Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.6 Lisboa dez. 2017
https://doi.org/10.1159/000479232
ORIGINAL ARTICLE
Cytomegalovirus Disease of the Upper Gastrointestinal Tract: A 10-Year Retrospective Study
Estudo Retrospectivo a 10 Anos sobre os Aspectos Clínicos e Achados Endoscópicos da Infecção a Citomegalovirus do Tubo Digestivo Alto
Susana Marquesa, Joana Carmoa, Daniel Pintob, Miguel Bispoa, Sância Ramosb, Cristina Chagasa
Departments of aGastroenterology and bPathology, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Background and Aims: Cytomegalovirus (CMV) disease of the gastrointestinal (GI) tract is a major cause of morbidity and mortality in immunocompromised patients. The colon is the most commonly affected site, and the literature is scarce regarding CMV disease of the upper GI tract. Therefore, our study aimed to evaluate the clinical and endoscopic features of upper GI CMV disease. Methods: This 10-year retrospective study included all patients with a histopathological diagnosis of upper GI CMV infection. Patients clinical, endoscopic, therapy, and follow-up data were collected from medical records. Results: Twelve patients with histopathologically proven upper GI CMV disease were identified (age 61 ± 18 years, 50% men). Most of the patients were immunocompromised (75%) due to acquired immunodeficiency syndrome (AIDS), malignancy, and/or immunosuppressive therapy. In the remainder (25%), the disease occurred in the absence of immunodeficiency and immunosuppression. Three patients (all with AIDS) presented with disseminated CMV infection. In the majority of the cases (83%), upper GI CMV disease was symptomatic, and the most common clinical presentations were odynophagia/dysphagia (25%) and nausea/vomiting (25%). Endoscopically, there were 5 cases of esophagitis (42%) and 7 cases of gastritis (58%). The lower esophagus (33%) and the gastric antrum (42%) were the most frequently affected GI sites. Regardless of the location, mucosal ulceration was the most common endoscopic finding (75%) and was associated with very deep ulceration resembling cavitation in 2 cases. Other endoscopic features were mucosal edema, hyperemia, and nodularity (25%). Eleven patients (92%) received antiviral treatment (duration 26 ± 12 days). The 1-month and 1-year mortality rates were 16.7 and 25%, respectively. Conclusions: Upper GI CMV disease can occur in the absence of immunodeficiency and immunosuppression. It is usually symptomatic, and mucosal ulceration is often evident at endoscopy. It is associated with significant mortality; therefore, early diagnosis and adequate antiviral treatment are essential.
Keywords: Cytomegalovirus, Esophagitis, Gastritis, Endoscopy
RESUMO
Introdução: A doença gastrointestinal (GI) por Citomegalovírus (CMV) é uma causa importante de morbilidade e mortalidade em doentes imunocomprometidos. O cólon é o local mais comummente afectado e a literatura é escassa em relação à doença por CMV do tracto GI alto. Dessa forma, o nosso estudo teve como objectivo avaliar as características clínicas e endoscópicas da doença por CMV do tracto GI alto. Métodos: Trata-se de um estudo retrospectivo de 10 anos, que incluiu todos os doentes com o diagnóstico histopatológico de doença por CMV do tracto GI alto. Os dados clínicos, endoscópicos e sobre a terapêutica e o follow-up dos doentes foram obtidos por consulta de processos clínicos. Resultados: Foram identificados 12 doentes com o diagnóstico histopatológico de doença por CMV do tracto GI alto (idade 61 ± 18 anos, 50% homens). A maioria dos doentes era imunocomprometida (75%) no contexto de síndrome de imunodeficiência adquirida (SIDA), malignidade e/ou terapêutica imunossupressora. Nos restantes doentes (25%), a doença ocorreu na ausência de imunodeficiência ou imunossupressão. Três doentes (todos com SIDA) apresentaram infecção por CMV disseminada. Na maioria dos casos (83%), a doença por CMV do tracto GI alto foi sintomática e as apresentações clínicas mais comuns foram odinofagia/disfagia (25%) e náuseas/vómitos (25%). Endoscopicamente, registaram-se 5 casos de esofagite (42%) e 7 casos de gastrite (58%). O esófago inferior (33%) e o antro gástrico (42%) foram os locais mais frequentemente envolvidos. Independentemente da localização, a ulceração da mucosa foi o achado endoscópico mais comum (75%) e associou-se a ulceração muito profunda semelhante a cavitação em 2 casos. Outros achados endoscópicos foram edema, hiperémia e nodularidade da mucosa (25%). Onze doentes (92%) receberam terapêutica antiviral (duração 26 ± 12 dias). As taxas de mortalidade a 1 mês e a 1 ano foram 16.7 e 25%, respectivamente. Conclusões: A doença por CMV do tracto GI alto pode ocorrer na ausência de imunodeficiência e de imunossupressão. É geralmente sintomática e apresenta com frequência ulceração da mucosa na endoscopia. Associa-se a mortalidade significativa, pelo que o diagnóstico precoce e a instuição adequada de tratamento antiviral são essenciais.
