Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
GE-Portuguese Journal of Gastroenterology
Print version ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.5 Lisboa Oct. 2018
https://doi.org/10.1159/000485567
ORIGINAL ARTICLE
Clinical Practice Impact of the Boston Bowel Preparation Scale in a European Country
Impacto Clínico da Classificação de Boston num País Europeu
Paulo Massinhaa, Nuno Almeidaa,b, Inês Cunhaa, Luís Toméa
aDepartment of Gastroenterology, Centro Hospitalar e Universitário de Coimbra, and bFaculty of Medicine, Coimbra University, Coimbra, Portugal
* Corresponding author.
ABSTRACT
Introduction: The diagnostic acuity of colonoscopy requires a careful evaluation of the colonic mucosa, so an adequate bowel cleansing is a key element of the procedure. It is internationally recommended that an evaluation of the quality of the intestinal preparation should be included in the colonoscopy report. The Boston Bowel Preparation Scale (BBPS) is a bowel cleanliness rating scale that has gained some preponderance in this context. However, its application implies some degree of subjective appreciation, and it is important to conduct interobserver reproducibility studies in different contexts. The objective of the present study was to evaluate the reliability of the BBPS in the Portuguese gastroenterological community. Methods: A prospective study involving Portuguese gastroenterologists with clinical practice in several contexts, and using different methods of evaluation of the intestinal preparation. Participants were invited to answer a questionnaire encompassing 93 static images and 12 video segments of colonoscopy examinations, with different levels of intestinal preparation. For each item, the participant gastroenterologist assigned a score of 0–3, according to the BBPS criteria. A statistical analysis was performed with SPSS 20.0 software, using the intraclass correlation coefficient (ICC). Results: From 45 invited gastroenterologists, 36 replied (mean age 39 ± 9 years). Fifteen (41%) had more than 10 years of colonoscopy experience and 20 (56%) performed more than 40 examinations per month. Twenty-seven (77%) usually used the BBPS in their daily practice. Statistical analysis revealed a strong interobserver correlation (ICC = 0.783) in the application of the BBPS, even in those gastroenterologists who did not use the scale in their daily routine (ICC = 0.775) and those with less years of experience (ICC = 0.820). The correlation in the videos was slightly lower than that observed in the static images (ICC = 0.74 vs. ICC = 0.78). Conclusion: The application of the BBPS in the Portuguese gastroenterology community is reproducible and can represent a way to harmonize the colonoscopy reports, contributing to its correct interpretation and subsequent patient orientation.
Keywords: Boston Bowel Preparation Scale, Colonoscopy, Bowel preparation
RESUMO
Introdução: A acuidade diagnóstica da colonoscopia exige uma visualização cuidadosa da mucosa, pelo que uma adequada preparação intestinal é um dos elementos chave para otimização do exame. É internacionalmente recomendado que a avaliação da qualidade da preparação intestinal seja incluída no relatório da colonoscopia. A escala de preparação intestinal de Boston (BBPS) tem ganho alguma preponderância neste contexto, mas a sua determinação inclui uma apreciação algo subjetiva, sendo importante realizar estudos de reprodutibilidade interobservador em diferentes contextos. O objetivo do presente estudo foi avaliar esta mesma reprodutibilidade na comunidade gastrenterológica portuguesa. Métodos: Estudo prospetivo envolvendo Gastrenterologistas portugueses de diferentes faixas etárias e com prática clínica em diferentes contextos Os Gastrenterologistas foram convidados, de forma aleatória, para avaliar, online, 93 imagens estáticas e 12 vídeos de segmentos intestinais, com diferentes níveis de preparação. Para cada uma destas imagens/vídeos o participante atribuía uma pontuação de 0 a 3, segundo os critérios da BBPS. A análise estatística foi realizada com o software SPSS 20.0, utilizando o coeficiente de correlação intraclasses (ICC). Resultados: Dos 45 Gastrenterologistas convidados, 36 (Média etária – 39 ± 9 anos) aceitaram participar (taxa de resposta de 80%). Quinze (41%) tinham mais de 10 anos de experiência em colonoscopia e 20 (56%) realizavam mais de 40 exames por mês. Recorriam a diferentes métodos de avaliação da preparação intestinal (27 (77%) utilizavam habitualmente a BBPS). A análise estatística revelou uma correlação interobservador forte (ICC = 0.783) na aplicação da BBPS, mesmo nos Gastrenterologistas que não utilizavam a escala no seu dia-a-dia (ICC = 0.775) e nos com menos anos de experiência (ICC = 0.820). A correlação nos vídeos foi ligeiramente inferior à observada nas imagens estáticas (ICC = 0.74 vs. ICC = 0.78). Conclusão: A aplicação da BBPS na comunidade gastrenterológica portuguesa revela-se reprodutível, podendo representar uma forma de harmonizar os relatórios, contribuindo assim para a sua correta interpretação e posterior orientação dos doentes.
