Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.3 Lisboa jun. 2018
https://doi.org/10.1159/000484868
ORIGINAL ARTICLE
Mortality Associated with Hepatobiliary Disease in Portugal between 2006 and 2012
Mortalidade por doença hepatobiliar em Portugal entre 2006 e 2012
Manuel Coelho da Rocha, Rui T. Marinho, Teresa Rodrigues
Department of Gastroenterology and Hepatology, Hospital de Santa Maria – Centro Hospitalar Lisboa Norte, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Introduction: Hepatobiliary disease is becoming a major public health problem, and recent data suggest that the burden of liver disease is higher than previously thought. Our aim was to quantify the mortality from hepatobiliary disease in Portugal and to compare this with the mortality related to other causes over a 7-year period (2006–2012). Materials and Methods: A statistical analysis of mortality data according to cause, sex, age, and region from the National Statistics Institute in Portugal was carried out. The data related to 14 causes of death, the most frequent of which were alcoholic liver disease (ALD) (International Classification of Diseases code K70), unspecified cirrhosis of liver (UCL) (K74.6), hepatocellular carcinoma (HCC) (C22.0), unspecified malignant neoplasm of liver (C22.9), and cholangiocarcinoma (C22.1). Results: Between 2006 and 2012, 18,279 deaths (24.5/100,000) from hepatobiliary disease were registered in Portugal, constituting the 8th leading cause of death. The main causes of death from hepatobiliary disease were ALD (7.1/100,000), UCL (5.5/100,000), and HCC (4.3/100,000), with a male predominance (72%). ALD was the main aetiology in younger age groups (40–65 years), while primary neoplasms of the liver and the intrahepatic bile ducts were predominant in the elderly (>80 years). The mortality related to HCC increased by 66% between 2006 and 2012. Conclusion: These data outline the burden of hepatobiliary disease in Portugal (8th cause of death) and highlight a potential impact on economic productivity.
Keywords: Hepatobiliary disease, Mortality, Alcoholic liver disease, Hepatocellular carcinoma
RESUMO
Introdução: A doença hepatobiliar representa um importante problema para a saúde pública e dados recentes sugerem que o seu impacto é superior ao que se pensava. O nosso objetivo foi quantificar a mortalidade por doença hepatobiliar em Portugal e compará-la com a mortalidade por outras causas, durante um período de sete anos (2006–2012). Materiais e Métodos: Foi feita uma análise estatística da mortalidade por doença hepatobiliar em Portugal, de acordo com a causa de morte, sexo, idade e região geográfica, com dados fornecidos pelo Instituto Nacional de Estatística. Foram estudadas 14 causas de morte, sendo as principais a doença hepatica alcoólica (código da Classificação Internacional de Doenças, 10a versão: K70), cirrose hepatica não especificada (K74.6), carcinoma hepatocelular (C22.0), neoplasia maligna do fígado não especificada (C22.9) e colangiocarcinoma (C22.1). Resultados: Entre 2006 e 2012 foram registadas 18,279 mortes (24.5/100,000) por doença hepatobiliar em Portugal, sendo a 8a causa de morte no país. As principais causas de morte por doença hepatobiliar foram a doença hepatica alcoólica (7.1/100,000), cirrose hepática não especificada (5.5/100,000) e carcinoma hepatocelular (4.3/ 100,000), com predominância no sexo masculino (72%). A doença hepática alcoólica foi a principal causa de morte nos grupos etários mais jovens (40–65 anos), enquanto que a neoplasia do fígado e vias biliares intra-hepáticas foi a principal causa nos idosos (>80 anos). A mortalidade por carcinoma hepatocelular aumentou 66% de 2006 a 2012. Conclusões: Este estudo salienta o impacto que a doença hepatobiliar tem em Portugal (8a causa de morte), o que representa um potencial impacto para a produtividade do país.
Palavras-Chave: Doença hepatobiliar, Mortalidade, Doença hepática alcoólica, Carcinoma hepatocelular
Introduction
Hepatobiliary disease is becoming a major public health problem, and recent data suggest that the burden of liver disease is higher than previously thought [1]. If we aggregate mortality data from chronic liver conditions such as hepatitis C, hepatitis B, and hepatocellular carcinoma (HCC), the burden of liver-related mortality is much higher, with around 2 million deaths occurring each year [2–4]. There is also evidence to suggest that mortality related to liver cirrhosis and liver cancer has increased over the last decade [5]. According to Eurostat figures, liver disease was the 7th leading cause of death in 2013, with noticeably higher rates in certain countries [6]. However, very few studies have analysed mortality related to chronic liver conditions such as liver cirrhosis and HCC by aggregating data from major causes, namely excessive alcohol intake, hepatitis B and C, and metabolic syndrome [7].