Palavras-Chave: Citomegalovírus, Esofagite, Gastrite, Endoscopia
Introduction
Cytomegalovirus (CMV) disease of the gastrointestinal (GI) tract is a major cause of morbidity and mortality in immunocompromised patients [1–3]. Patients at increased risk for GI CMV infection are those with acquired immunodeficiency syndrome (AIDS), recipients of solid and bone marrow transplants, those receiving immunosuppressive therapy, and patients with malignancies, especially those under chemotherapy or with haematological malignancies [1–3]. The colon is the most commonly affected site in GI CMV disease. However, the literature is limited regarding CMV disease of the upper GI tract.
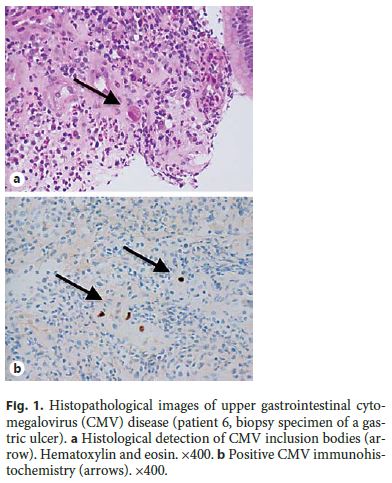
The clinical presentation of GI CMV disease is variable and depends on the location and severity of the disease. Symptomatic patients may complain of dysphagia/odynophagia, nausea/vomiting, abdominal pain, and weight loss [1, 4]. Diagnosis of GI CMV disease relies mostly on endoscopy and GI biopsy. Histopathological diagnosis is made with the identification of CMV inclusion bodies on histology or with a positive immunohistochemical staining using anti-CMV monoclonal antibodies (Fig. 1) [1, 3]. A 2- to 3-week course of antiviral treatment with intravenous (i.v.) ganciclovir or per os (p.o.) valganciclovir is successful in most cases [5–7]. Nonetheless, GI CMV can cause serious disease in immunocompromised patients and has been associated with significant morbidity and mortality [8, 9]. Our study aimed to evaluate the clinical and endoscopic features of upper GI CMV disease, which have still not been well defined in the literature.
Material and Methods
Upper GI CMV disease was defined as the histological detection of CMV inclusion bodies in routine hematoxylin and eosin staining or a positive immunohistochemistry staining using anti-CMV monoclonal antibodies, and presenting signs or symptoms consistent with upper GI disease [3]. Disseminated CMV disease was defined as involvement of one or more organs besides the upper GI tract.
We retrospectively identified and reviewed the medical records of patients with histopathologically proven upper GI CMV disease who were hospitalized in our medical center between January 2006 and December 2015 (10-year period).
Patients demographic, clinical, endoscopic, therapy, and follow- up data were collected from medical records. The following parameters were recorded: age, sex, underlying systemic diseases, disseminated CMV disease, symptoms and signs at the time of diagnosis, involved site of the upper GI tract at endoscopy, endoscopic findings, antiviral treatment, and 1-month and 1-year mortality.
Statistical analysis was performed using IBM SPSS Statistics, 22.0 (IBM Corp., USA).
Results
A total of 12 patients with histopathologically proven upper GI CMV disease were identified. The mean patient age at diagnosis was 61 ± 18 years (range 39–94 years) and there was no gender predilection (male:female ratio 1.0) (Table 1).