Palavras-Chave: Escala de Preparação Intestinal de Boston, Colonoscopia,·Preparação intestinal
Introduction
A meticulous observation of the colonic mucosa is the main objective of colonoscopy. For this purpose, it is mandatory to obtain an adequate bowel preparation. Failure to achieve a correct cleansing of the bowel can lead to missed lesions, prolonged procedure duration, and unnecessary repeated examinations at earlier intervals [1].
The American Society for Gastrointestinal Endoscopy (ASGE) and the European Society of Gastroenterology and Endoscopy (ESGE) recommended that every colonoscopy report should incorporate an evaluation of the quality of bowel preparation [2, 3]. Several scales with the aim of evaluating bowel preparation quality, such as the Aronchick Scale, Ottawa Bowel Preparation Scale, Harefield Cleansing Scale, Chicago Bowel Preparation Scale, and Boston Bowel Preparation Scale (BBPS), have emerged over time, but prior attempts to introduce this bowel preparation descriptors have been limited by their lack of extensive validation and reliability testing, and their unwieldy complexity in practice [4, 5].
The BBPS, developed at the Boston University Medical Center, USA, has been attracting worldwide attention. The BBPS is a 9-point standardized evaluation scale that was initially intended for use in colonoscopy-oriented investigation [6]. In contrast to preceding rating scales that considered the degree of bowel cleanliness encountered by endoscopists during the initial inspection of the colon, the BBPS assesses bowel preparation during withdrawal of the colonoscope, after all cleansing maneuvers, such as washing and suctioning of fluid, have been completed [7–9]. Rather than relying on a conventional global assessment of the bowel, the BBPS uses a summation of 3 colonic segment scores (for the right, transverse, and left colonic regions) to show the grade of bowel visualization [6].
Despite the simplicity of the application of this scale, its use is conditioned by a somewhat subjective appraisal, requiring interobserver reproducibility studies in different contexts and different degrees of experience to evaluate the true usefulness of this scale. This study examined the reliability of the BBPS assessment by different gastroenterologists in several medical institutions in Portugal.
Methods
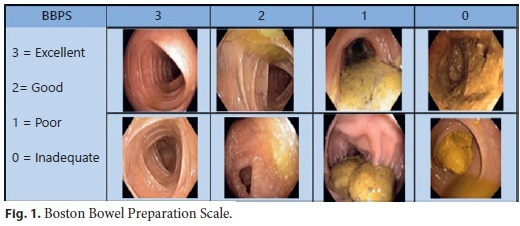
The BBPS was explained in detail by Lai et al. [6]. Concisely, this scale is applied during the withdrawal stage of colonoscopy, after all washing, suctioning, and other cleansing maneuvers have been carried out. The 3 segments of the colon (right, including the splenic flexures; and left, including the descending colon, sigmoid, and rectum) are given a score from 0 to 3 defined as follows: 0 = unprepared colon segment with mucosa not visible due to remnants of solid stool that cannot be cleared; 1 = portions of mucosa of the colon segment are visible, but other areas of the colon segment cannot be clearly visualized because of staining, residual stool, and/or opaque liquid; 2 = minor amount of residual staining, small fragments of stool and/or opaque liquid, but mucosa of the colon segment seen well; 3 = entire mucosa of the colon segment clearly visible with no residual staining, stool fragments, or opaque liquid (Fig. 1). The 3 segment scores are summed up separately to achieve a total score from 0 to 9, for which 0 indicates a completely unprepared bowel and 9 represents an entirely clean bowel. If an endoscopist aborts a procedure because of inadequate preparation, then any nonvisualized proximal segments are assigned as nonapplicable [6].