According to the World Health Organization, hepatobiliary disease is one of the top ten causes of death in Portugal [8]. However, data remain insufficient as the burden of liver disease is currently based on information obtained through hospital admissions from liver cirrhosis [9, 10] and HCC [11]. Unlike other countries, aggregated mortality data for hepatobiliary disease in Portugal are yet to be communicated.
One of the main causes of death from hepatobiliary disease is liver cirrhosis due to alcohol consumption. Mortality from liver disease in Europe is closely related to the pattern of alcohol consumption [12], and Portugal is among the 15 countries with the highest alcohol consumption per capita in the world [13]. Chronic viral hepatitis is another important cause of hepatobiliary mortality, particularly chronic hepatitis B and C, due to progression to cirrhosis and/or HCC. In Portugal, the prevalence of chronic carriers of hepatitis B virus (HBV) and hepatitis C virus (HCV) is approximately 1% [14, 15]. HCC accounts for approximately 80% of all primary neoplasms of the liver and is the 6th leading cause of cancer death among men [16]. In Portugal, high alcohol consumption and hepatitis C are the two main causes of HCC [17, 18].
Other emerging causes of chronic liver disease with increasing importance are non-alcoholic fatty liver disease (NAFLD), associated with obesity and type 2 diabetes [19], and liver disease in patients with human immunodeficiency virus (HIV) infection, mainly caused by hepatitis C due to the efficacy of highly active antiretroviral therapy and consequently longer survival of these patients [20, 21].
Spanning a 7-year period (2006–2012) and including fourteen hepatobiliary disease entities, this study was conducted to assess mortality related to liver disease in Portugal compared with mortality from other causes.
Materials and Methods
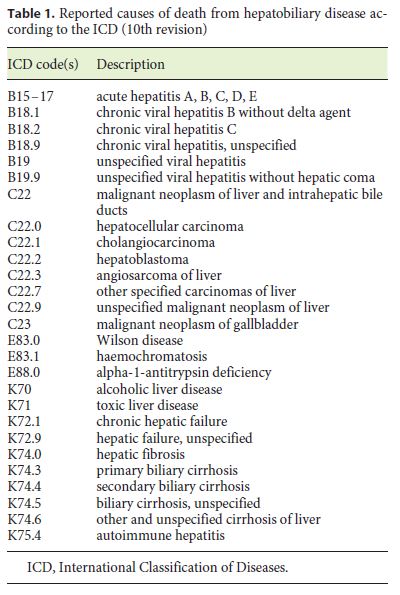
Mortality data from all main causes of death in Portugal were provided by the National Statistics Institute according to cause (International Classification of Diseases, 10th revision, version 2014), sex, age, and region. The reported causes of death from hepatobiliary disease in Portugal are showed in Table 1.
The National Statistics Institutes statistical confidentiality framework stood as the main limitation of this study. As such, occurrences of less than three deaths were unavailable for study inclusion.
Statistical analysis was conducted using the IBM SPSS® (Version 21) software, and charts and tables were produced using Microsoft Word 2007® and Microsoft Excel 2007®, respectively. To calculate the number of deaths from liver disease in patients with HIV infection, 15% of the total number of deaths from HIV infection were considered to be related to liver disease, as reported in the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study [20].
