Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.1 Lisboa fev. 2018
https://doi.org/10.1159/000477550
CLINCIAL CASE STUDY
Intestinal Obstruction of Uncommon Cause and Point-of-Care Ultrasonography – Where Do We Stand?
Obstrução Intestinal de Causa Rara e Ecografia Point-of-Care – Em que Ponto Nos Encontramos?
Tiago Capelaa, Paula Sousab, Ana Caldeirac, Eduardo Pereirac
aGastroenterology Department, Hospital Santo António dos Capuchos, Centro Hospitalar Lisboa Central, Lisbon, bGastroenterology Department, Centro Hospitalar Tondela-Viseu, Viseu and cGastroenterology Department, Hospital Amato Lusitano, Castelo Branco, Portugal
* Corresponding author.
ABSTRACT
Malignant neoplasms of the small bowel, especially from the jejunum, are among the rarest types of cancer. Given its location, a delayed diagnosis is frequent and sometimes only made in an emergency context. The authors present a case of intestinal obstruction, where ultrasonography was pivotal in establishing a diagnosis. Point-of-care ultrasonography seems to be particularly sensitive in assessing emergency patients with abdominal pain, allowing effective orientation and saving human and technical resources.
Keywords: Jejunal adenocarcinoma, Point-of-care ultrasonography,·Intestinal obstruction, Small bowel tumor
RESUMO
As neoplasias malignas do intestino delgado, particularmente as do jejuno, estão entre os tipos de tumores mais raros. Devido à sua localização, é frequente existir um atraso no diagnóstico e muitas vezes apenas em contexto de emergência a situação é solucionada. Os autores apresentam um caso de obstrução intestinal, onde a ecografia realizada por gastrenterologista foi fundamental no estabelecimento diagnóstico. A ecografia point-of-care parece ser muito sensível no diagnóstico em urgência, nomeadamente em doentes com dor abdominal, permitindo orientação adequada e poupando recursos humanos e técnicos.
Palavras-Chave: Adenocarcinoma do jejuno, Ecografia point-of-care,·Obstrução intestinal, Tumor de intestino delgado
Introduction
Malignant neoplasms of the small bowel are among the rarest types of cancer, accounting for only 2% of all gastrointestinal neoplasms. In Western countries, adenocarcinomas generally represent the largest histological type; in the small bowel, the duodenum is its most frequent location [1]. For neoplasms from the jejunum and ileum, diagnostic delays range from months to years. Many patients are misdiagnosed as being neurotic or as having irritable bowel syndrome [2]. It is sometimes only due to emergency situations that a correct diagnosis is finally established. Concepts like bedside ultrasonography (US) and point-of-care US are becoming routine in our clinical practice, expanding the possible applications of US, thus sharing the importance of ultrasound knowledge between senior physicians and residents of several specialties [3].
Case Report
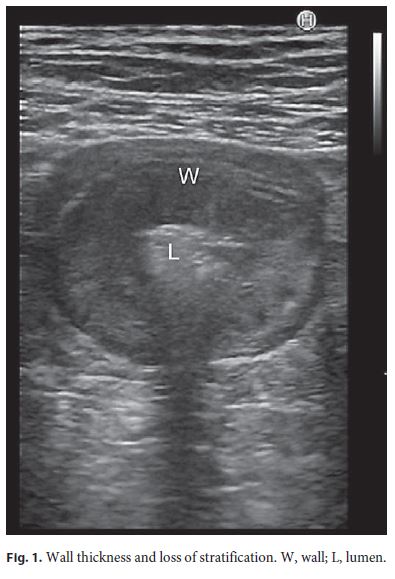
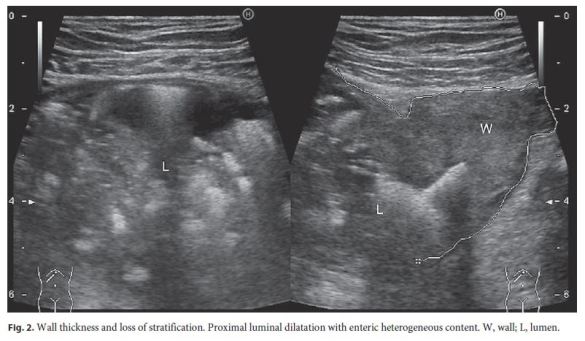
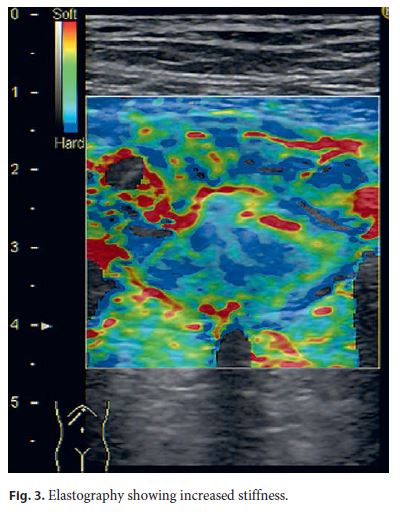
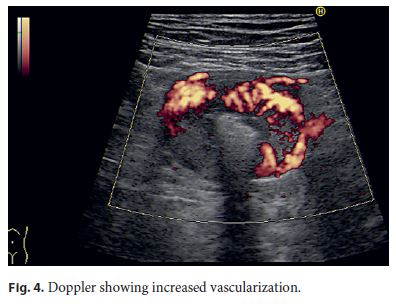
We report the case of a 79-year-old male, without a relevant medical history, who presented with a 5-month history of weight loss, vomiting, and periumbilical cramping. The initial evaluation showed microcytic anemia and hypoalbuminemia. Later, upper gastrointestinal endoscopy, colonoscopy, and abdominal and pelvic CT scans were performed but demonstrated no relevant findings. Because of clinical worsening with daily vomiting and abdominal tenderness, the patient returned to the emergency room. An US evaluation with a linear probe was performed by a gastroenterologist who observed a 3-cm-long, jejunal, obstructive lesion, with irregular intestinal wall thickness and loss of stratification (Fig. 1, 2), increased stiffness on elastography (Fig. 3), and increased vascularization on Doppler (Fig. 4). A proximal dilatation of the duodenum and the jejunum (Fig. 2) was also noted, indicating an obstruction of the small bowel. No local adenopathies were seen.
