Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.5 Lisboa out. 2018
https://doi.org/10.1159/000486242
CLINICAL CASE STUDY
Sigmoid Volvulus in Children: Diagnosis and Therapeutic Challenge
Vólvulo do Sigmóide em Idade Pediátrica: Um Desafio Clínico
Leonor Carmoa, Marina Amarala, Eunice Trindadeb, Tiago Henriques-Coelhoc,José Pinho-Sousaa
aDepartment of Pediatric Surgery, Centro Hospitalar de Vila Nova de Gaia/Espinho, Porto, Portugal; bDepartment of Pediatric Gastroenterology, Centro Hospitalar São João, Porto, Portugal; cDepartment of Pediatric Surgery, Centro Hospitalar São João, Porto, Portugal
* Corresponding author.
ABSTRACT
Background: Sigmoid volvulus is a rare condition in children. Early diagnosis increases the success of nonsurgical treatment in the emergency department, but posterior elective surgery is important due to the risk of recurrence. Methods/Conclusions: We present the case of a healthy 16-yearold girl with recurrent volvulus and successful endoscopic treatment followed by elective surgery.
Keywords: Intestinal volvulus, Colon, sigmoid, Colonoscopy,·Abdominal pain, Pediatrics
RESUMO
Introdução: A ocorrência de um vólvulo do sigmoide na criança é raro, constituindo desta forma um desafio diagnóstico. A identificação precoce desta patologia é essencial pois permite que a redução do vólvulo seja efetuada numa primeira abordagem por métodos não cirúrgicos, e quanto mais precoce na história da doença maior a taxa de sucesso e menor o risco de complicações associadas. Métodos/Conclusões: No entanto a cirurgia eletiva posterior é mandatória pelo alto risco de recidiva. Os autores apresentam o caso de uma adolescente sem antecedentes patológicos de relevo com um vólvulo sigmoideu recorrente submetido a redução endoscópica com sucesso.
Palavras-Chave: Vólvulo intestinal, Cólon sigmoide, Colonoscopia, Dor abdominal, Pediatria
Introduction
Sigmoid volvulus is a rare cause of pediatric bowel obstruction [1]. It occurs due to torsion of a dilated sigmoid colon around its mesenteric axis. This causes venous and arterial blood flow obstruction with progressive bowel ischemia, necrosis, and perforation if left untreated [2]. The clinical presentation can be acute with intense abdominal pain, abdominal distention, and vomiting, or chronic with vague symptoms. Physical examination results are unspecific, and the diagnosis relies on a high clinical suspicion and further complementary studies [1, 2]. There is no consensus on the best diagnostic imaging modality, but the procedures most often performed on children remain abdominal radiography and CT.
Clinical suspicion allows an early diagnosis and a nonsurgical approach in the acute setting, decreasing the morbidity and mortality associated with perforation and necrosis. Nevertheless, the definite treatment in children consists of sigmoid resection and primary anastomosis, due to the risk of recurrence.
The aim of this clinical case study is to make this rare entity in children known to clinicians and to assess the safety and benefits of endoscopic reduction as the primary approach, without precluding definitive surgery.
Clinical Case
A healthy teenager was admitted to the emergency department due to a 1-day history of intense, generalized, cramping abdominal pain, nausea, and abdominal distention, with no other symptoms. Previous episodes of generalized abdominal pain were described, but of lower intensity, normally resolving with the passage of stools. She had a previous history of functional constipation, with improvement in the last years and no follow-up at the moment. She had no history of previous abdominal surgeries.
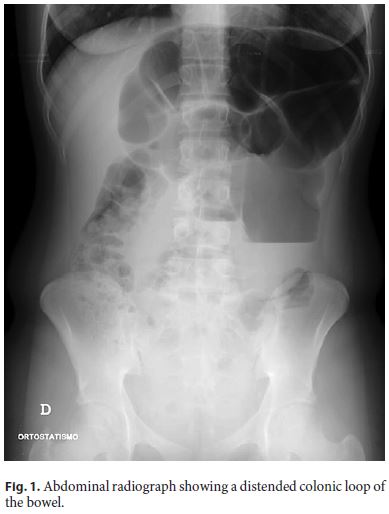
On physical examination she was pale, sudoretic, tachycardic, with abdominal distention, subtle metallic bowel sounds, and tenderness on palpation of the left abdominal quadrants with associated voluntary guarding. Blood count and serum chemistry results were normal. Abdominal ultrasound showed generalized intestinal distention, without free fluid or inflammatory findings. Upright abdominal radiography (Fig. 1) revealed a dilated colon on the left quadrants, with an air-fluid level. Abdominal CT was performed (Fig. 2), which identified a distended gas-filled colonic loop on the left quadrant, probably the sigmoid, associated with twisting of the correspondent mesentery and vessels (whirlpool sign). These findings were compatible with intestinal occlusion probably from a sigmoid volvulus.

