Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.4 Lisboa ago. 2018
https://doi.org/10.1159/000484440
ORIGINAL ARTICLE
Lymphoproliferative Disorders in Inflammatory Bowel Disease Patients: Is It the Drugs or the Disease?
Doenças Linfoproliferativas e Doença Inflamatória Intestinal: Será o Tratamento ou a Doença?
Carlos Bernardes, Pedro Russo, Diana Carvalho, Joana Saiote, Jaime Ramos
Gastroenterology Department, Centro Hospitalar de Lisboa Central, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Introduction: Systemic inflammatory diseases are related to an increased risk of lymphoproliferative disorders. Although inflammatory bowel disease (IBD) was also associated with these conditions, population-based studies failed to demonstrate this relationship, and most studies only identified a very small number of cases. In the last few years, concerns arose regarding the role of thiopurines and tumour necrosis factor-alpha (TNF-α)-blocking agents in the development of lymphoma, influencing therapeutic decisions in IBD patients. The aim of this study was to describe a case series of IBD patients who developed a lymphoproliferative disorder in our tertiary referral centre. Material and Methods: The clinical records of all IBD patients who were observed in our unit between January 2007 and December 2016 were retrospectively reviewed, and IBD subjects who were diagnosed with a lymphoproliferative disorder were selected. Clinical and demographic data regarding both conditions were collected. Results: Six IBD patients were diagnosed with a lymphoma – 4 Hodgkin lymphomas and 2 B-cell non-Hodgkin lymphomas – of which 3 corresponded to primary colonic lymphomas. Immunohistochemical analysis detected the presence of Epstein-Barr virus in the tumour cells of 2 patients, both of them with Hodgkin lymphomas. Only 2 patients were previously treated with thiopurines or anti-TNF-α drugs; none of the remaining had any history of immunosuppressive treatment. Discussion and Conclusions: Despite major attention being currently focused on the effect of treatment, which may play the main role in the increased susceptibility to lymphoma in IBD patients, and although it may be difficult to demonstrate, IBD itself may contribute to the development of lymphoproliferative disorders, particularly primary intestinal lymphomas.
Keywords: Anti-TNF-α, Inflammatory bowel disease, Lymphoma, Lymphoproliferative disorders, Thiopurines
RESUMO
Introdução: Doenças inflamatórias crónicas estão relacionadas com um aumento de risco de doenças linfoproliferativas. Apesar da doença inflamatória intestinal (DII) também ter sido associada a estas complicações, estudos de base populacional falharam em demonstrar esta relação, e a maioria dos estudos apenas identificou um baixo número de casos. Nos últimos anos, preocupações foram levantadas no que diz respeito ao papel das tiopurinas e dos bloqueadores do factor de necrose tumoral alpha (TNF-α) no desenvolvimento de linfomas, influenciando decisões terapêuticas em doentes com DII. O objectivo deste estudo foi o de descrever uma série de casos de doentes com DII que desenvolveram doenças linfoproliferativas num centro de referência. Material e Métodos: Os registos clínicos dos doentes que foram observados na nossa unidade entre Janeiro de 2007 e Dezembro de 2016 foram retrospectivamente analisados, tendo sido seleccionados os doentes diagnosticados com uma doença linfoproliferativa. Os dados clínicos e demográficos respeitantes a ambas as condições foram colectados. Resultados: Seis doentes com DII foram diagnosticados com linfoma – 4 linfomas de Hodgkin e 2 linfomas não-Hodgkin de células B –, dos quais 3 corresponderam a linfomas primários do cólon. Análise imunohistoquímica detectou a presença do vírus Epstein-Barr nas células tumorais de 2 doentes, ambos com linfoma de Hodgkin. Apenas 2 doentes tinham recebido tratamento prévio com tiopurinas ou agentes anti-TNF-α; nenhum dos restantes tinha qualquer história de terapêutica imunossupressora. Discussão e Conclusão: Apesar da maioria das atenções estar focada no efeito do tratamento, o qual será o principal responsável pela maior susceptibilidade para linfomas em doentes com DII, e apesar da dificuldade em demonstrá-lo, a própria DII poderá contribuir para o desenvolvimento de doenças linfoproliferativas, particular de linfomas intestinais primários.