Results
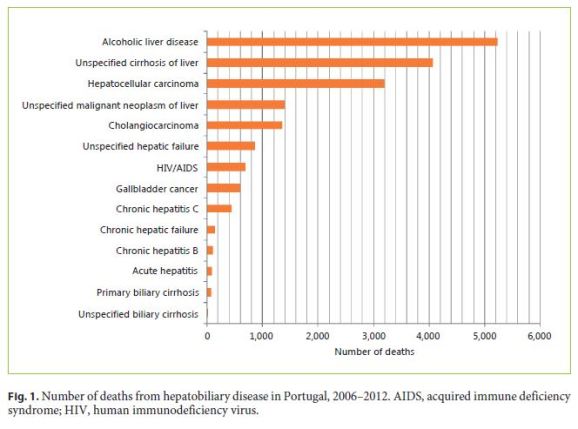
A total of 18,279 deaths (24.5/100,000) from hepatobiliary disease were reported between 2006 and 2012. The main causes were alcoholic liver disease (ALD) (7.1/100,000), unspecified cirrhosis of liver (UCL) (5.5/100,000), and HCC (4.3/100,000) (Fig. 1). When comparing the mortality rates from 2006 to those from 2012, the mortality from ALD and HCC increased by 6 and 66%, respectively, while the mortality from UCL decreased by 26%.
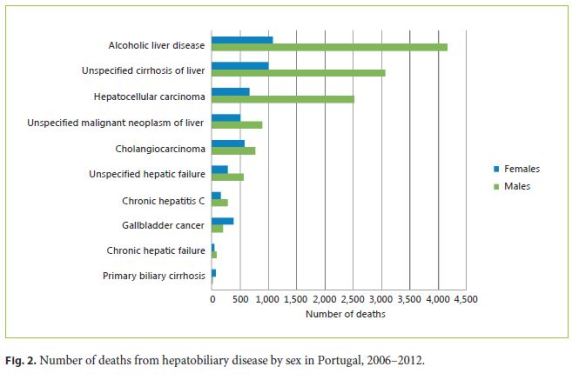
Sex
All-cause hepatobiliary disease mortality was higher in males (72%) compared with females, with a male:female (M:F) ratio of 2.6: 1. The three leading causes of death for both sexes were ALD (M: 11.7/100,000; F: 2.8/100,000; M:F ratio: 3.9: 1), UCL (M: 8.6/100,000; F: 2.6/100,000; M:F ratio: 3.0: 1), and HCC (M: 7.1/100,000; F: 1.8/100,000; M:F ratio: 3.7: 1) (Fig. 2).
Age
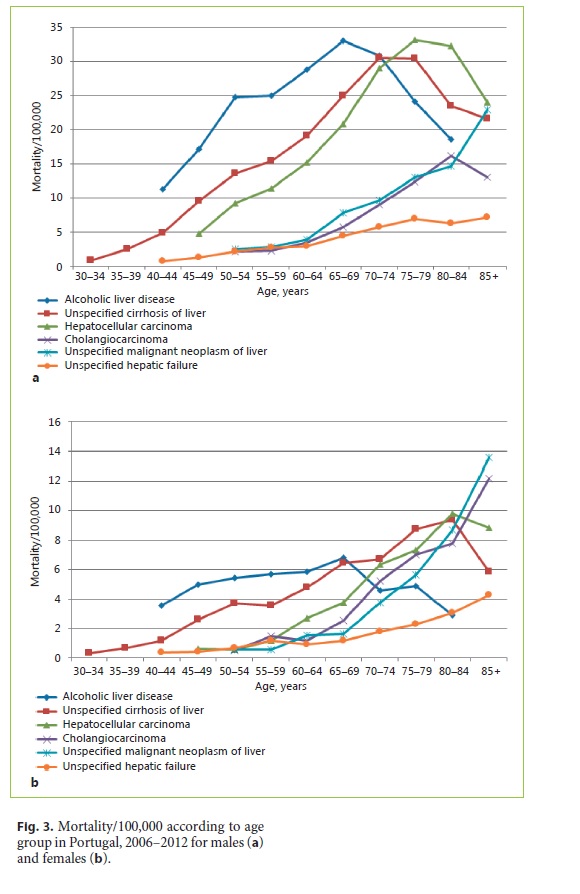
Considering all causes of hepatobiliary disease included in our study, mortality was highest in males 75–79 years of age (120.1/100,000) and in females ≥85 years of age (44.8/100,000) between 2006 and 2012.
ALD showed greater mortality in the middle-age groups (40–65 years), while mortality from primary neoplasms of the liver and intrahepatic bile ducts occurred predominantly in the elderly (>80 years). Mortality from UCL and HCC occurred predominantly in the 8th and 9th decade of life, respectively (Fig. 3).