An endoscopic exsufflation reduction was decided for first-line treatment and was performed with success under general anesthesia. The patient was asymptomatic after the procedure and discharged on the following day. She was scheduled for a follow-up consultation with a pediatric surgeon.
Four months later, she was readmitted to the emergency department with the same complaints and additional nonbilious vomiting. The complementary examinations confirmed the recurrence of sigmoid volvulus. A broad-spectrum prophylactic antibiotic treatment and fluid resuscitation was started and colonoscopic reduction under general anesthesia was performed. During the procedure, a complete bowel obstruction was identified 25 cm from the anal margin. Reduction with exsufflation and fluid instillation was completed with success, and a complete colonoscopy showed no signs of bowel ischemia. The patient was admitted to the hospital for further study and monitoring. On the following day, a barium enema was requested to exclude a transition zone (due to the previous history of constipation and to evaluate a possible Hirschsprung disease). The examination identified a redundant distended sigmoid colon with a narrow and long axis, with no visible transition zone (Fig. 3).

Due to the risk of recurrence, it was decided to perform an elective surgery on the 4th day of hospital stay. Upon surgery, a redundant sigmoid colon with a large diameter and a narrow, long mesenteric axis was visible. Signs of malrotation were searched for and excluded. A sigmoidectomy with primary end-to-end colonic anastomosis was conducted, and the postoperative period was uneventful. A histopathological analysis identified a normal ganglion distribution. To date, the patient has been followed up for 2 years in the outpatient clinic, without symptoms.
Discussion
Sigmoid volvulus is a rare condition in children but should be a differential diagnosis of intense abdominal pain. In pediatrics, it is most often associated with congenital anomalies of the fixation of the colon (a redundant sigmoid colon with a short mesenteric axis), a longstanding history of constipation, or Hirschsprung disease [1, 3–6]. Different studies found an incidence of Hirschsprung disease in up to 18% of patients with sigmoid volvulus [4, 6]. There are also reports that identified roundworm infestation [6, 7], malrotation [1], and neurologic disorders [2, 6] as predisposing factors.
Clinical awareness and an early diagnosis increase the success of nonsurgical detorsion (either by contrast enema or colonoscopy), preventing the ischemic/necrotic bowel complications and morbidity of emergent surgery. Nevertheless, this diagnosis can be challenging, especially in children. In adults, abdominal radiographs identify the omega or coffee bean sign in more than 60% of cases, but in children this has only a 17–30% success rate [1, 2, 4]. The most common findings in radiographs of children are colonic distention or an air-fluid level in sigmoid loops [1, 8].
Abdominal contrast-enhanced CT is the second most often performed examination for the diagnosis of bowel volvulus, being diagnostic in approximately 56% of pediatric cases of sigmoid volvulus, normally by identifying a swirled mesentery or the beak sign [2]. It also has the advantaged of evaluating the presence of bowel wall necrosis, which is an indication for surgery.
After diagnosis, IV resuscitation, placement of a nasogastric tube, and broad-spectrum antibiotics should be administered. Most authors agree that if a patient is stable and there are no signs of bowel perforation or necrosis, a nonoperative reduction must be attempted [2, 9]. The importance of these procedures is that they reduce the higher complication rate associated with a colectomy in an emergency setting [2, 6]. The main controversy is about whether it should be endoscopic or a contrast enema reduction. Proponents of enema reduction advocate that it is a diagnostic (identification of the birds beak sign) and therapeutic procedure that simultaneously facilitates bowel preparation for surgery, being successful in up to 77% of cases [1–3, 6, 7]. Nevertheless, it is believed by some to have a higher complication rate (perforation due to bowel ischemia), and sometimes more than one attempt is necessary [1, 4]. As for endoscopic reduction, previous reports have stated a lower success rate in children [1, 2, 7], but a recent review of the literature reported a success rate of 69% and no associated complications, also having the advantage that it allows for inspection of the bowel mucosa and avoiding exposure to radiation [6]. The main complications associated with this procedures are iatrogenic bowel perforation and unsuccessful detorsion. In the review of the pediatric literature there are no described cases of perforation. In order to reduce this complication, the following points are important: (1) a thorough selection of patients and the reduction technique, (2) avoidance of excessive air insufflation, and (3) the use of flexible scopes. Rigid devices should not be used, because of higher perforation rates [6]. Patients that are clinically unstable or have a suspected bowel perforation, bowel necrosis, or peritonitis are contraindicated for endoscopic/nonsurgical reduction.
