Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.4 Lisboa ago. 2018
https://doi.org/10.1159/000484528
CLINICAL CASE STUDY
Unusual Cause of Epigastric Pain: Intra-Abdominal Focal Fat Infarction Involving Appendage of Falciform Ligament – Case Report and Review of Literature
Causa rara de epigastralgia: Enfarte focal de gordura intra-abdominal envolvendo o apêndice do ligamento falciforme – Caso clínico e revisão da literatura
Venkatraman Indiran, Rishi Dixit, Prabakaran Maduraimuthu
Sree Balaji Medical College and Hospital, Chennai, India
* Corresponding author.
ABSTRACT
Torsion of the fatty appendage of the falciform ligament, part of the spectrum of conditions known as intra-abdominal focal fat infarction (IFFI), is very rare with less than 20 cases reported on imaging so far. Here we report a case of torsion of the lipomatous appendage of the falciform ligament in a middle-aged female, diagnosed on ultrasound and computed tomography (CT). CT showed classical hyperattenuating rim sign in the anterior perihepatic space adjacent to the falciform ligament. We re-emphasize the importance of hyperattenuating rim sign on CT in recognizing IFFI in locations other than the pericolic region.
Keywords: Torsion, Falciform ligament, Focal fat infarction, Hyperattenuating rim
RESUMO
A torção do apêndice epiplóico do ligamento falciforme, parte do espectro de condições conhecidas como enfarte focal de gordura intra abdominal (IFFI), é uma situação muita rara com menos de 20 casos descritos como imagem até à data. Reportamos um caso de torção do apêndice epiplóico do ligamento falciforme numa mulher de meia-idade, diagnosticado em ecografia e TC abdominal. A TC evidenciou o clássico sinal do anel de hiperdensidade no espaço perihepático anterior, adjacente ao ligamento falciforme. Enfatizamos a importância deste sinal radiológico na TC no reconhecimento de situações de IFFI noutras localizações para além da região pericólica.
Palavras-Chave: Torção, Ligamento falciforme, Enfarte focal de gordura, Anel de hiperdensidade
Introduction
The falciform ligament, a peritoneal fold which divides the right and left lobes of the liver anatomically, may rarely be involved by disease. Fatty appendages of the falciform ligament may very rarely undergo torsion, leading to fat infarction [1, 2]. This type of torsion or infarction, which occurs more commonly in the epiploic appendages or greater omentum and rarely involving the perigastric ligaments (gastrohepatic, gastrosplenic, and falciform), is grouped together as intra-abdominal focal fat infarction (IFFI) [3]. Clinically, these conditions mimic acute surgical conditions and hence need to be differentiated from them. We emphasize the utility of hyperattenuating rim sign on computed tomography (CT) in recognizing IFFI in locations other than the pericolic region, through this case report.
Clinical Case
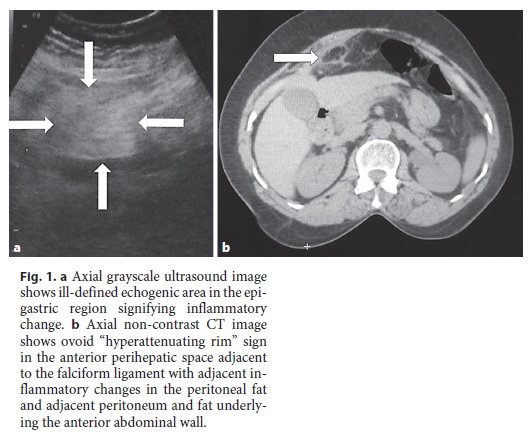
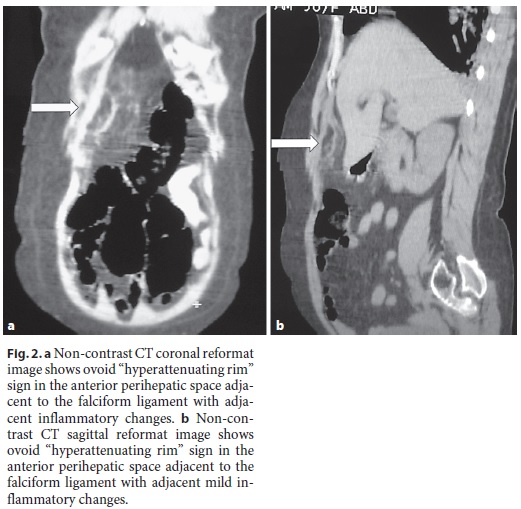
A 56-year-old female patient came with complaints of epigastric pain for 3 days. The pain was continuous in nature, pricking in type, and was not radiating to the back. She had no nausea, vomiting, or fever. On examination, there was epigastric fullness and tenderness in the epigastric and right hypochondrium region. Mild guarding was seen in the epigastric region. Clinical diagnosis was possible perforation with local peritonitis. Blood tests showed mild leukocytosis (15,000 WBCs/mm3), with mild neutrophilia. Liver function tests, C-reactive protein, serum lipase, and amylase were within normal limits. Plain erect radiograph of the abdomen revealed no free air under the diaphragm. Ultrasound of the abdomen revealed an ovoid echogenic area measuring ∼5 × 2 cm in the epigastric region with adjacent inflammatory changes (Fig. 1). There was no fluid collection or free fluid in the peritoneal cavity. Non-contrast CT of the abdomen (done on a Hitachi Eclos CT scanner, Hitachi Corporation, US; 5-mm sections reconstructed to 1.25-mm thickness; pitch of 1.5) revealed classical ovoid hyperattenuating rim sign in the anterior perihepatic space adjacent to the falciformligament with adjacent mild inflammatory changes in the peritoneal fat and adjacent peritoneum and fat underlying the anterior abdominal wall (Fig. 2). The rest of the peritoneal cavity was normal. There was no intraperitoneal free air or fluid collection. The patient did not consent to contrast-enhanced CT study.