Palavras-Chave: Anti-TNF-α, Doença inflamatória intestinal, Linfomas, Doenças linfoproliferativas, Tiopurinas
Introduction
The risk of lymphoproliferative disorders is higher among patients with systemic inflammatory diseases [1– 3]. With regard to inflammatory bowel disease (IBD), since the first report of a patient who developed a lymphoma, this association has been discussed by numerous authors [4]. It is widely recognized that inflammation and immune activation may be implicated in the occurrence of lymphoproliferative disorders; in addition, recent reports have illustrated the development of intestinal lymphatic malignancies at sites of active IBD, underlining the possible role of chronic antigen stimulation in the pathogenesis of such conditions [3]. However, controversy has been raised due to the fact that large population-based studies did not show a relationship between those two conditions [5]. Notwithstanding, given the widespread use of biologic and immunosuppressive drugs in IBD treatment, concerns arose regarding the potential role of such agents in the development of lymphoproliferative disorders [6, 7]. The study aims to describe a case series of patients with IBD who were diagnosed with lymphoma in our tertiary referral centre, highlighting and discussing the plausible association between the occurrence of this malignancy and their treatment history.
Material and Methods
Between January 2007 and December 2016, the clinical records of all IBD patients who were observed in our unit were retrospectively reviewed, and IBD subjects who were diagnosed with a lymphoproliferative disorder were selected. Data concerning the timing of diagnosis, therapeutic history – particularly anti-tumour necrosis factor-alpha (TNF-α) or thiopurine use – disease location, behaviour, and clinical course were collected for both conditions. Histological features and the presence of Epstein-Barr virus (EBV) by immunohistochemical analysis in the tumour cells were also assessed.
Results
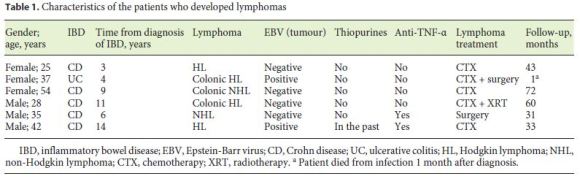
Overall, in a population of 900 subjects, 6 cases of lymphoma were identified: 4 Hodgkin lymphomas (HL) and 2 B-cell non-Hodgkin lymphomas (NHL), in 3 male and 3 female patients, with a median age of 36 years (range 17–45) at diagnosis (Table 1). Of those 6 cases, 3 were primary colonic lymphomas (2 HL and 1 NHL): 1 was located in the ascending (HL) and the remaining 2 in the descending/sigmoid colon (HL and NHL). With regard to the histological subtypes, 2 were lymphocyte-predominant HL while the remaining 2 were classical HL; of the NHL, both were diffuse large B-cell lymphomas, one of germinal centre origin and the other of non-germinal centre B-cell-like phenotype. Five of the subjects had ileocolonic, non-stricturing, non-penetrating Crohn disease, one of them also with perianal involvement, and 1 had left-sided ulcerative colitis. The mean period from IBD onset to the development of lymphoma was 8 years (range 3–14). All patients were in clinical remission when the lymphoproliferative disease was diagnosed, with 4 of them being also in endoscopic remission. Two subjects were receiving maintenance therapy with infliximab, initiated 17 and 80 months before, one of which had also been previously treated with azathioprine (used for 36 months and suspended 7 years before the diagnosis of lymphoma). None of the remaining, including those 3 with primary colonic lymphoma, had any prior use of anti-TNF-α or other immunomodulators. Immunohistochemical analysis detected the presence of EBV in the tumour cells of 2 patients, both of them with HL. Chemotherapy was applied in 5 lymphomas, in combination with surgery and radiotherapy in one case each, and 1 patient was treated with surgery alone. One HL subject died due to infectious complications during the postchemotherapy period. The remaining 5 achieved sustained clinical remission with a median follow-up of 43 months (range 31–72).
