low risk of metastasis [2–4]. There is no consensus regarding the best endoscopic resection technique [1, 2, 4, 5], including conventional polypectomy, endoscopic mucosal resection (EMR) or ESD. Conventional polypectomy should be avoided as complete resection is often not achieved [1, 4] and EMR shows a suboptimal complete resection rate (30–70%) due to frequent submucosal involvement affecting mostly the vertical margin [1, 3, 5]. Incomplete resection requires endoscopic retreatment with additional difficulty due to submucosal fibrosis, surgery and/or long-term follow-up. Alternatively, ESD has a higher complete resection rate (80– 100%) with the disadvantage of being a complex and time-consuming procedure and an increased risk of complications [1–4].
Recently, modified EMR (cap- or band ligation-assisted), hybrid EMR/ESD (H-EMR/ESD) techniques, and full-thickness resection [1, 3–5] have been proposed to improve in-depth resection of conventional EMR and decrease ESD drawbacks [3–5]. These techniques have a comparable complete resection rate (70–100%) and similar safety profile as ESD, but with a shorter procedure time [1–4]. H-EMR/ESD has an additional advantage for difficult lesions and tumor size close to 10 mm or larger, reducing recurrence rate related with modified-EMR due to the limited tumor size that can be aspirated [2, 5]. However, there are no randomized trials comparing these different resection techniques.
Although ESD, modified EMR, and H-EMR/ESD could be adequate in this case, considering the pericentimetric endoscopic size of the lesion, the authors opted to perform an H-EMR/ESD in order to secure horizontal free margin. Partial submucosal dissection after complete circumferential incision was additionally performed to provide a deeper submucosal resection and more precise snaring beneath the lesion, theoretically increasing the vertical tumor-free margin without the risk of a full dissection. H-EMR/ESD may be a good treatment choice for small R-NET limited to submucosa, without significantly compromising the completeness, timing, and safety of the procedure.
References
1 Chablaney S, Zator ZA, Kumta NA: Diagnosis and management of rectal neuroendocrine tumors. Clin Endosc 2017;50:530–536. [ Links ]
2 He L, Deng T, Luo H: Efficacy and safety of endoscopic resection therapies for rectal carcinoid tumors: a meta-analysis. Yonsei Med J 2015;56:72–81. [ Links ]
3 Park SB, Kim HW, Kang DH, et al: Advantage of endoscopic mucosal resection with a cap for rectal neuroendocrine tumors. World J Gastroenterol 2015;21:9387–9393. [ Links ]
4 Bang BW, Park JS, Kim HK, et al: Endoscopic resection for small rectal neuroendocrine tumors: comparison of endoscopic submucosal resection with band ligation and endoscopic submucosal dissection. Gastroenterol Res Pract 2016;2016:6198927. [ Links ]
5 Zhang J, Liu M, Li H, et al: Comparison of endoscopic therapies for rectal carcinoid tumors: endoscopic mucosal resection with circumferential incision versus endoscopic submucosal dissection. Clin Res Hepatol Gastroenterol 2018;42:24–30. [ Links ]
Statement of Ethics
Protection of human and animal subjects: The authors declare that no experiments were performed on humans or animals for this study. Confidentiality of data: The authors declare that they have followed the protocols of their work center on the publication of patient data. Right to privacy: The authors declare that no patient data appear in this article. Informed patient consent for publication: Informed consent was obtained for this case report.
Disclosure Statement
The authors declare no disclosures to report.
* Corresponding author.
Dr. Marta Gravito-Soares
Gastroenterology Department, Centro Hospitalar e Universitário de Coimbra
Praceta Prof. Mota Pinto PT–3000-075 Coimbra (Portugal)
E-Mail ms18498@gmail.com
Received: December 11, 2017; Accepted after revision: February 7, 2018
Author Contributions
Marta Gravito-Soares and Elisa Gravito-Soares contributed equally, writing the manuscript and reviewing the literature. Marta Gravito-Soares is the article guarantor. João Fraga reviewed histologic findings. Pedro Amaro, Inês Cunha, and Luís Tomé contributed to critical revision of the manuscript for important intellectual content.