Region
Portugal is a country located in Western Europe. The regional distribution of the three main causes of death from hepatobiliary disease in Portugal was as follows:
ALD. Mortality was highest in the archipelago of Madeira (11.3/100,000). In mainland Portugal there was a north-south gradient in mortality rates of 8.4/100,000 and 4.3/100,000, respectively (Fig. 4a).
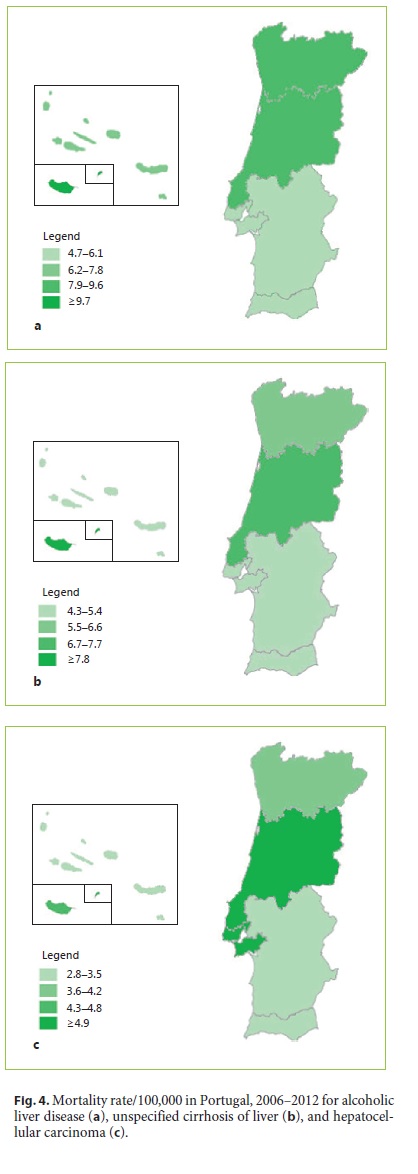
UCL. Once again, mortality was higher in the archipelago of Madeira (8.8/100,000) compared with mainland Portugal. In mainland Portugal, mortality from UCL was highest in the centre of the country, with a rate of 6.9/100,000, and lowest in the south (4.3/100,000) (Fig. 4b).
HCC. Mortality from HCC was highest in the centre of the country, with rates of around 5.0/100,000, compared to the south with rates of around 3.0/100,000 (Fig. 4c).
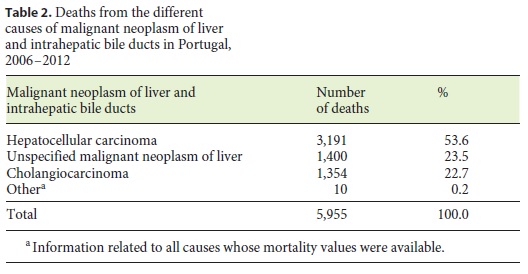
Malignant Neoplasm of Liver and Intrahepatic Bile Ducts (C22)
Considering the mortality from the various types of primary neoplasms of the liver and intrahepatic bile ducts, HCC was the most frequent (53.6%), followed by unspecified malignant neoplasm of liver (23.5%) and cholangiocarcinoma (22.7%) (Table 2).
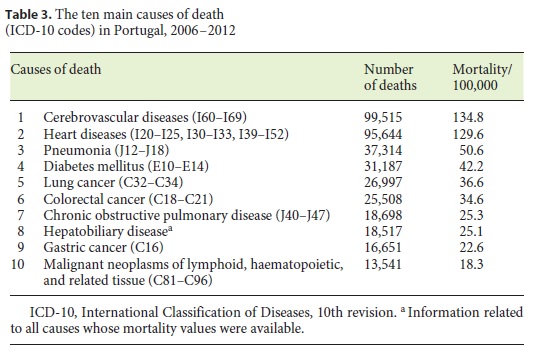
Top 10 Causes of Death in Portugal
Hepatobiliary disease was the 8th leading cause of death in Portugal between 2006 and 2012, with a mortality rate of 25.1/100,000, almost equivalent to the 7th leading cause of death, chronic obstructive pulmonary disease (Table 3).
Discussion and Conclusions
Current evidence suggests that the burden of liver-related mortality is increasing [22]. However, there are very few studies that consider mortality from liver disease by aggregating death rates from different causes such as liver cirrhosis, liver cancer, viral hepatitis, and HBV/HCV coinfection with HIV. In this study, in which mortality from fourteen types of hepatobiliary disease was aggregated, the disease was found to be the 8th leading cause of death in Portugal, consistent with results from Europe [6] and Brazil [23].
