Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.4 Lisboa ago. 2018
https://doi.org/10.1159/000481457
ENDOSCOPIC SNAPSHOT
Adenosquamous Carcinoma of the Ampulla of Vater: A Rare Cause of Obstructive Jaundice
Carcinoma Adenoescamoso da Ampola de Vater: Uma Causa Rara de Icterícia Obstrutiva
Liliana Carvalho, Maria Ana Túlio, Joana Carmo, Miguel Bispo, Cristina Chagas
Gastroenterology Department, Hospital Egas Moniz, Centro Hospitalar de Lisboa Ocidental, Lisbon, Portugal
* Corresponding author.
Keywords: Jaundice, Endoscopic ultrasonography, Ampullary tumor, Adenosquamous carcinoma
Palavras-Chave: Icterícia, Ultrassonografia endoscópica, Ampuloma, Adenocarcinoma escamoso
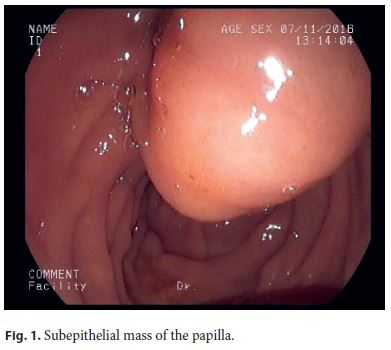
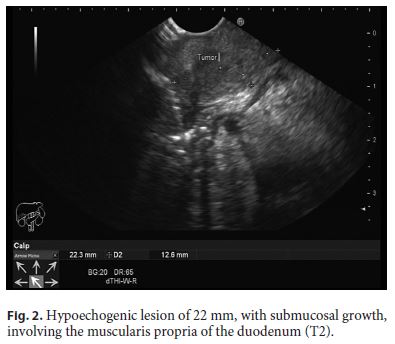
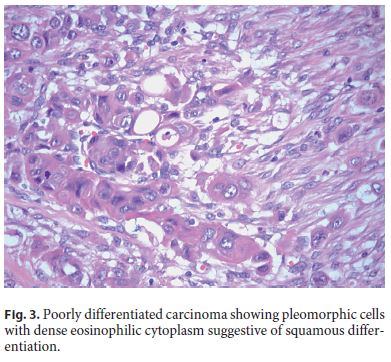
A 68-year-old Caucasian male was admitted with painless jaundice, choluria, and acholia for the previous 10 days. On admission, the patient was markedly affected by jaundice, with no relevant findings in the abdominal examination. Laboratory tests showed conjugated hyperbilirubinemia (total 15.4 mg/dL; conjugated 10.7 mg/dL), elevated transaminase levels (ALT 271 U/L; AST 102 U/L), and cholestasis parameters (GGT 1,049 U/L; AP 279 U/L). Abdominal ultrasonography revealed dilation of the common bile duct and intrahepatic biliary ducts. Tumour markers CA19.9 and CEA were normal. Endoscopic ultrasound was performed using a linear scope and showed a subepithelial mass of the papilla (Fig. 1), corresponding to a hypoechogenic lesion of 22 mm, with submucosal growth, involving the muscularis propria of the duodenum (T2) (Fig. 2). This lesion caused marked dilation of the proximal common bile duct and intrahepatic ducts. A perilesional adenopathy was identified (N1). Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) was performed using a 25-gauge needle and cytologic evaluation was consistent with adenocarcinoma. Computed tomography ruled out distant metastasis and the patient was referred for surgery (cephalic duodenopancreatectomy). Histological analysis of the surgical specimen documented an adenosquamous carcinoma of the ampulla of Vater (ASC AV; Fig. 3), involving the duodenal muscularis propria, with one regional lymph node metastasis (R0, pT2N1). Postoperative outcome was uneventful and the patient remains asymptomatic after a 10-month follow-up period.
Adenocarcinomas account for most primary malignant tumors of the ampulla of Vater, while other histological types such as squamous or adenosquamous carcinomas are exceedingly rare [1]. Duodenoscopy in combi nation with EUS-FNA are first-line diagnostic procedures in the workup of papillary tumors. Surgery is the treatment of choice in the presence of invasive carcinoma (T>T1a; N1) [2].
ASC AV is an extremely rare condition, with scarce case reports in the literature. It is defined as a tumor in which both glandular and squamous components are malignant, being clinically more aggressive, with worse prognosis than conventional adenocarcinoma [3]. The origin of squamous carcinoma in the ampulla of Vater remains unclear. Squamous metaplasia of the pancreatic ductal epithelium after chronic inflammation has been hypothesized as one of the possible oncogenic mechanisms [4].
The clinicopathological features and biologic behavior of ASC AV are largely unknown because of the rarity of this condition. Outcomes of this entity remain unclear and no therapeutic strategies have been established.
In a review of 7 cases of ASC AV, the mean age at diagnosis was 62 years and 71% were men. In 4 cases, the squamous components were identified in preoperative endoscopic biopsy results, whereas the diagnosis of adenosquamous carcinoma was made after surgical resection in 3 cases. Overall survival in all 7 cases ranged from 6 to 20 months [5].
References
1 Saavedra-Albores J, Hruban RH, Klimstra DS, Zamboni G: Invasive adenocarcinoma of the ampullary region. In: Bosman F, Carneiro F, Hruban H, Theise D (eds): WHO Classification of Tumours of the Digestive System, ed 4. Lyon, International Agency for Research on Cancer, 2010, pp 87–90. [ Links ]
2 Napoléon B: Écho-endoscopie biliaire; in Palazzo L (ed): Écho-Endoscopie Digestive. France, Springer-Verlag, 2012, pp 219–227. [ Links ]
3 Yang S-J, Ooyang C-H, Wang S-Y, et al: Adenosquamous carcinoma of the ampulla of Vater – a rare disease at unusual location. World J Surg Oncol 2013;11:124. [ Links ]
4 Balci B, Calik B, Karadeniz T, Sahin H, Ugurlu L, Aydin C: Primary squamous cell carcinoma of the ampulla of Vater: a case report. Surg Case Rep 2016;2:2. [ Links ]
5 Hoshimoto S, Aiura K, Shito M, Kakefuda T, Sugiura H: Adenosquamous carcinoma of the ampulla of Vater: a case report and literature review. World J Surg Oncol 2015;13:287. [ Links ]
Disclosure Statement
The authors have no conflicts of interest to declare.
Statement of Ethics
This report has been performed in accordance to the principles of the Helsinki Declaration, in order to protect patient confidentiality.
* Corresponding author.
Dr. Liliana Carvalho
Gastroenterology Department, Hospital Egas Moniz
Centro Hospitalar de Lisboa Ocidental, Rua Da Junqueira 126
PT–1349-019 Lisbon (Portugal)
E-Mail lilipcarvalho@gmail.com
Received: July 17, 2017; Accepted after revision: August 15, 2017