In this study, we prospectively evaluated the reliability of BBPS through an online questionnaire, using Google Forms, during a 2-month period (March and April 2017). In this query, besides the explanation of the study and its objectives, an online instructional video demonstrating the proper use of the BBPS was provided to all participants. This online instrument was created by the Gastroenterology Division at Boston University Medical Center in Boston, USA, and is available freely (http://www.cori.org/bbps/instruction.php). In the questionnaire, 93 images and 12 video segments of colonoscopies were presented and the participants were asked to assess them by using the BBPS. The following data were also collected: attendants name, years of experience, average number of colonoscopies per month, and workplace.
To assess interobserver reliability, we calculated the intraclass correlation coefficient (ICC) among total BBPS scores provided by the participants. All statistical analyses were carried out using SPSS 20.0 software (SPSS, Chicago, IL, USA). To assess any differences between the best and worst preparations, we requested 5 gastroenterologists with good experience in colonoscopy and use of the BBPS to assess, in a consensual way, our images/videos in 4 subgroups, i.e., BBPS 3, 2, 1 and 0, allowing us to compare the different ICC results separately in each group of images/videos.
Results
The invitation was sent to 45 gastroenterologists from different regions of Portugal, at random from our department database. From these, 36 (80%) agreed to participate in this study. Their mean age was 39 ± 9 years. Ten gastroenterologists only carried out their professional activity in the National Health System, 24 in the National Health System and private practice, and 2 only in private practice. Thirteen of them had more than 10 years of experience in colonoscopy, and another 13 between 3 and 5 years (Table 1). Twenty-three participants usually performed more than 40 colonoscopies per month, and only 1 normally performed less than 20 (Table 1). Twenty-seven (77%) usually applied the BBPS in their daily practice. Three thought its application took up too much time, 3 did not see any advantage in the use of the BBPS, and 3 thought it had no relation with practical daily use.
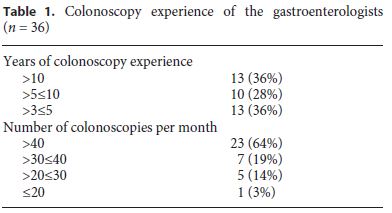
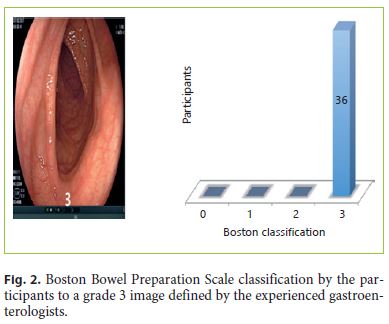
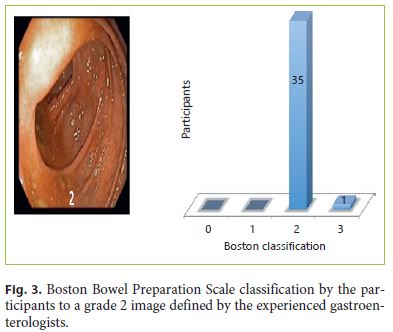
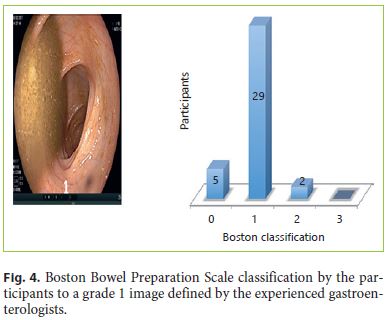
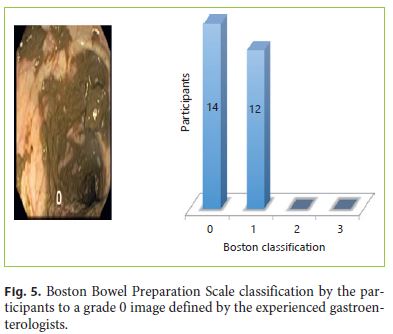
The global interobserver ICC was 0.783, which corresponds to a strong correlation. Analyzing only the images and videos consensually classified as 3 by our panel of experienced gastroenterologists, the ICC was 0.84 (very strong correlation). In the images/videos classified as 2 by the panel group, we obtained an ICC of 0.75 (strong correlation). The ICC in the images/segments classified as 1 was 0.67 (strong correlation) and for the images/segments classified as 0 the ICC was 0.66 (also a strong correlation). Figures 2, 3, 4, 5 present an example of an image classified as 3, 2, 1, and 0.