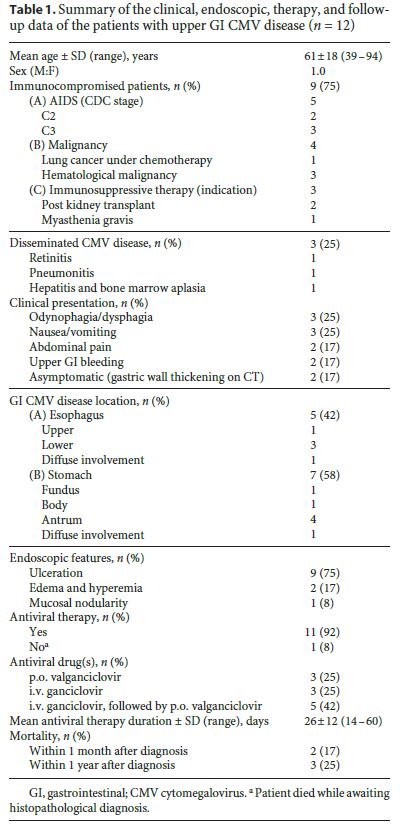
Most of the patients were immunocompromised (9/12, 75%) (Table 2). Five patients had AIDS and all were stage C2 or C3 by the CDC definition. Two AIDS patients also had a malignancy (1 had a diffuse large B-cell lymphoma and the other had a lung tumor and was receiving chemotherapy). In the immunocompromised non-AIDS group, 2 patients were kidney transplant recipients under immunosuppressive treatment (one of which had a concomitant anaplastic lymphoma), 1 patient had myasthenia gravis and was receiving immunosuppression, and 1 patient had a diffuse large B-cell lymphoma. In 3 patients, the disease occurred in the absence of immunodeficiency and immunosuppression (25%). In the non-immunocompromised group, there was an 87-year-old patient without known comorbidities, an 86-year-old post-stroke patient, and a 51-year-old patient with decompensated alcoholic liver cirrhosis.
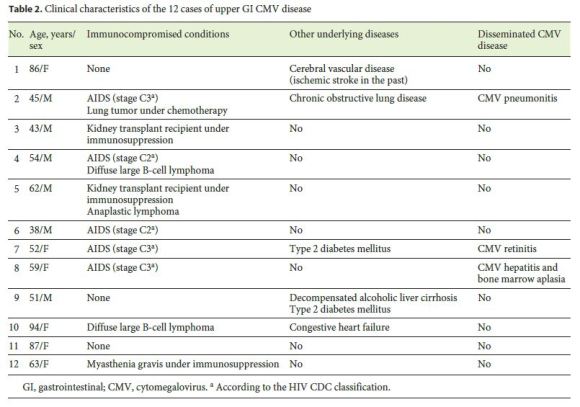
Three patients, all AIDS stage C3 by CDC definition, presented with disseminated CMV infection. Besides upper GI tract involvement, 1 had retinitis, 1 had pneumonitis, and 1 had hepatitis and bone marrow aplasia. Most of the patients had symptomatic upper GI CMV disease (83%) (Table 3). The most common clinical presentations were odynophagia/dysphagia (25%) and nausea/vomiting (25%). Other reported symptoms were abdominal pain (17%) and upper GI bleeding manifested by melena (17%). Two patients were asymptomatic (17%) and both were referred for upper GI endoscopy because of gastric wall thickening found incidentally on CT.