The main cause of death from hepatobiliary disease in Portugal is ALD (7.1/100,000), which is most predominant in males between 40 and 65 years of age. This was expected, as alcohol consumption in Portugal is higher in males than females [24] and is most common between the ages of 25 and 54 years (80% of consumers) [25]. It is important to emphasise that ALD in males between 50 and 65 years of age has a mortality rate of 25–30/100,000, and so has the potential of having a severe impact on national productivity and economy [26–28].
The 2nd leading cause of death from liver disease in Portugal is UCL (5.5/100,000), with chronic hepatitis B and C and NAFLD possibly contributing to this category. The mortality from hepatitis B and C is lower than expected when considering the prevalence estimated for the disease in Portugal (1%) [14, 29, 30]. Mortality fromNAFLD in Portugal is unknown. However, its burden is probably high due to an increasing prevalence of obesity, which is directly related to the development of NAFLD [31]. The proportion of adults who are overweight or obese in Portugal is known to be rising and has increased from 49.6% in 1995–1998 to 53.6% in 2003–2005 [32].
In Portugal, mortality from HCC increased by 66% between 2006 and 2012. This may be related to the longer survival of patients with liver cirrhosis due to better prevention and treatment, which in turn increases the possibility of developing HCC (by approximately 4% for each additional year of life) [33]. In addition, diagnostic accuracy has improved, mainly due to the widespread use of ultrasonography and determination of α-fetoprotein levels, which has led to better detection of HCC in cirrhotic patients [17].
As expected, HCC is predominant in males due to a higher incidence of liver cirrhosis. Furthermore, there is evidence showing an increased incidence of viral hepatitis in males (M:F ratio: hepatitis B, 1.5: 1; hepatitis C, 2: 1) [34] and therefore an increased susceptibility to the development of HCC [35, 36].
In 2007, the countries of the European Union with the highest HCC mortality rates in males were France (6.2/ 100,000), Spain (4.9/100,000), and Italy (4.0/100,000) [37]. According to this study, the HCC mortality rate in males in 2007 was 5.8/100,000, suggesting that Portugal is among the European countries with the highest mortality from HCC.
With regards to cholangiocarcinoma, the European countries with the highest mortality rates in 2008 included Germany, France, and the United Kingdom (males: 1.2–1.5/100,000; females: 0.8–1.1/100,000) [37]. According to our study, the mortality rate from cholangiocarcinoma in Portugal in the same year was 1.6/100,000 in males and 1.4/100,000 in females. Therefore, Portugal also seems to be one of the European countries with the highest mortality rates from cholangiocarcinoma.
In this study, HCC was the most frequent cause of death from malignant neoplasms of the liver and intrahepatic bile ducts (53.6%). Considering that HCC corresponds to 80% of primary tumours of the liver and incidence is almost the same as mortality [38], we expected a higher percentage of deaths from HCC in this group. However, it was observed that 23.5% of all deaths from malignant neoplasms of the liver and intrahepatic bile ducts were coded as unspecified malignant neoplasm of liver, suggesting that HCC is underdiagnosed in Portugal.
Regarding regional distribution, the mortality from liver cirrhosis was highest in the archipelago of Madeira. This is likely to be due to high alcohol consumption and historically high levels of intravenous drug abuse. In mainland Portugal there was a north-south gradient in ALD mortality which is consistent with the pattern of alcohol consumption [25]. The higher mortality rates registered in the north of the country are also related to the location of the reference centres. These centres are located in the north (Porto) and centre (Coimbra and Lisbon) of Portugal and are where many of the patients died.
In conclusion, from 2006 to 2012, hepatobiliary disease was the 8th leading cause of death in Portugal. The main causes were ALD, UCL, and HCC, with the highest predominance in males. In particular, ALD represents an important problem in males between 50 and 65 years old, with a potential impact on national productivity. Since almost all causes of liver disease are preventable, we believe that this study highlights an urgent unmet need for a strategic policy to prevent liver-related deaths in Portugal.