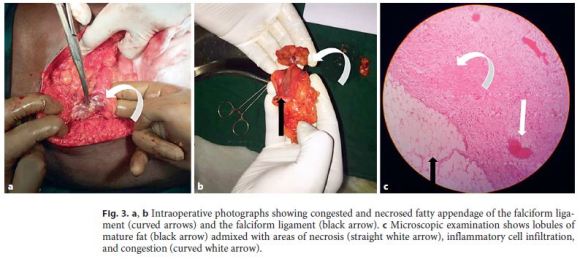
The patient was taken for laparotomy in view of continuing epigastric pain. Intraoperatively, a focal necrotic patch with early gangrenous change was seen in the falciform ligament towards the anterior abdominal wall with omental adhesions adjacent to it (Fig. 3). Inflammation did not extend to the fissure of the falciform ligament. Stomach, large bowel, small bowel, mesentery, and omentum were normal. Falciform ligament was divided from the anterior abdominal wall and the liver and excised in toto. Postoperative period was uneventful and the patient recovered well.
Discussion
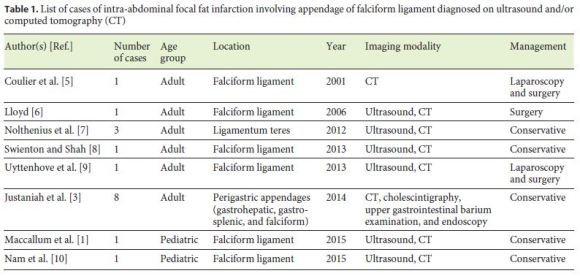
Epiploic appendages are peritoneum-covered pedunculated fatty structures located adjacent to the anterior and posterior tenia coli over the colon wall from the cecum to the rectosigmoid junction [4]. Intra-abdominal focal fat infarction, which occurs more commonly in the epiploic appendages or greater omentum, may rarely involve the perigastric ligaments (gastrohepatic, gastrosplenic, and falciform) also [3]. Of these, torsion and infarction of fatty appendage of the falciform ligament is exceedingly rare with less than 20 cases documented with imaging studies so far (Table 1). There have been very few cases reported before 1977 (based on surgical findings without use of imaging modalities) [1]. The falciform ligament is a double-layered peritoneal fold which extends from the superior edge of the liver to the inferior border of the diaphragm and anatomically divides the right and left lobes of liver. Falciform ligament passes from the parietal peritoneum along the anterior abdominal wall to the visceral peritoneum along the liver surface and divides the superior aspect of the supramesocolic spaces into the right and left subphrenic spaces.
Other pathologies of falciform ligament include internal hernia through congenital defects, congenital/infective/neoplastic cysts, and lipomas [5]. Sometimes, there may be isolated necrosis of the falciform ligament with no other findings [2]. All these pathologies present with similar clinical complaints of epigastric pain with or without constitutional symptoms, closely mimicking other common gastroduodenal and pancreatic diseases. Hence, imaging definitely plays a pivotal role in identifying and differentiating these pathologies. Ultrasound may help locate and identify the pathology owing to real-time dynamic interaction with the patient, but is not adequate in differentiating the various etiologies. CT would be essential in unequivocally diagnosing the gastroduodenal and pancreatic diseases and these rare mimics like IFFI [3]. MRI too may identify the pathology as a primarily fat signal lesion with adjacent inflammation, but does not have a primary role as the CT [8].