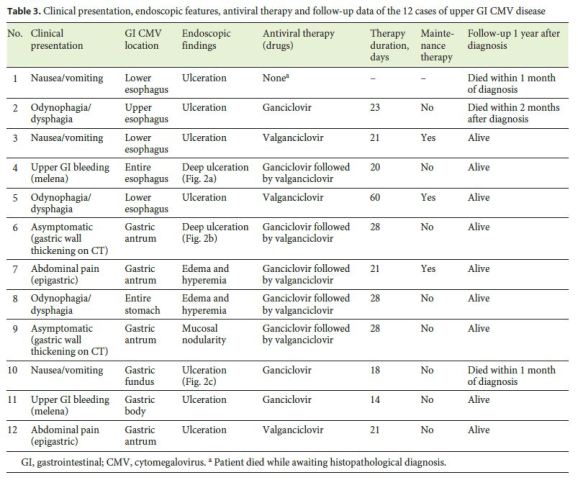
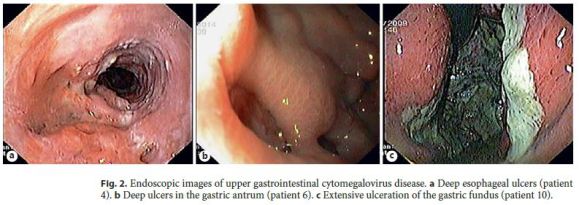
Endoscopically, there were 5 cases of CMV esophagitis (42%) and 7 cases of CMV gastritis (58%). The lower esophagus (33%) and the gastric antrum (42%) were the most frequently affected GI sites. Regardless of the location of the upper GI CMV disease, mucosal ulceration was the most frequent endoscopic finding (75%). Ulcers were very deep, resembling the formation of cavities in 2 cases (Fig. 2). Other endoscopic features were mucosal edema and hyperemia (17%) as well as mucosal nodularity (8%).
Except for 1 patient who died while awaiting histopathological diagnosis, all others received antiviral treatment (11/12, 92%). Three patients were treated with p.o. valganciclovir alone, 3 with i.v. ganciclovir alone, and 5 received sequential therapy with i.v. ganciclovir followed by p.o. valganciclovir. The mean duration of the antiviral treatment was 26 ± 12 days (range 14–60 days). Maintenance therapy with a lower dose of p.o. valganciclovir was subsequently given in 3 patients (1 AIDS patient with CMV retinitis and 2 kidney transplant recipients under high-dose immunosuppression).
Regarding the clinical outcome, 2 patients died within the first month after diagnosis (1-month mortality rate of 17%) and 1 patient died within the first year (1-year mortality rate of 25%).
Discussion
CMV disease of the GI tract is a common manifestation of CMV infection and the colon is the most frequently involved GI segment [1]. However, the literature is scarce regarding CMV disease of the upper GI tract. Two of the largest studies concerning upper GI CMV disease are from Wang et al. [1] and from Péter et al. [10]. The first study identified 16 patients with CMV esophagitis and the second included 91 patients with CMV gastritis and/or duodenitis. Among these and other studies, it has been consistently observed that GI CMV infection is much more common in immunocompromised patients. The immunocompromised conditions most frequently reported are AIDS, solid and bone marrow transplantation, other conditions requiring immunosuppressive therapy, and malignancies, especially if under chemotherapy or hematological malignancies [1–3]. Despite immunocompromised patients being more often affected, Bonetti et al. [4] reported in a case series of 30 patients with upper GI CMV disease that 50% of them were apparently healthy individuals. In a similar way, in the present study, although the majority of patients were immunocompromised, in 25% the disease occurred in the absence of immunodeficiency and immunosuppression.
The clinical presentation of upper GI CMV disease is variable and depends on its location and severity. Wang et al. [1] reported odynophagia/dysphagia (44%) and epigastric pain (31%) as the most common symptoms in CMV esophagitis patients. In contrast, Péter et al. [10] concluded that abdominal pain (39%), anemia/GI bleeding (20%), and nausea/vomiting (13%) were the most frequently complaints in patients with CMV gastritis/duodenitis. Moreover, in up to 7% of the cases, upper GI CMV disease may have an asymptomatic presentation [10]. Our study was consistent with these results as dysphagia (40%) and abdominal pain (29%) were also the most common symptoms in CMV esophagitis and gastritis patients, respectively. Additionally, 17% of the patients were asymptomatic and were referred for upper endoscopy because of gastric wall thickening found incidentally on an abdominal CT scan.
The endoscopic appearance of upper GI CMV disease is also variable and nonspecific. It can range from normal or minimal inflamed mucosa to deep ulceration [2, 4]. The most documented endoscopic findings depend on the location of the disease. In CMV esophagitis, ulcers are more common than mucosal inflammation (88 vs. 63%) [1], whereas in gastroduodenal disease inflammatory changes may exceed ulceration (54 vs. 18%) [10]. Despite the location in the GI tract, erosions and ulcers tend to be multiple [1, 4]. Extensive and deep ulceration can also be present and may lead to serious GI complications, such as perforation and massive bleeding [2, 11–17]. Therefore, early diagnosis and treatment are of great importance. In our study, mucosal ulceration was observed in the majority of cases (75%). It was documented in 57% of the patients with gastritis and in all patients with esophagitis (100%). Of note, in 2 cases (17%) profound ulcers, resembling the formation of cavities, were observed at endoscopy.