References
1 World Health Organization: The top 10 causes of death in the world. http://www.who.int/mediacentre/factsheets/fs310/en/ (accessed November 1, 2014). [ Links ]
2 Thrift AP, El-Serag HB, Kanwal F: Global epidemiology and burden of HCV infection and HCV-related disease. Nat Rev Gastroenterol Hepatol 2017;14:122–132. [ Links ]
3 Chang MS, Nguyen MH: Epidemiology of hepatitis B and the role of vaccination. Best Pract Res Clin Gastroenterol 2017;31:239– 247. [ Links ]
4 Ghouri YA, Mian I, Rowe JH: Review of hepatocellular carcinoma: epidemiology, etiology, and carcinogenesis. J Carcinog 2017;16:1. [ Links ]
5 Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al: Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095–2128. [ Links ]
6 European Commission: Eurostat Pocketbooks: European Social Statistics – 2013 edition. Luxembourg, Publications Office of the European Union, 2013. [ Links ]
7 Blachier M, Leleu H, Peck-Radosavljevic M, Valla DC, Roudot-Thoraval F: The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol 2013;58:593–608. [ Links ]
8 World Health Organization: The world health report 2004: changing history. Geneva, World Health Organization, 2004. [ Links ]
9 Cortez-Pinto H, Marques-Vidal P, Monteiro E: Liver disease-related admissions in Portugal: clinical and demographic pattern. Eur J Gastroenterol Hepatol 2004;16:873–877. [ Links ]
10 Ratib S, Fleming KM, Crooks CJ, Aithal GP, West J: 1 and 5 year survival estimates for people with cirrhosis of the liver in England, 1998–2009: a large population study. J Hepatol 2014;60:282–289. [ Links ]
11 Marinho RT, Giria J, Moura MC: Rising costs and hospital admissions for hepatocellular carcinoma in Portugal (1993–2005). World J Gastroenterol 2007;13:1522–1527. [ Links ]
12 Mäkelä P, Gmel G, Grittner U, Kuendig H, Kuntsche S, Bloomfield K, et al: Drinking patterns and their gender differences in Europe. Alcohol 2006;41:8–18. [ Links ]
13 World Health Organization: Global status report on alcohol and health, 2011. Geneva, World Health Organization, 2011. [ Links ]
14 Viral Hepatitis Prevention Board: Viral hepatitis: burden and prevention of viral hepatitis in Portugal, Lisbon, November 18–19, 2010. Antwerp, Viral Hepatitis Prevention Board, 2011. [ Links ]
15 Esteban JI, Sauleda S, Quer J: The changing epidemiology of hepatitis C virus infection in Europe. J Hepatol 2008;48:148–162. [ Links ]
16 Torre LA, Bray F, Siegel RL, Ferlay J, Lortet- Tieulent J, Jemal A: Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87–108. [ Links ]
17 Chuang SC, La Vecchia C, Boffetta P: Liver cancer: descriptive epidemiology and risk factors other than HBV and HCV infection. Cancer Lett 2009;286:9–14. [ Links ]
18 Martins A, Cortez-Pinto H, Marques-Vidal P, Mendes N, Silva S, Fatela N, et al: Treatment and prognostic factors in patients with hepatocellular carcinoma. Liver Int 2006;26:860– 867. [ Links ]
19 Benedict M, Zhang X: Non-alcoholic fatty liver disease: an expanded review. World J Hepatol 2017;9:715–732. [ Links ]
20 Weber R, Sabin CA, Friis-Møller N, Reiss P, El-Sadr WM, Kirk O, et al: Liver-related deaths in persons infected with the human immunodeficiency virus: the D:A:D study. Arch Intern Med 2006;166:1632–1641. [ Links ]
21 Klein MB, Rockstroh JK, Wittkop L: Effect of coinfection with hepatitis C virus on survival of individuals with HIV-1 infection. Curr Opin HIV AIDS 2016;11:521–526. [ Links ]
22 All-Party Parliamentary Hepatology Group: The All-Party Parliamentary Hepatology Group (APPHG) inquiry into improving outcomes in liver disease. London, All-Party Parliamentary Hepatology Group, 2014. [ Links ]
23 Nader LA, De Mattos AA, Bastos GA: Burden of liver disease in Brazil. Liver Int 2014;34:844–849. [ Links ]
