Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.6 Lisboa dez. 2017
https://doi.org/10.1159/000478942
ENDOSCOPIC SNAPSHOT
An Unusual Diagnosis in a Patient with Suspected Colorectal Cancer
Um diagnóstico raro em doente com suspeita de neoplasia colo-rectal
Joana Carmoa, Susana Marquesa, Miguel Bispoa,b, Pedro Figueiredoa,b, David Serrab
aDepartment of Gastroenterology, Hospital de Egas Moniz, Centro Hospitalar de Lisboa Ocidental, and
bDepartment of Gastroenterology, Hospital da Luz, Lisbon, Portugal
* Corresponding author.
Keywords: Colonoscopy, Colorectal cancer, Colonic lipoma
Palavras-Chave: Colonoscopia, Cancro colo-rectal, Lipoma do cólon
A 78-year-old female was referred to a gastroenterology appointment due to recurrent lower abdominal pain, anorexia, and significant ( ∼ 10%) weight loss over the last 3 months. Abdominal computed tomography (CT) showed a 4-cm hypodense lobulated lesion, with an eccentric solid component, in the ascending colon (Fig. 1). In colonoscopy, a large broad-based ulcerated mass, with necrotic and fatty tissue exposed in the ulcerated area, was documented in the ascending colon (Fig. 2a, b). First, this lesion was misinterpreted as an ulcerated and necrotic colonic adenocarcinoma, but biopsies were negative for malignancy. Colonoscopy was repeated and the hypothesis of a large ulcerated colonic lipoma was considered. As this large and extensively ulcerated lesion was symptomatic, laparoscopic right hemicolectomy was performed. Pathological gross examination showed an ulcerated mass with a broad base, measuring 40 × 30 mm. The ulcerated surface was covered with fatty and gray necrotic material. Cut sections showed that the lesion was within the submucosa. Histopathologic examination revealed that the mass was composed of mature adipose tissue covered by ulcerated and chronic inflamed mucosa (Fig. 3a, b). Resected lymph nodes had only reactive changes. Postoperative outcome was uneventful and the patient has been asymptomatic since then.
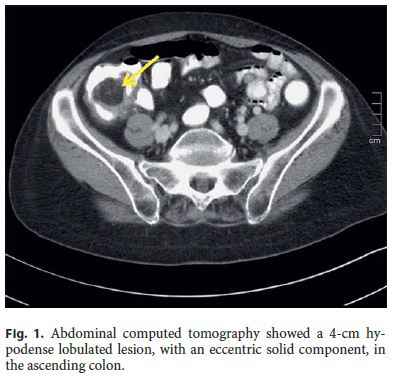


Colonic lipomas are the most common nonepithelial tumors of the colon (mesenchymal origin) and rank third in frequency among benign colonic tumors, after hyperplastic and adenomatous polyps [1]. Most of these tumors are asymptomatic and usually detected incidentally during imaging studies or colonoscopy [2]. Large lipomas can become symptomatic and may mimic clinical features and endoscopic appearance of colonic carcinoma [1–4]. When lipomas are >2 cm, they may present with abdominal pain, bleeding and/or bowel obstruction, either intermittent or complete, secondary to intussusceptions or to direct luminal obstruction by the enlarging mass [1, 2]. CT may demonstrate a well-circumscribed intraluminal mass with low attenuation consistent with soft (fatty) tissue, and it is particularly useful for identifying large colonic lipomas [2]. However, the diagnostic value of CT is limited, particularly in small lipomas [4]. Surrounding soft tissue or stool may create an artificial increase in CT density values, which can also limit its accuracy [3]. Magnetic resonance imaging may be particularly useful in the detection of these lesions, as the signal intensity is characteristic of adipose tissue on T1-weighted and fat-suppressing images [1]. Colonoscopy is generally reliable for the diagnosis of colonic lipoma. A number of endoscopic features suggestive of colonic lipomas have been described, including the cushion/pillow sign (indentation on gentle pressure with the tip of a biopsy forceps), the tenting sign (elevation of the overlying mucosa when grasped by the forceps), and the naked fat sign (extrusion of fat at a biopsy site) [3]. The mucosa overlying colonic lipomas is usually normal, but, in rare cases, colonoscopy may reveal ulceration, a finding that may lead to a wrong diagnosis of adenocarcinoma [1, 2]. Asymptomatic lipomas of the large bowel probably do not need treatment, because malignant transformation has not been reported [3]. Therapy should be reserved for symptomatic lesions or for cases where exclusion of adenocarcinoma cannot be assured [3].
References
1 Katsinelos P, Chatzimavroudis G, Zavos C, Pilpilidis I, Lazaraki G, Papaziogas B, Paroutoglou G, et al: Cecal lipoma with pseudomalignant features: a case report and review of the literature. World J Gastroenterol 2007;13:2510–2513. [ Links ]
2 Meghoo C, Cook P, McDonough C, Bowser L, Waddell B: Large colonic lipoma with mucosal ulceration mimicking carcinoma. Gastrointest Endosc 2003;58:468–470. [ Links ]
3 El-Khalil T, Mourad F, Uthman S: Sigmoid lipoma mimicking carcinoma: case report with review of diagnosis and management. Gastrointest Endosc 2000;51:495–496. [ Links ]
4 Aytaç B, Yerci O, Gurel S, Ferik Z: Colonic lipomas mimicking colon cancer. Turk J Pathol 2010;26:196–199. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
All authors have approved the manuscript and agree with its submission to GE – Portuguese Journal of Gastroenterology . All authors have nothing to disclose and there is no funding to declare.
* Corresponding author.
Dr. Joana Carmo
Gastroenterology Department, Hospital Egas Moniz
Centro Hospitalar de Lisboa Ocidental, Rua da Junqueira, 126
PT–1349-019 Lisbon (Portugal)
E-Mail joanavcarmo@gmail.com
Received: March 14, 2017; Accepted after revision: May 18, 2017