Contrary to previous reports [18–23], the esophagus does not appear to represent the most common site of upper GI tract involvement in our study, as we identified 5 cases of CMV esophagitis (42%) and 7 cases of CMV gastritis (58%). The most frequently affected sites of the upper GI tract were the lower esophagus (33%) and the gastric antrum (42%). Of interest, the lower esophagus was involved in 80% (4/5) of the patients with CMV esophagitis and the antrum in 71% (5/7) of the patients with CMV gastritis. Similar findings were reported in previous studies, which showed that the most commonly affected sites arethe mid-distal esophagus (88%) [1] and the antrum (84%) [4] in esophageal and gastric CMV disease, respectively. In the present study, 2 cases (17%) of diffuse CMV organ involvement were documented (1 patient with diffuse esophagitis and 1 with diffuse gastritis). A few similar cases of diffuse organ involvement and synchronous multiple organ involvement have also been documented in the literature [1, 4]. Synchronous organ involvement seems to be particularly prevalent in duodenal CMV disease, which is associated with gastric disease in 77% of cases [4, 10].
The recommended antiviral therapy for GI CMV disease is i.v. ganciclovir for at least 2–3 weeks [2, 5–6]. Because of its high bioavailability, p.o. valganciclovir is also considered an effective drug [7]. Maintenance therapy with oral valganciclovir is advocated in particular situations, such as in patients with concomitant CMV retinitis and in those receiving high-dose immunosuppression [24, 25]. In this study, sequential therapy with i.v. ganciclovir followed by p.o. valganciclovir was the most common treatment (42%). The antiviral therapy duration ranged between 2 weeks and 2 months, and in 3 patients maintenance therapy was subsequently given. Although very few studies have assessed patient outcomes, upper GI CMV disease has been associated with significant morbidity and mortality [8, 9]. This was also evident in this study, where the 1-year mortality rate reached 25%.
Conclusion
There is increasing evidence that upper GI CMV disease can occur in both immunocompromised patients and apparently healthy individuals. Future studies are needed to identify other potential risk factors for developing this disease. Patients with upper GI CMV infection are usually symptomatic, and mucosal ulceration is often evident at endoscopy. Upper GI CMV is associated with significant mortality; therefore, early diagnosis and adequate antiviral treatment are essential.
References
1 Wang HW, Kuo CJ, Lin WR, et al: The clinical characteristics and manifestations of cytomegalovirus esophagitis. Dis Esophagus 2016;29:392–399. [ Links ]
2 Ozaki T, Yamashita H, Kaneko S, et al: Cytomegalovirus disease of the upper gastrointestinal tract in patients with rheumatic diseases: a case series and literature review. Clin Rheumatol 2013;32:1683–1690. [ Links ]
3 Seo M, Kim do H, Gong EJ, et al: Is follow-up endoscopy necessary in upper gastrointestinal cytomegalovirus disease? Medicine (Baltimore) 2016;95:e3389. [ Links ]
4 Bonetti LR, Losi L, Greagorio C, et al: Cytomegalovirus infection of the upper gastrointestinal tract: a clinical and pathological study of 30 cases. Scand J Gastroenterol 2011;46:1228–1235. [ Links ]
5 You DM, Johnson MD: Cytomegalovirus infection and the gastrointestinal tract. Curr Gastroenterol Rep 2012;14:334–342. [ Links ]
6 Asberg A, Humar A, Rollag H, et al: Oral valganciclovir is noninferior to intravenous ganciclovir for the treatment of cytomegalovirus disease in solid organ transplant recipients. Am J Transplant 2007;7:2106–2113. [ Links ]
7 Len O, Gavaldà J, Aguado JM, et al: Valganciclovir as treatment for cytomegalovirus disease in solid organ transplant recipients. Clin Infect Dis 2008;46:20–27. [ Links ]
