Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.5 Lisboa out. 2018
https://doi.org/10.1159/000485841
ENDOSCOPIC SNAPSHOT
Role of Direct Peroral Cholangioscopy in Difficult Biliary Stones: A Case Report
Papel da Colangioscopia Peroral Direta NA Litíase Difícil: Descrição de um Caso
Marco Silva, Armando Peixoto, Eduardo Rodrigues-Pinto, Pedro Pereira, Guilherme Macedo
Gastroenterology Department, Centro Hospitalar de São João, Porto Medical School, Porto, Portugal
* Corresponding author.
Keywords: ERCP, Choledocholithiasis, Biliodigestive anastomosis
Palavras-Chave: CPRE, Coledoclitíase, Anastomose biliodigestive
The authors report the case of a 76-year-old female with a medical history of liver transplant in 1991 for primary biliary cholangitis, which was complicated with an anastomotic stricture. She had previously been submitted to 4 endoscopic retrograde cholangiopancreatography (ERCP) procedures (between 2009 and 2016), including 2 direct peroral cholangioscopies (POC) [1], due to episodes of symptomatic choledocholithiasis/cholangitis.
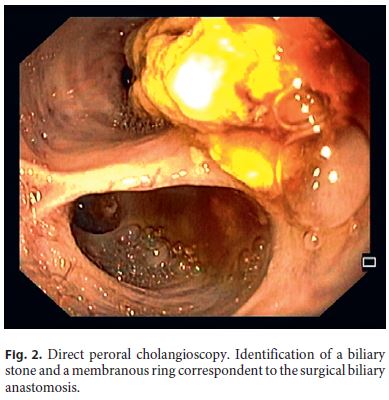
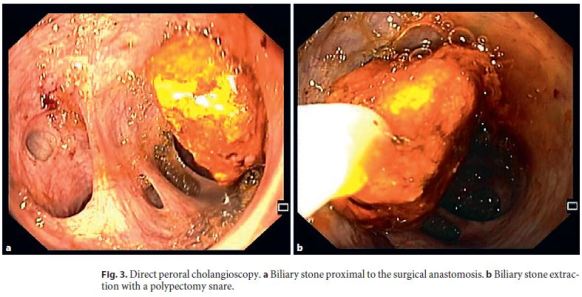
In the last procedure, balloon catheter passage and POC with mechanical lithotripsy failed to remove the largest stone, and a plastic stent was placed to permit biliary drainage and promote partial stone fragmentation (Fig. 1). Three months later, POC was repeated with a conventional videogastroscope (Olympus® GIF-Q180), with identification of a biliary stone at the anastomosis (Fig. 2), which was removed with a Roth Net®. A cholangiogram confirmed the persistence of a subtraction defect of 20 mm, proximal to the anastomosis. Mechanical lithotripsy (Olympus® BML-110 Mechanical Lithotriptor) was attempted without success. Then, anastomosis dilatation up to 15 mm (Boston Scientific® CRE Wireguided Balloon Dilation) was performed, under direct and fluoroscopic control. Subsequently, the conventional endoscope was introduced proximal to the anastomosis with direct visualization of the calculus, which was successfully removed recurring to a polypectomy snare (Olympus® SnareMaster) (Fig. 3). The final cholangiogram revealed no subtraction defects, with proper biliary drainage.

Benign biliary strictures are mostly related to liver transplantation or chronic pancreatitis [2]. Benign biliary strictures are mostly related to liver transplantation or chronic pancreatitis [2]. In fact, anastomotic strictures are one of the most common adverse events after liver transplantation, occurring in up to 34% of cases, being more common in transplants with living liver donors [3]. In the recent years, endoscopic treatment with balloon dilation or biliary stent has become the gold standard, and surgical intervention is reserved for unsuccessful or inaccessible strictures to endoscopic treatment [3]. Even though the optimal endoscopic strategy for the treatment of these strictures remains to be defined, in a recent metaanalysis, Aparício et al. [3] concluded that the endoscopic treatment of anastomotic strictures with fully covered self-expandable metal stents was equally effective as the treatment with plastic stents, but the former was associated with a lower complication risk. Also, the use of single-balloon dilation or balloon dilation combined with plastic stents presented similar outcomes [3].