Discussion and Conclusions
Our case series shows a significant occurrence of lymphoproliferative disorders among IBD individuals, particularly of primary intestinal lymphomas. Remarkably, despite comprising less than 5% of all gastrointestinal malignancies, primary intestinal lymphomas appear to be more frequent when there is a history of IBD [3, 4, 8]. Analysis of the CESAME (Cancers et sur-risque associé aux maladies inflammatoires intestinales en France) observational cohort identified 14 cases of primary intestinal lymphoproliferative disorders – all NHL – representing an incidence of 0.12/1,000 patient-years and resulting in a standardized incidence ratio of 17.51 (95% confidence interval, 6.43–38.11; p < 0.0001). Importantly, the risk of acquiring lymphomas was significantly higher in patients with thiopurine exposure, in whom the standardized incidence ratio was 49.52. In fact, thiopurines seem to play a major role in the likelihood of developing such a condition in IBD patients [6, 7]. Treatment with those agents was associated with a 4- to 5-fold increase in the risk of lymphoproliferative disorders; this risk appears to rise with longer duration of therapy and to decrease after drug withdrawal [6, 7]. These data, taken together with the identification of predictors of relapse, have encouraged authors to redefine thiopurine treatment specificities, either in combination or as monotherapy [9, 10]. Despite having also been implicated as potential contributing factors for the development of lymphoma in IBD subjects, no clear correlation was found between anti-TNF-α agents and the occurrence of these disorders [11, 12]. A register-based study which included 56,146 patients did not find an increased risk of lymphoproliferative disorders in subjects treated with anti- TNF-α after adjusting the results for confounding factors such as thiopurine use [12]. Nevertheless, in the specific situation of hepatosplenic T-cell lymphoma, the fact that the majority of the identified patients had received combination treatment with TNF-α antagonists and thiopurines cannot be ignored [13]. This assumption suggests that anti-TNF-α therapy may potentiate the risk of thiopurine-related hepatosplenic T-cell lymphoma; however, due to the low frequency of this entity, the relative contribution of each drug is difficult to assess. In order to minimize the susceptibility to these complications, particular precautions should be taken with higher-risk groups, such as young male and elderly patients [11]. Moreover, since EBV is known to be involved in the pathogenesis of lymphoproliferative disorders in immunosuppressed patients, testing for this virus prior to treatment initiation should be considered [11, 14]. Noteworthy, almost half of the primary intestinal lymphomas identified in the CESAME cohort were EBV positive, addressing the influence of the virus in the emergence of this disease [3]. A meaningful fact is that 4 out of our 6 cases corresponded to HL, whose association with IBD is extremely rare [15]. Taking into account the previously reported cases, EBV appears to be particularly common in the tumour cells of that histological type [16]. Although we cannot justify the abnormally high incidence of HL in our population, the fact that both of our EBV-positive tumours were of the Hodgkin type reinforces the potential role of this agent in the pathogenesis of the disease.
Given the relative rarity of these malignancies – illustrated by the detection of only 3 cases of lymphoma in more than 7,000 patients included in one meta-analysis [9] – data resulting from observational studies will be essential to improve our knowledge regarding these topics. With the widespread use of biologic agents and immunomodulators, the number of cases will possibly increase in the future. Interestingly, in our study, only 1 patient had received thiopurines, and even in this case the drug had been suspended 7 years before the diagnosis of lymphoma. In addition, 4 of our patients did not have any past history of anti-TNF-α or immunomodulator treatment. Finally, frequently associated risk factors for the development of lymphoma in IBD patients, such as male gender, early disease onset or age greater than 65 years, were not particularly striking in our series [17].
In conclusion, in spite of being an isolated study with a small number of patients, our results should alert clinicians that, notwithstanding the major influence of the therapeutic history – particularly of thiopurine use – and although it may be difficult to demonstrate, not only the treatment but also the disease itself could contribute to a higher occurrence of lymphoproliferative disorders in IBD patients, specially primary intestinal lymphomas.