IFFI and epiploic appendagitis are usually caused by epiploic appendage torsion with or without spontaneous thrombosis of the central draining vein and are associated with secondary inflammatory changes. IFFI is usually self-limiting in the majority of patients and resolves without treatment within 1 week. Rarely, IFFI may lead to adhesion, peritonitis, necrosis, or abscess formation and calcified peritoneal loose bodies [4]. Sonographic findings in IFFI include hyperechoic, non-compressible lesion at the site of tenderness with or without central hypoechoic area. Color flow is typically absent on Doppler study and helps in differentiating from other inflammatory conditions [4, 8].
CT of IFFI and epiploic appendagitis demonstrates an area of fat density with a thin peripheral rim of hyperattenuation (hyperattenuating rim sign) with or without central dot sign (a punctate hyperdense focus corresponding to the thrombosed vein) [4, 8]. Such appearance close to the colon wall is characteristic for epiploic appendagitis. Similar appearance of hyperattenuating rim sign away from the colon in the perihepatic space prompted us to consider the possibility of similar pathology of fatty appendage unrelated to the colon. Multiplanar reconstruction (MPR) following helical CT (sagittal and coronal reformats) exquisitely depicts the anatomical structure (falciform ligament) and its associated pathology, as demonstrated in our case. Corroborating the anatomical location and classical imaging appearance prompted us to consider the diagnosis of IFFI involving appendage of falciform ligament.
Usually, conservative treatment is adequate, but a few of the reported cases have been operated, primarily due to lesser awareness about the condition and its usually self-limiting nature [5, 6, 9]. Another reason for laparotomy was due to the possibility of necrosis and gangrene as seen in some reports [2]. In this cases also, the surgeons proceeded with surgery despite the unequivocal CT diagnosis of IFFI, due to the increasing severity of abdominal pain in the patient. Their contention was that the necrosed and gangrenous tissue had to be removed, even if the diagnosis of IFFI was correct. However, we feel that, as enunciated by Coulier et al. [5], non-contrast CT with MPR can unequivocally diagnose the IFFI involving appendage of falciform ligament and conservative treatment can be instituted for all the cases instead of proceeding directly to surgery. Better awareness of this condition among the radiologists and the surgeons can be a good step in that direction.
References
1 Maccallum C, Eaton S, Chubb D, Franzi S: Torsion of Fatty Appendage of Falciform Ligament: Acute Abdomen in a Child. Case Rep Radiol DOI: 10.1155/2015/293491. [ Links ]
2 Ozkececı ZT, Ozsoy M, Celep B, Bal A, Polat C: A rare cause of acute abdomen: an isolated falciform ligament necrosis. Case Rep Emerg Med DOI: 10.1155/2014/570751. [ Links ]
3 Justaniah AI, Scholz FJ, Katz DS, Scheirey CD: Perigastric appendagitis: CT and clinical features in eight patients. Clin Radiol. 2014; 69:e531–e537. Erratum in: Clin Radiol 2015;70:457. [ Links ]
4 Coulier B: Contribution of US and CT for diagnosis of intraperitoneal focal fat infarction (IFFI): a pictorial review. JBR-BTR 2010;93:171–185. [ Links ]
5 Coulier B, Cloots V, Ramboux A: US and CT diagnosis of a twisted lipomatous appendage of the falciform ligament. Eur Radiol 2001;11:213–215. [ Links ]
6 Lloyd T: Primary torsion of the falciform ligament: computed tomography and ultrasound findings. Australas Radiol 2006;50:252–254. [ Links ]
7 Nolthenius CJ, Bruinsma WE, Knook MT, Puylaert JB: Acute appendagitis of the ligamentum teres hepatis: clinical, ultrasound, and computed tomographic findings. J Clin Ultrasound 2013;41:108–112. [ Links ]
8 Swienton D, Shah SV: Infarction of a fatty appendage of the falciform ligament – a case report. Eur Radiol DOI: 10.1594/EURORAD/CASE.10799. [ Links ]
9 Uyttenhove F, Leroy C, Nzamushe Lepan Mabla JR, Ernst O: Torsion of a fatty fringe of the falciform ligament, a rare cause of right hypochondrial pain. Diagn Interv Imaging 2013;94:637–639. [ Links ]
10 Nam JG, Choi SH, Kang BS, Kim JY, Kwon WJ: Serial ultrasound and computed tomography findings of torsion of lipomatous appendage of the falciform ligament in a child treated by conservative management. J Korean Soc Radiol 2015;72:368–371. [ Links ]
Statement of Ethics
This article does not contain any studies with animals performed by any of the author(s). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Disclosure Statement
The authors declare that they have no conflict of interest.
* Corresponding author.
Dr. Venkatraman Indiran, MD, DNB
Sree Balaji Medical College and Hospital
#7, Works Road
Chennai 600044 (India)
E-Mail ivraman31@gmail.com
Received: July 25, 2017; Accepted after revision: October 18, 2017