Frequently, anastomotic strictures are associated with formation of sludge or biliary stones. In most cases, biliary stones can be removed by ERCP using conventional techniques, such as an extraction balloon or basket, but difficult or large stone removal may constitute a therapeutic challenge. POC using a conventional endoscope allows a better visualization of the biliary tree and the treatment of difficult-to-remove stones for which conventional techniques have failed. Several studies have reported high success rates in clearing the bile ducts of stones using intraductal electro-hydraulic or holmium laser lithotripsy under direct vision during cholangioscopy [4–6]. Although the use of holmium laser lithotripsy would be a suitable option for the case presented here, it was not available at the time in our institution. Also, laser lithotripsy is an expensive method, and the reported case shows that the use of POC with a conventional endoscope may be a cheaper, safe, and effective procedure in selected cases. Aggressive balloon dilation may be necessary for the extraction of large bile duct stones, as shown in the reported case.
POC is considered a safe procedure; however, cases of cholangitis, pancreatitis, bleeding, infection, and fatal air embolism have been reported [4, 7–9]. The use of POC with a conventional endoscope is not always feasible, but may be considered an alternative to surgery in selected cases.
References
1 Rodrigues-Pinto E, Pereira P, Lopes S, Macedo G: Direct peroral cholangioscopy with a conventional videogastroscope in a transplanted patient with anastomotic stricture and choledocholithiasis. Rev Esp Enferm Dig 2015;107:631–632. [ Links ]
2 Dumonceau JM, Tringali A, Blero D, Devière J, Laugiers R, Heresbach D, Costamagna G; European Society of Gastrointestinal Endoscopy: Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012;44:277–298. [ Links ]
3 Aparício DPS, Otoch JP, Montero EFS, Khan MA, Artifon ELA: Endoscopic approach for management of biliary strictures in livertransplant recipients: a systematic review and meta-analysis. United European Gastroenterol J 2017;5:827–845. [ Links ]
4 Ghersi S, Fuccio L, Bassi M, Fabbri C, Cennamo V: Current status of peroral cholangioscopy in biliary tract diseases. World J Gastrointest Endosc 2015;7:510–517. [ Links ]
5 Chen YK, Parsi MA, Binmoeller KF, Hawes RH, Pleskow DK, Slivka A, Haluszka O, Petersen BT, Sherman S, Devière J, Meisner S, Stevens PD, Costamagna G, Ponchon T, Peetermans JA, Neuhaus H: Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc 2011;4:05–814. [ Links ]
6 Piraka C, Shah RJ, Awadallah NS, Langer DA, Chen YK: Transpapillary cholangioscopy-directed lithotripsy in patients with difficult bile duct stones. Clin Gastroenterol Hepatol 2007;5:1333–1338. [ Links ]
7 Sethi A, Chen YK, Austin GL, Brown WR, Brauer BC, Fukami NN, Khan AH, Shah RJ: ERCP with cholangiopancreatoscopy may be associated with higher rates of complications than ERCP alone: a single-center experience. Gastrointest Endosc 2011;73:251–256. [ Links ]
8 Hammerle CW, Haider S, Chung M, Pandey A, Smith I, Kahaleh M, Sauer BG: Endoscopic retrograde cholangiopancreatography complications in the era of cholangioscopy: is there an increased risk? Dig Liver Dis 2012;44:754–758. [ Links ]
9 Efthymiou M, Raftopoulos S, Antonio Chirinos J, May GR: Air embolism complicated by left hemiparesis after direct cholangioscopy with an intraductal balloon anchoring system. Gastrointest Endosc 2012;75:221–223. [ Links ]
Statement of Ethics
All rules of the local ethics committee (Comissão de Ética para a Saúde do Centro Hospitalar São João/Faculdade de Medicina da Universidade do Porto) were followed, preserving patient identity and confidentiality.
Disclosure Statement
The authors declare that they have no conflict of interest.
* Corresponding author.
Dr. Marco Silva
Gastroenterology Department, Centro Hospitalar São João
Alameda Professor Hernâni Monteiro
PT–4200-319 Porto (Portugal)
E-Mail marcocostasilva87@gmail.com
Received: September 19, 2017; Accepted after revision: November 28, 2017
Author Contributions
Marco Silva: performed the peroral cholangioscopy, data collection, and drafting of the manuscript. Armando Peixoto: data collection and drafting of the manuscript. Eduardo Rodrigues-Pinto: performed the peroral cholangioscopy. Pedro Pereira: critical revision of the manuscript. Guilherme Macedo: critical revision and final approval of the manuscript.