8 Siciliano RF, Castelli JB, Randi BA, et al: Cytomegalovirus colitis in immunocompetent critically ill patients. Int J Infect Dis 2014;20:71–73. [ Links ]
9 Galiatsatos P, Shrier I, Lamoureux E, Szilagyi A: Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts. Dig Dis Sci 2005;50:609–616. [ Links ]
10 Péter A, Telkes G, Varga M, et al: Endoscopic diagnosis of cytomegalovirus infection of upper gastrointestinal tract in solid organ transplant recipients: Hungarian single-center experience. Clin Transplant 2004;18:580–584. [ Links ]
11 Featherstone RJ, Camero LG, Khatib R, et al: Massive esophageal bleeding in achalasia complicated by cytomegalovirus esophagitis. Ann Thorac Surg 2995;59:1021–1022. [ Links ]
12 Kanda K, Kume K, Yoshikawa I, et al: Cytomegalovirus esophagitis with massive upper-GI hemorrhage. Gastrointest Endosc 2004;59:741–743. [ Links ]
13 Kaplan CS, Petersen EA, Icenogle TB, et al: Gastrointestinal cytomegalovirus infection in heart and heart-lung transplant recipients. Arch Intern Med 1989;149:2095–2100. [ Links ]
14 Aqel NM, Tanner P, Drury A, et al: Cytomegalovirus gastritis with perforation and gastrocolic fistula formation. Histopathology 1991;18:165–168. [ Links ]
15 Lee HK, Chung DH, Jung J, et al: Three cases of pancreas allograft dysfunction. J Korean Med Sci 2001;15:105–110. [ Links ]
16 Howaizi M, Abboura M, Sbai-Idrissi MS, et al: Cytomegalovirus-associated perforated gastric ulcer healing under antiviral therapy. Dig Dis Sci 2002;47:2380–2382. [ Links ]
17 Mayeux GP, Smith JW: Massive esophageal bleeding from cytomegalovirus esophagitis. Am J Gastroenterol 1990;85:626. [ Links ]
18 Lin WR, Su MY, Hsu CM, et al: Clinical and endoscopic features for alimentary tract cytomegalovirus disease: report of 20 cases with gastrointestinal cytomegalovirus disease. Chang Gung Med J 2005;28:476–484. [ Links ]
19 Goodgame RW: Gastrointestinal cytomegalovirus disease. Ann Intern Med 1993;119:924–935. [ Links ]
20 Chuah SK, Changchien CS, Kuo CM, et al: Gastrointestinal tract cytomegalovirus disease in southwestern Taiwan: a clinical study of 1950 endoscopic biopsies. Chang Gung Med J 2005;28:467–475. [ Links ]
21 Péter A, Telkes G, Varga M, et al: Gastrointestinal cytomegalovirus infections in organ transplant patients. Orv Hetil 2008;149:2463–2470. [ Links ]
22 Ohnuma H, Sato Y, Takayama T, et al: Esophageal cancer complicated by cytomegalovirus esophagitis during chemoradiotherapy: case report. Gastrointest Endosc 2003;57:622–626. [ Links ]
23 Francis ND, Boylston AW, Roberts AH, et al: Cytomegalovirus infection in gastrointestinal tracts of patients infected with HIV-1 or AIDS. J Clin Pathol 1989;42:1055–1064. [ Links ]
24 Patil AJ, Sharma A, Kenney MC, et al: Valganciclovir in the treatment of cytomegalovirus retinitis in HIV-infected patients. Clin Ophthalmol 2010;4:111–119. [ Links ]
25 Kotton CN, Kumar D, Caliendo AM, et al; Transplantation Society International CMV Consensus Group: International consensus guidelines on the management of cytomegalovirus in solid organ transplantation. Transplantation 2010;89:779–795. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
All authors approved the manuscript and agree with its submission to GE – Portuguese Journal of Gastroenterology. All authors have nothing to disclose.
* Corresponding author.
Dr. Susana Marques
Department of Gastroenterology, Centro Hospitalar Lisboa Ocidental
Rua da Junqueira 126
PT–1349-019 Lisbon (Portugal)
E-Mail xsusanamarx@gmail.com
Received: October 10, 2016; Accepted after revision: January 23, 2017
Author Contributions
S. Marques and J. Carmo wrote the manuscript. M. Bispo, S. Ramos, and C. Chagas were responsible for the revision of its contents.