These patients and those on whom nonsurgical procedures have failed should undergo emergent surgery. For stable patients submitted to successful nonsurgical reduction, posterior elective sigmoidectomy is the gold standard, due to the high risk of recurrence (more than 65%). This is even more important in this age group, because of the patients longer average life expectancy [1, 4–6]. It should be done as a semi-elective procedure during the same period of hospital stay, normally after at least 24–48 h, due to the high early recurrence rates [1, 6]. It is also recommended that a full-thickness rectal biopsy be performed for immunohistochemical study to rule out Hirschsprung disease [2, 3].
Several nonresective alternative surgical techniques have been described for nongangrenous sigmoid volvulus, advocating that they prevent the morbidity related to colectomy. Some of these techniques are extraperitonization and mesosigmoidoplasty, widening of the sigmoid mesentery (following the principles of Ladds procedure in midgut volvulus), and percutaneous endoscopic or surgical sigmoidopexy [6, 7, 10]. Reports of these techniques in children are limited to case reports; they show a higher recurrence rate and the long-term results are not described.
Although rare, colonic volvulus should be considered in the differential diagnosis of pediatric bowel occlusion. The best management approach for patients with acute, noncomplicated presentation is debatable, but there is a consensus that nonsurgical reduction should be attempted in order to stabilize patients for a posterior, definitive surgery.
References
1 Salas S, Angel CA, Salas N, Murillo C, Swischuk L: Sigmoid volvulus in children and adolescents. J Am Coll Surg 2000;190:717–723. [ Links ]
2 Tannouri S, Hendi A, Gilje E, Grissom L, Katz D: Pediatric colonic volvulus: a single-institution experience and review. J Pediatr Surg 2017;52:1062–1066. [ Links ]
3 Khalayleh H, Koplewitz BZ, Kapuller V, Armon Y, Abu-Leil S, Arbell D: Neonatal sigmoid volvulus. J Pediatr Surg 2016;51:1782–1785. [ Links ]
4 Zeng M, Amodio J, Schwarz S, Garrow E, Xu J, Rabinowitz SS: Hirschsprung disease presenting as sigmoid volvulus: a case report and review of the literature. J Pediatr Surg 2013;48:243–246. [ Links ]
5 Gingold D, Murrell Z: Management of colonic volvulus. Clin Colon Rectal Surg 2012;25:236–244. [ Links ]
6 Parolini F, Orizio P, Bulotta AL, Garcia Magne M, Boroni G, Cengia G, Torri F, Alberti D: Endoscopic management of sigmoid volvulus in children. World J Gastrointest Endosc 2016;8:439–443. [ Links ]
7 Parolini F, Alberti D: Sigmoid volvulus in children. Surgery 2017;161:562–563. [ Links ]
8 Colinet S, Rebeuh J, Gottrand F, Kalach N, Paquot I, Djeddi D, et al: Presentation and endoscopic management of sigmoid volvulus in children. Eur J Pediatr 2015;174:965–969. [ Links ]
9 Onuoha U, Möhrlen U, Meuli M: Sigmoid volvulus – with a twist. J Pediatr Surg Case Rep 2013;1:230–231. [ Links ]
10 Chiang LL, Lai HS, Ni YH, Hsu WM: Management of sigmoid volvulus based on Ladds procedure: a case report. Pediatr Neonatol 2009;50:129−131. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest do declare.
* Corresponding author.
Dr. Leonor Carmo
Serviço de Cirurgia Pediátrica, Centro Hospitalar Vila Nova de Gaia/Espinho
Unidade 2, Rua Francisco Sá Carneiro
PT–4400-129 Vila Nova de Gaia (Portugal)
E-Mail leonorfmcarmo@gmail.com
Received: October 11, 2017; Accepted after revision: December 11, 2017














