Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.6 Lisboa dez. 2017
https://doi.org/10.1159/000478939
CLINICAL CASE STUDY
Endoscopic Mucosectomy in a Child Presenting with Gastric Heterotopia of the Rectum
Mucosectomia endoscópica em criança com heterotopia gástrica do reto
Joana Soaresa, Carla Ferreirab, Margarida Marquesc, Susana Corujeirad, Marta Tavaresd, Joanne Lopese, Fátima Carneiroe, Jorge Amil Diasd, Eunice Trindaded
aServiço de Pediatria, Centro Hospitalar de Trás-os-Montes e Alto Douro, EPE, Vila Real, bServiço de Pediatria, Hospital Senhora da Oliveira, Guimarães, EPE, Guimarães, and cServiço de Gastroenterologia, dServiço de Pediatria, and eServiço de Anatomia Patológica, Centro Hospitalar de São João, EPE, Porto, Portugal
* Corresponding author.
ABSTRACT
Gastric mucosal heterotopia has been described in all levels of the gastrointestinal tract. Its occurrence in the rectum is uncommon. We report the case of a 4-year-old boy referred to Pediatric Gastroenterology for intermittent rectal bleeding for the past 2 years. Total ileocolonoscopy revealed a flat, well-circumscribed lesion of 4 cm, with elevated margins, localized at 10 cm from the anal verge. Histologic examination showed typical gastric mucosa of the oxyntic type. Treatment with proton pump inhibitors was started without resolution of the symptoms and, therefore, an endoscopic mucosal resection was performed. Heterotopic gastric mucosa represents a rare cause of rectal bleeding in children and endoscopic evaluation is fundamental for diagnosis. Although not usually performed in pediatric ages, endoscopic mucosectomy allows complete resolution of the problem avoiding surgery.
Keywords: Heterotopic gastric mucosa, Endosocopic mucosal resection, Rectum
RESUMO
A heterotopia da mucosa gástrica pode ocorrer em qualquer local do trato gastrointestinal, mas a localização retal é invulgar. Apresenta-se o caso clínico de uma criança de 4 anos, referenciada à consulta de Gastroenterologia Pediátrica por retorragia intermitente com cerca de 2 anos de evolução. Foi realizada ileocolonoscopia total com visualização de lesão plana de bordos elevados e bem delimitada, com cerca de 4 cm, localizada 10 cm acima da margem anal. O exame histológico revelou a presença de mucosa gástrica do tipo oxíntico. Iniciou terapêutica oral com inibidor da bomba de protões, sem resposta, pelo que se procedeu a mucosectomia endoscópica. A heterotopia da mucosa gástrica é uma causa rara de retorragias em idade pediátrica sendo a avaliação endoscópica fundamental para o diagnóstico. A utilização de técnica endoscópica de ablação da mucosa, pouco usual em idade pediátrica, permite a resolução definitiva do problema evitando a cirurgia.
Palavras-Chave: Heterotopia mucosa gástrica, Resseção endoscópica mucosa, Reto
Introduction
Gastric heterotopia has been described at all sites of the gastrointestinal (GI) tract, but its localization in the rectum is uncommon, with few cases described in pediatric ages. The most common symptom at presentation is painless rectal bleeding, with abdominal pain and diarrhea also being reported.
Case Report
A healthy 4-year-old boy with no past medical history was referred to Pediatric Gastroenterology for rectal intermittent bleeding, at least twice a month, for the past 2 years. The bleeding was described as bright red blood, in variable amount, on the toilet paper and streaked on the stools. There were no other symptoms, namely, abdominal pain, changes in intestinal habits, weight loss, or other systemic symptoms. Physical examination was unremarkable and anal inspection was normal.
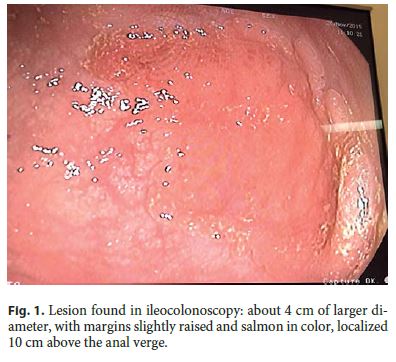
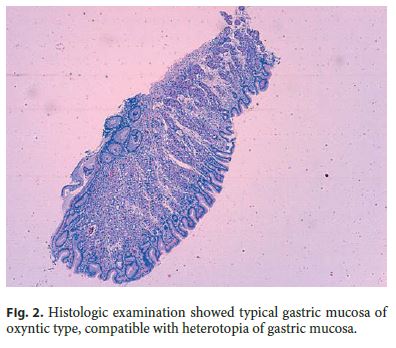
Ileocolonoscopy examination revealed a well-circumscribed lesion of about 4 cm of larger diameter, slightly raised and salmon in color, without ulcers or erosions, localized 10 cm above the anal verge (Fig. 1). Apart from this lesion, the examination of the colonic mucosa was normal. Histologic examination of the lesion showed typical gastric mucosa of oxyntic type, without inflammatory changes, compatible with heterotopia of gastric mucosa localized in the rectum (Fig. 2).