Regarding the ICC in the groups with different years of experience, the values were very similar (≥10 years ICC = 0.75; ≥6 < 10 years ICC = 0.77; >3 ≤ 5 years ICC = 0.78), with a strong interobserver correlation. The same was verified when analyzing the groups with different numbers of colonoscopies per month (≥40 colonoscopies/month ICC = 0.79; >30 < 40 colonoscopies/month ICC = 0.76; >20 ≤ 30 colonoscopies/month ICC = 0.76; ≤20 colonoscopies/month ICC = 0.75) with also a strong correlation.
The ICC was smaller in the video segments compared with static images, but not statistically significant (0.78 vs. 0.74), both with a strong correlation.
Discussion
The present study evaluated the reliability of BBPS scoring for the assessment of bowel preparation quality by gastroenterologists. We observed a strong interobserver agreement among the participating examiners. Bowel preparation quality is a critical aspect in determining the diagnostic precision of colonoscopies. High-quality colonoscopy increases treatment efficiency and reduces the costs related to the technique. Bowel preparation is one of the most frequently cited problems by the patients as an explanation for not having a screening colonoscopy, and poor preparation is a main obstacle to attaining a high-quality colonoscopy [10]. A large multicenter report found that the bowel preparation scale critically limits the quality, level of difficulty, quickness, and completeness of a colonoscopy [11]. Besides, endoscopists with a higher adenoma detection rate are more likely to be critical of the bowel preparation scale [12]. Preparation adequacy primarily impacts the ability to discern small lesions [10]. Therefore, assessment of bowel preparation quality in the colonoscopy report reflects not only bowel preparation quality itself, but also conveys the quality of the colonoscopy procedure as a whole. It should be noted that none of the bowel preparation scales have been developed and formally validated by Portuguese gastroenterologists.
BBPS scores can meaningfully guide the physicians judgment of the likelihood of a missed diagnosis, enabling him or her to better determine the follow-up interval [13]. Despite the strong correlation in all images, we observed a lower correlation when the bowel cleansing level was poor. The real impact of this phenomenon is not well known but we could assume that a colonoscopy report with an excellent preparation is reliable concerning this variable and a repeat examination is not necessary.
Reliability is an important indicator of the quality of an assessment scale [14]. The ICC value that we obtained from 36 participants rating 93 images and 12 video segments of colonoscopy cases was similar to that previously reported for the BBPS in other populations [15, 16]. With the same video demonstration, researchers at Boston University Medical Center trained 22 physicians. The ICC for interobserver variation in that study was 0.74 and a repeat test carried out 1 month later yielded a weighted kappa value of 0.77, demonstrating high reliability of the evaluation scale [17].
Our study enrolled health care professionals from different hospitals, with different skill levels in colonoscopy, and distinctive professional backgrounds. In our study, these variables had shown no differences regarding reliability. While this heterogeneity makes the examiner group more representative, it should be noted that the credibility analysis was carried out exclusively in an online form, with no previous knowledge of training in the BBPS.