24 Jepsen P, Vilstrup H, Sørensen HT: Alcoholic cirrhosis in Denmark – population-based incidence, prevalence, and hospitalization rates between 1988 and 2005: a descriptive cohort study. BMC Gastroenterol 2008;8:3. [ Links ]
25 Balsa C, Vital C, Pascueiro L: O Consumo de bebidas alcoólicas em Portugal, prevalências e padrões de consumo, 2001–2007. Report, da Droga e da Toxicodependência, Universidade Nova de Lisboa, Portugal, 2011. [ Links ]
26 Marinho RT, Duarte H, Gíria J, Nunes J, Ferreira A, Velosa J: The burden of alcoholism in fifteen years of cirrhosis hospital admissions in Portugal. Liver Int 2015;35:746–755. [ Links ]
27 Pinho I, Santos JV, Dinis-Ribeiro M, Freitas A: Burden of digestive diseases in Portugal: trends in hospitalizations between 2000 and 2010. Eur J Gastroenterol Hepatol 2015;27:279–289. [ Links ]
28 Vitor S, Marinho RT, Gíria J, Velosa J: An observational study of the direct costs related to hospital admissions, mortality and premature death associated with liver disease in Portugal. BMC Res Notes 2016;9:62. [ Links ]
29 Marinho RT, Moura MC, Giria JA, Ferrinho P: Epidemiological aspects of hepatitis C in Portugal. J Gastroenterol Hepatol 2001;16:1076–1077. [ Links ]
30 Ministério da Saúde: Avaliação do programa nacional de vacinação. 2° Inquérito serológico nacional Portugal continental 2001–2002. Report, Direcção Geral da Saúde, Lisboa, 2004. [ Links ]
31 Bertot LC, Adams LA: The natural course of non-alcoholic fatty liver disease. Int J Mol Sci 2016;17:E774. [ Links ]
32 Do Carmo I, Dos Santos O, Camolas J, Vieira J, Carreira M, Medina L, et al: Overweight and obesity in Portugal: national prevalence in 2003–2005. Obes Rev 2008;9:11–19. [ Links ]
33 Bolondi L, Sofia S, Siringo S, Gaiani S, Casali A, Zironi G, et al: Surveillance programme of cirrhotic patients for early diagnosis and treatment of hepatocellular carcinoma: a cost effectiveness analysis. Gut 2001;4:251–259. [ Links ]
34 European Centre for Disease Prevention and Control: Annual epidemiological report 2012: reporting on 2010 surveillance data and 2011 epidemic intelligence data. Stockholm, European Centre for Disease Prevention and Control, 2013. [ Links ]
35 Liu WH, Yeh SH, Lu CC, Yu SL, Chen HY, Lin CY, et al: MicroRNA-18a prevents estrogen receptor-alpha expression, promoting proliferation of hepatocellular carcinoma cells. Gastroenterology 2009;136:683–693. [ Links ]
36 Yang WJ, Chang CJ, Yeh SH, Lin WH, Wang SH, Tsai TF, et al: Hepatitis B virus X protein enhances the transcriptional activity of the androgen receptor through c-Src and glycogen synthase kinase-3beta kinase pathways. Hepatology 2009;49:1515–1524. [ Links ]
37 Bertuccio P, Bosetti C, Levi F, Decarli A, Negri E, La Vecchia C: A comparison of trends in mortality from primary liver cancer and intrahepatic cholangiocarcinoma in Europe. Ann Oncol 2013;24:1667–1674. [ Links ]
38 Are C, Meyer B, Stack A, Ahmad H, Smith L, Qian B, et al: Global trends in the burden of liver cancer. J Surg Oncol 2017;115:591–602. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
There are no conflicts of interest to declare for this work.
* Corresponding author.
Dr. Manuel Coelho da Rocha
Department of Gastroenterology and Hepatology
Hospital de Santa Maria – Centro Hospitalar Lisboa Norte
Avenida Professor Egas Moniz, PT–1649-035 Lisbon (Portugal)
E-Mail manel.rocha@gmail.com
Received: April 27, 2017; Accepted after revision: August 24, 2017
Acknowledgements
The authors would like to acknowledge the editorial assistance provided by Creston Unlimited, paid for by Gilead Sciences Ltd. However, Gilead Sciences Ltd had no input into the design, conduct, or reporting of the study. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.