Treatment with proton pump inhibitors was started without resolution of the symptoms and therefore, an endoscopic mucosal resection (EMR) was performed. The technique used was the injection-assisted EMR. The procedure started with injection of a saline solution into the submucosal space under the lesion creating a safety cushion. The cushion lifted the lesion, facilitating capture and removal by using a 15-mm snare, while minimizing mechanical and electrocautery damage to the deeper layers of the GI wall. The lesion was completely removed in a piecemeal fashion (Fig. 3).

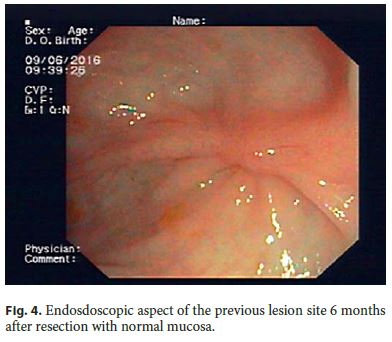
Sigmoidoscopy performed 6 months later confirmed the efficacy of the procedure with normal biopsies of the tissue around the scar (Fig. 4). The patient remains asymptomatic 1 year later.
Discussion
Heterotopic gastric mucosa has been described throughout the GI tract being more often present in the esophagus. In recent published series, endoscopic prevalence of heterotopic gastric mucosa in the proximal digestive tract ranges from 0.4 to 9% [1–4]. Rectal localization is rare, particularly in pediatric ages, with less than 30 cases published in the literature [5]. Males seem to be predominantly affected and patient age is extremely variable, with an average age at presentation of about 21 years [6].
The pathogenesis of this condition is unclear: ectopic mucosa can result from an embryologic defect in differentiation of rectal endoderm resulting in fundic or mixed gastric mucosa or as metaplasia following trauma which results in pyloric mucosa [7 . Ectopic gastric mucosa can secrete acid and induce the appearance of gastritis and ulcer. Active acid secretion has been proved in in vitro studies and indirectly demonstrated in cases in whom treatment with proton pump inhibitors induced healing of associated ulcers [8–10]. In children, clinical symptoms are usually present at diagnosis, the most common being painless rectal bleeding, and the presence of anorectal symptoms has been associated with a higher prevalence of gastric oxyntic mucosa. More serious complications like life-threatening bleeding, bowel perforation, megacolon, perianal fistula, and rectovesical fistula have also been reported [11–15].
Definitive diagnosis requires a biopsy and histologic analysis of the abnormal mucosa. Typically, fundic-type mucosa is identified, although lesions containing other variants of gastric mucosa have been described [7, 16]. The heterotopic tissue is frequently located in the posterolateral region of the rectum, about 5–8 cm from the anal verge.
Medical treatment with H 2 receptor blockers or proton pump inhibitors can ameliorate or completely resolve the symptoms by inhibiting the production of acid; however, they do not cause the involution of the lesion and symptoms may reappear when treatment is discontinued [15–17]. In this case, there was no symptomatic relief with pharmacologic therapeutics and an EMR was performed. EMR was developed for minimally invasive, organ-sparing endoscopic removal of benign and early malignant lesions in the GI tract and it seemed the best option for our patient. The successful use of this technique has been reported in 3 other pediatric patients without complications [18–20]. Successful en bloc endoscopic submucosal dissection has been recently reported in an adult patient; this approach was also considered in our patient but due to the increased risk of perforation and the benign nature of the lesion, it was abandoned [5]. Due to its exceptional application in pediatric ages, the procedure was performed by an adults gastroenterologist.
Conclusion
EMR is a safe and effective option in the treatment of gastric heterotopia of the rectum as long as it is carried out by experienced gastroenterologists. The use of EMR allowed complete resolution of the situation with documented safety and efficacy.