References
1 Ekström K, Hjalgrim H, Brandt L, Baecklund E, Klareskog L, Ekbom A, Askling J: Risk of malignant lymphomas in patients with rheumatoid arthritis and in their first-degree relatives. Arthritis Rheum 2003;48:963–970. [ Links ]
2 Dionigi G, Annoni M, Rovera F, Boni L, Villa F, Castano P, Bianchi V, Dionigi R: Primary colorectal lymphomas: review of the literature. Surg Oncol 2007;16(suppl 1):S169–S171. [ Links ]
3 Sokol H, Beaugerie L, Maynadié M, Laharie D, Dupas JL, Flourié B, Lerebours E, Peyrin- Biroulet L, Allez M, Simon T, Carrat F, Brousse N; CESAME Study Group: Excess primary intestinal lymphoproliferative disorders in patients with inflammatory bowel disease. Inflamm Bowel Dis 2012;18:2063–2071. [ Links ]
4 Bargen J: Chronic ulcerative colitis associated with malignant disease. Arch Surg 1928;8793:1307–1311. [ Links ]
5 Lewis JD, Bilker WB, Brensinger C, Deren JJ, Vaughn DJ, Strom BL: Inflammatory bowel disease is not associated with an increased risk of lymphoma. Gastroenterology 2001;121:1080–1087. [ Links ]
6 Beaugerie L, Brousse N, Bouvier AM, Colombel JF, Lémann M, Cosnes J, Hébuterne X, Cortot A, Bouhnik Y, Gendre JP, Simon T, Maynadié M, Hermine O, Faivre J, Carrat F; CESAME Study Group: Lymphoproliferative disorders in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Lancet 2009;374:1617–1625. [ Links ]
7 Khan N, Abbas AM, Lichtenstein GR, Loftus EV Jr, Bazzano LA: Risk of lymphoma in patients with ulcerative colitis treated with thiopurines: a nationwide retrospective cohort study. Gastroenterology 2013;145:1007– 1015. [ Links ]
8 Herrmann R, Panahon AM, Barcos MP, Walsh D, Stutzman L: Gastrointestinal involvement in non-Hodgkins lymphoma. Cancer 1980;46:215–222. [ Links ]
9 Torres J, Burisch J, Riddle M, Dubinsky M, Colombel JF: Preclinical disease and preventive strategies in IBD: perspectives, challenges and opportunities. Gut 2016;65:1061–1069. [ Links ]
10 Beaugerie L: Lymphoma: the bête noire of the long-term use of thiopurines in adult and elderly patients with inflammatory bowel disease. Gastroenterology 2013;145:927–930. [ Links ]
11 Williams CJ, Peyrin-Biroulet L, Ford AC: Systematic review with meta-analysis: malignancies with anti-tumour necrosis factor-α therapy in inflammatory bowel disease. Aliment Pharmacol Ther 2014;39:447–458. [ Links ]
12 Nyboe Andersen N, Pasternak B, Basit S, Andersson M, Svanström H, Caspersen S, Munkholm P, Hviid A, Jess T: Association between tumor necrosis factor alpha antagonists and risk of cancer in patients with inflammatory bowel disease. JAMA 2014;311:2406–2413. [ Links ]
13 Kotlyar DS, Osterman MT, Diamond RH, Porter D, Blonski WC, Wasik M, Sampat S, Mendizabal M, Lin MV, Lichtenstein GR: A systematic review of factors that contribute to hepatosplenic T-cell lymphoma in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2011;9:36–41.e1. [ Links ]
14 Posthuma EF, Westendorp RG, van der Sluys Veer A, Kluin-Nelemans JC, Kluin PM, Lamers CB: Fatal infectious mononucleosis: a severe complication in the treatment of Crohns disease with azathioprine. Gut 1995;36:311–313. [ Links ]
15 Castrellon A, Feldman PA, Suarez M, Spector S, Chua L, Byrnes J: Crohns disease complicated with primary gastrointestinal Hodgkins lymphoma presenting with small bowel perforation. J Gastrointestin Liver Dis 2009;18:359–361. [ Links ]
16 Kumar S, Fend F, Quintanilla-Martinez L, Kingma DW, Sorbara L, Raffeld M, Banks PM, Jaffe ES: Epstein-Barr virus-positive primary gastrointestinal Hodgkins disease: association with inflammatory bowel disease and immunesuppression. Am J Surg Pathol 2000;24:66–73. [ Links ]
17 Magro F, Peyrin-Biroulet L, Sokol H, Aldeger X, Costa A, Higgins PD, Joyce JC, Katsanos KH, Lopez A, de Xaxars TM, Toader E, Beaugerie L: Extra-intestinal malignancies in inflammatory bowel disease: results of the 3rd ECCO Pathogenesis Scientific Workshop (III). J Crohns Colitis 2014;8:31–44. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors declare no conflicts of interest.
* Corresponding author.
Dr. Carlos Bernardes
Gastroenterology Department, Centro Hospitalar de Lisboa Central
Rua Alfredo Inácio Ramos da Silva, 28, 3° E.
PT–2730-203 Barcarena (Portugal)
E-Mail carlosfbernardes@gmail.com
Received: August 24, 2017; Accepted after revision: October 18, 2017
Author Contributions
All authors have contributed to the study conception and design, data analysis, and interpretation. Carlos Bernardes prepared the manuscript; Pedro Russo, Diana Carvalho, Joana Saiote, and Jaime Ramos reviewed the manuscript.