After clinical discussion, segmental enterectomy was performed. Histology showed a jejunal adenocarcinoma (based on the surgical sample and anterior radiologic findings, the tumors stage was T3N0M0). Six months later, the patient remains well and without complaints. A retrospective evaluation of the CT scan performed 3 months before surgery showed a slight thickening of the enteric wall that could have corresponded to the tumor later found in the emergency room.
Discussion
Malignant neoplasms of the small bowel are rare entities. The duodenum seems to be the most frequently affected segment with 55–82% of all cases [4]. The estimated incidence in the United States is around 7 per 1 million individuals [5]. In Europe, an incidence rate of 3,600 new cases per year has been reported [6]. The strongest known risk factor for small bowel adenocarcinoma is prior Crohns disease [7]. Other suggested factors include cigarette smoking, alcohol consumption, prior peptic ulcer disease, familial adenomatous polyposis, prior colon cancer, celiac sprue, and cystic fibrosis [1]. With none of the risk factors (as in the present case), a jejunal adenocarcinoma is an even rarer diagnosis. Recently, Young et al. [8] have revealed that surgery seems to be the only treatment that improves survival on small bowel adenocarcinoma, and no benefit was seen by adding chemotherapy regimens. Even so, the 5-year survival rate after diagnosis is around 30% [5]. The clinical, ultrasound-assisted approach has proved to be particularly sensitive in assessing emergency patients with nodules of the neck, dyspnea, abdominal pain, and limb edema [9].
We present this case because of the rarity of the previously described entity, but also to exhibit that point-ofcare US allows a quick and effective patient orientation, with innumerous clinical applications, saving human and technical resources, and showing once more that US competences should be transversely acquired perhaps by all physicians.
References
1 Neugut I, Jacobson S, Suh S, et al: Epidemiology of cancer of the small intestine. Cancer Epidemiol Biomarkers Prev 1998;7:243–251. [ Links ]
2 Bauer L, Palmer L, Bauer M, et al: Adenocarcinoma of the small intestine: 21-year review of diagnosis, treatment, and prognosis. Ann Surg Oncol 1994;1:183–188. [ Links ]
3 Sabath BF, Singh G: Point-of-care ultrasonography as a training milestone for internal medicine residents: the time is now. J Community Hosp Intern Med Perspect 2016;6:33094. [ Links ]
4 Aparicio T, Zaanan A, Svrcek M, et al: Small bowel adenocarcinoma: epidemiology, risk factors, diagnosis and treatment. Dig Liver Dis 2014;46:97–104. [ Links ]
5 Bilimoria KY, Bentrem DJ, Wayne JD, et al: Small bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg 2009;249:63–71. [ Links ]
6 Faivre J, Trama A, De Angelis R, et al: Incidence, prevalence and survival of patients with rare epithelial digestive cancers diagnosed in Europe in 1995–2002. Eur J Cancer 2012;48:1417–1424. [ Links ]
7 Cahill C, Gordon C, Petrucci A, et al: Small bowel adenocarcinoma and Crohns disease: any further ahead than 50 years ago? World J Gastroenterol 2014;20:11486–11495. [ Links ]
8 Young J, Mongoue-Tchokote S, Wieghard N, et al: Treatment and survivl of small-bowel adenocarcinoma in the United States: a comparison with colon cancer. Dis Colon Rectum 2016;59:306–315. [ Links ]
9 Arienti V, Di Giulio R, Cogliati C, et al: Bedside ultrasonography (US), Echoscopy and US point of care as a new kind of stethoscope for Internal Medicine Departments: the training program of the Italian Internal Medicine Society (SIMI). Intern Emerg Med 2014;9:805–814. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
All authors declare no conflicts of interest.
* Corresponding author.
Dr. Tiago Capela
Gastroenterology Department, Hospital Santo António dos Capuchos
Centro Hospitalar Lisboa Central, Alameda de Santo António dos Capuchos
PT–1169-050 Lisbon (Portugal)
E-Mail teixeira.capela@gmail.com
Received: December 16, 2016; Accepted after revision: February 21, 2017