We invited 45 gastroenterologists to participate in our study. Although 36 (80%) replied, we do not know the true reason for the nonresponse of the remaining 9. A major limitation of our study was the mixing of static images and videos of bowel segments. By definition, the BBPS is administered only after bowel examination. In fact, we observed a lower value in ICC in videos compared to images, although not statically relevant. The most correct way to validate the BBPS would be to present the videos of complete colonoscopies to our candidates. However, in such cases, the recruitment of gastroenterologists would probably be lower. With our results, we demonstrated a good correlation among different gastroenterologists. A future study, involving some of the present participants classifying complete colonoscopies, in a controlled environment, could now be implemented.
In addition, in our reliability analysis, though all participants were requested not to discuss their interpretations, but rather to provide BBPS scores independently, there is a possibility that others might have influenced the participants. Finally, we did not translate the instructional video of the BBPS into Portuguese. Thus, because the examiners were using materials in a language other than their native one, the variable English proficiency levels of the participants may have affected the results.
Conclusion
The BBPS is a reliable instrument for assessing the bowel preparation quality during colonoscopy by Portuguese gastroenterologists. It is easy to learn and worthy of being disseminated throughout Portugal. Upcoming reports should evaluate the validity of the BBPS in other countries, verify its reliability across the full spectrum of scores, and observe the association between BBPS scores and polyp detection rates.
References
1 Burke CA, Church JM: Enhancing the quality of colonoscopy: the importance of bowel purgatives. Gastrointest Endosc 2007;66:565–573. [ Links ]
2 Rembacken B, et al: Quality in screening colonoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE). Endoscopy 2012;44:957–968. [ Links ]
3 Faigel DO, Pike IM, Baron TH, et al: Quality indicators for gastrointestinal endoscopic procedures: an introduction. Gastrointest Endosc 2006;63(suppl):S3–S9. [ Links ]
4 Hassan C, et al: Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2013;45:142–155. [ Links ]
5 Johnson DA, et al: Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastointest Endosc 2014;80:543–562. [ Links ]
6 Lai EJ, Calderwood AH, Gheorghe D, Fix OK, Jacobson BC: The Boston Bowel Preparation Scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc 2009;69:620–625. [ Links ]
7 Rex DK, Petrini JL, Baron TH, et al: Quality indicators for colonoscopy. Am J Gastroenterol 2006;101:873–885. [ Links ]
8 Aronchick CA, Lipshutz WH: Validation of an instrument to assess colon cleansing Am J Gastroenterol 1999;94:2667. [ Links ]
9 Rostom A, Jolicoeur E: Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc 2004;59:482–486. [ Links ]
10 Harewood GC, Sharma VK, de Garmo P: Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc 2003;58:76–79. [ Links ]
11 Rex DK, Petrini JL, Baron TH, et al: Quality indicators for colonoscopy. Am J Gastroenterol 2006;101:873–885. [ Links ]
12 Thomas-Gibson S, Rogers P, Cooper S, et al: Judgement of the quality of bowel preparation at screening flexible sigmoidoscopy is associated with variability in adenoma detection rates. Endoscopy 2006;38:456–460. [ Links ]
13 Lieberman DA, et al: Guidelines for colonoscopy surveillance after screening and polypectomy:a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844–857. [ Links ]
14 Landis J, Koch G: The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174. [ Links ]
15 Calderwood AH, Jacobson BC: Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc 2010;72:686–692. [ Links ]
16 GaoY, et al: Pilot validation of the Boston Bowel Preparation Scale in China. Dig Endosc 2013;25:167–173. [ Links ]
17 Calderwood AH, Jacobson BC: Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc 2010;72:686–692. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors declare no conflicts of interest for this article.
* Corresponding author.
Dr. Paulo Massinha
Department of Gastroenterology
Centro Hospitalar e Universitário de Coimbra, EPE
Praceta Prof. Mota Pinto, PT–3000-075 Coimbra (Portugal)
E-Mail massinha@iol.pt
Received: September 8, 2017; Accepted after revision: November 21, 2017