References
1 Rodriguez Martinez A, Salazar Quero JC, Tutau Gomez C, et al: Heterotopic gastric mucosa of the proximal oesophagus (inlet patch): endoscopic prevalence, histological and clinical characteristics in paediatric patients. Eur J Gastroenterol Hepatol 2014;26:1139–1145. [ Links ]
2 Fang Y, Chen L, Chen DF, et al: Prevalence, histologic and clinical characteristics of heterotopic gastric mucosa in Chinese patients. World J Gastroenterol 2014;20:17588–17594. [ Links ]
3 Terada T: Heterotopic gastric mucosa of the gastrointestinal tract: a histopathologic study of 158 cases. Pathol Res Pract 2011;207:148–150. [ Links ]
4 Maconi G, Pace F, Vago L, Carsana L, Bargiggia S, Bianchi Porro G: Prevalence and clinical features of heterotopic gastric mucosa in the upper oesophagus (inlet patch). Eur J Gastroenterol Hepatol 2000;12:745–749. [ Links ]
5 Iacopini F, Gotoda T, Elisei W, et al: Heterotopic gastric mucosa in the anus and rectum: first case report of endoscopic submucosal dissection and systematic review. Gastroenterol Rep (Oxf) 2016;4:196–205. [ Links ]
6 Devereaux CE, Devereaux RG: Heterotopic gastric mucosa of the rectum with a review of the literature. J Clin Gastroenterol 1994;19:41–45. [ Links ]
7 Wolff M: Heterotopic gastric epithelium in the rectum: a report of three new cases with a review of 87 cases of gastric heterotopia in the alimentary canal. Am J Clin Pathol 1971;55:604–616. [ Links ]
8 Pistoia MA, Guadagni S, Tuscano D, et al: Ulcerated ectopic gastric mucosa of the rectum. Gastrointest Endosc 1987;33:41–43. [ Links ]
9 Goldfarb WB, Schaefer R: Gastric heterotopias in the rectum: report of a case. Ann Surg 1961;154:133–136. [ Links ]
10 Debas HT, Chaun H, Thomson FB, et al: Functioning heterotopic oxyntic mucosa in the rectum. Gastroenterology 1980;79:1300–1302. [ Links ]
11 Dubilier LD, Caffrey PR, Hyde GL: Multifocal gastric heterotopia in a malformation of the colon presenting as a megacolon. Am J Clin Pathol 1969;51:646–653. [ Links ]
12 Parkash S, Veliath AJ, Chandrasekaran V: Ectopic gastric mucosa in duplication of the rectum presenting as a perianal fistula. Dis Colon Rectum 1982;25:225–226. [ Links ]
13 Kalani BP, Vaezzadeh K, Sieber WK: Gastric heterotopia in rectum complicated by rectovesical fistula. Dig Dis Sci 1983;28:378–380. [ Links ]
14 Schwarzenberg SJ, Whitington PF: Rectal gastric mucosa heterotopia as a cause of hematochezia in an infant. Dig Dis Sci 1983;28: 470–472. [ Links ]
15 Testart J, Maupas JL, Metayer J, et al: Rectal peptic ulceration – a rare cause of rectal bleeding. Report of a case. Dis Colon Rectum 1988;31:803–805. [ Links ]
16 Steele SR, Mull enix PS, Martin MJ, OrmsethE, Weppler E, Graham J, et al: Heterotopic gastric mucosa of the anus: a case report and review of the literature. Am Surg 2004;70:715–719. [ Links ]
17 Murray FE, Lombard M, Dervan P, et al: Bleeding from multifocal heterotopic gastric mucosa in the colon controlled by an H2 antagonist. Gut 1988;29:848–851. [ Links ]
18 Di Nardo G, Frediani S, Lucarelli S, et al: An unusual cause of rectal bleeding in a child. Gastrointest Endosc 2010;72:851–852. [ Links ]
19 De Angelis P, Trecca A, Francalanci P, et al: Heterotopic gastric mucosa of the rectum. Endoscopy 2004;36:927. [ Links ]
20 Sauer CG, Bickston SJ, Borowitz SM: Gastric heterotopia of the rectum. J Pediatr Gastroenterol Nutr 2010;50:329–333. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors declare no conflicts of interest. No funding was obtained concerning this study.
* Corresponding author.
Dr. Joana Soares
Centro Hospitalar de Trás-os-Montes e Alto Douro, EPE
Avenida da Noruega
PT–5000-508 Vila Real (Portugal)
E-Mail joanamsoares1@hotmail.com
Received: October 27, 2016; Accepted after revision: January 10, 2017














