Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.2 Lisboa abr. 2018
https://doi.org/10.1159/000479591
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
A Rare Cause of Multisegmental Gastrointestinal Ulceration
Uma Causa Rara de Ulceração Multifocal do Tubo Digestivo
Joana Carmo, Miguel Bispo, Cristina Chagas
Gastroenterology Department, Hospital de Egas Moniz – Centro Hospitalar de Lisboa Ocidental, Lisbon, Portugal
* Corresponding author.
Keywords: Endoscopy, Gastrointestinal tract, Gastrointestinal lymphoma
Palavras-Chave: Endoscopia digestiva, Tubo digestivo, Linfoma gastro-intestinal
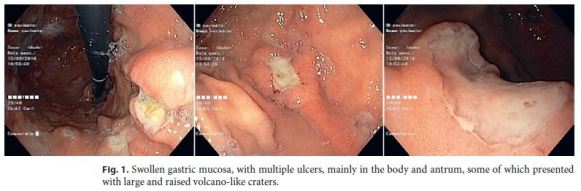
The authors present the case of a 62-year-old Caucasian female with a medical history of abdominal surgery, at another institution, due to bowel perforation with peritonitis, presumably owing to a nonspecific inflammatory process. The postoperative outcome was uneventful. During 3 months, she was completely asymptomatic, namely without fever, night sweats, or weight loss, and then, 3 months later, she was admitted due to acute onset of abdominal pain and fever. On physical examination, she presented abdominal pain and tenderness on the right lower abdominal quadrant without palpable organomegaly or lymph nodes. Acute appendicitis was suspected on the initial ultrasound examination. She was started on antibiotic therapy with lowering of the C-reactive protein but without remission of the fever. HIV and Epstein-Barr virus serologies were negative. She was submitted to an abdominal computed tomography scan that showed a thickened gastric antrum and terminal ileum with a 3-cm pericecal abscess. An upper gastrointestinal endoscopy was then performed and showed swollen gastric mucosa and multiple ulcers scattered in the body and antrum, some of which presented with large and raised volcano-like craters (Fig. 1). An ileocolonoscopy documented multiple ulcers in all colonic segments, some of them large, confluent, and excavated, with raised borders, the largest in the cecum and splenic flexure (Fig. 2). Biopsies were taken on both of these exams, and the histopathological examination showed extensive ulceration and epithelial permeation by a diffuse lymphocytic infiltrate with small- and medium-size cells (CD56+, CD8+, CD3+, CD4+/–, CD20–, CD79a–, and PAX5–) (Fig. 3). Flow cytometry of the gastric biopsies revealed an identical monoclonal lymphocyte population. The patient had an enteropathy-associated natural killer/T-cell lymphoma (type II), an unusual presentation of this rare disease with involvement of the stomach and small and largebowel. Serologic tests for celiac sprue were negative. Further studies excluded bone marrow involvement. Following the resolution of the pericecal abscess with antibiotic treatment, the patient started chemotherapy (CHOP). Six months later, due to disease progression with pulmonary and endometrium involvement, second-line chemotherapy was started.

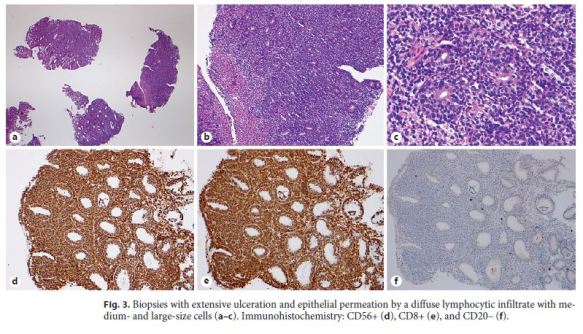
Despite being the most frequently extranodal site involved in by lymphomas, primary lymphomas of the gastrointestinal tract are rare and account for only 1–4% of the gastrointestinal malignancies [1]. Almost 90% are B-cell lineage lymphomas; therefore, T-cell and Hodgkin lymphomas are even rarer [1]. Enteropathy-associated T-cell lymphoma accounts for 1.4% of all lymphomas. It is more frequent in men and in the sixth to seventh decade of life [2, 3]. The vast majority of cases present with small bowel involvement (90%), while the colon (16%) and stomach (8%) are not so frequently affected [2]. There are 2 types: type I is the classic and most common form [4]. It is strongly associated with celiac disease, thus being more frequent in Northern Europe [2, 4]. Type II represents only 10–20% of all cases of this rare disease with an incidence of 0.5–1 per million per year [2]. It occurs sporadically and is more frequent in Asian countries [4]. In type II, bowel perforation is often the form of presentation, but clinical, endoscopic, and morphologic data are not enough for the differential diagnosis [3]. Epidemiological patterns could be helpful, but immunohistochemistry (CD56) is crucial for this diagnosis [2, 3]. The absence of positivity for Epstein-Barr virus is also important to distinguish this disease from other natural killer/T-cell lymphomas (nasal type). Both subtypes are aggressive and have a poor prognosis with a median survival of 10 months [4].
References
1 Ghimire P, Wu GY, Zhu L: Primary gastrointestinal lymphoma. World J Gastroenterol 2011;17:697–707. [ Links ]
2 Rand AJ, Cardona DM, Proia AD, Lagoo AS: Clinically undiagnosed enteropathy associated T-cell lymphoma type II presenting with prolonged lower gastrointestinal tract symptoms: report of an autopsy case and review of diagnostic challenges and clinicopathological correlation. J Gastrointest Oncol 2013;4:103– 108. [ Links ]
3 Chan JK, Chan AC, Cheuk W, Wan SK, Lee WK, Lui YH, Chan WK: Type II enteropathy-associated T-cell lymphoma: a distinct aggressive lymphoma with frequent γδ T-cell receptor expression. Am J Surg Pathol 2011;35:1557–1569. [ Links ]
4 Arps DP, Smith LP: Classic versus type II enteropathy-associated T-cell lymphoma. Arch Pathol Lab Med 2013;137:1227–1231. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors confirm that there are no conflicts of interest associated with this publication, and there has been no financial support for this work.
* Corresponding author.
Dr. Joana Carmo
Gastroenterology Department, Hospital Egas Moniz – CHLO
Rua da Junqueira, 126
PT–1349-019 Lisbon (Portugal)
E-Mail joanavcarmo@gmail.com
Received: April 27, 2017; Accepted after revision: July 17, 2017














