Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
GE-Portuguese Journal of Gastroenterology
versión impresa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa oct. 2017
https://doi.org/10.1159/000477549
ENDOSCOPIC SNAPSHOT
Underwater Endoscopic Mucosal Resection of a Large Flat Adenoma with Pseudoinvasion in the Rectum
Mucosectomia Underwater de Lesão Plana Adenomatosa com Pseudo-Invasão no Reto
Ana Pontea, Rolando Pinhoa, Luísa Proençaa, Joana Silvaa, Jaime Rodriguesa, Mafalda Sousaa, Xiaogang Wenb, Agostinho Sanchesb, João Carvalhoa
Departments of aGastroenterology and bPathology, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Pseudoinvasive adenoma; Underwater endoscopic mucosal resection; Rectum
Palavras-Chave: Adenoma pseudo-invasivo; Mucosectomia underwater;·Reto
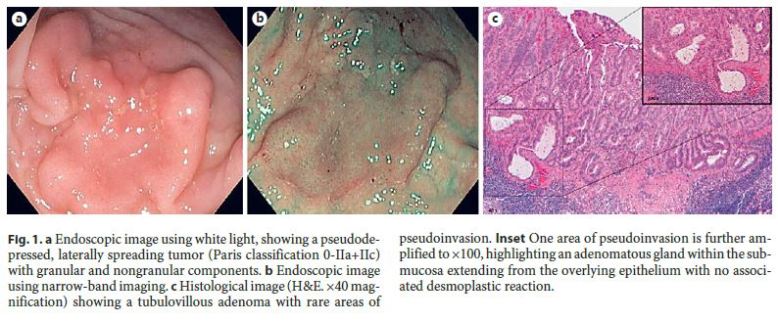
69-year-old male with no relevant personal and family medical history was admitted for endoscopic resection of a rectal laterally spreading tumor. Colonoscopy revealed a 30-mm pseudodepressed, laterally spreading tumor (Paris classification 0-IIa+IIc) with granular and nongranular components. A high-definition colonoscope (CF-H180AL; Olympus Medical Systems, Hamburg, Germany) was used to examine the lesion and its margins using white-light (Fig. 1a) and narrow-band imaging (Fig. 1b) to evaluate the mucosal and vascular patterns, which were regular. Subsequently, an underwater endoscopic mucosal resection (UEMR) was performed, as this technique enables resection of larger fragments and obviates the need of submucosal injection, which is sub-optimal in pseudodepressed lesions. Air insufflation was switched off, luminal air was aspirated, water was instilled using the water jet until complete immersion of the lumen was achieved (Fig. 2a), and the lesion was resected in piecemeal fashion using a conventional 25-mm oval snare (CJ-ADR-23–230–025; Nova LightSystems, Life Partners Europe, Bagnolet, France) and usual electrosurgical settings (Endocut effect 2, ICC 200; ERBE Elektromedizin, Tübingen, Germany) (Fig. 2b, c). A bleeding vessel was identified during the procedure (Fig. 3a) and managed with a hemostatic clip (Fig. 3b). Histological analysis revealed a tubulovillous adenoma with high-grade dysplasia and rare adenomatous glands within the submucosa extending from the overlying epithelium, with no associated desmoplastic reaction, corresponding to an adenoma with misplaced epithelium (Fig. 1c). A follow-up procedure performed 3 months later revealed no residual lesion.
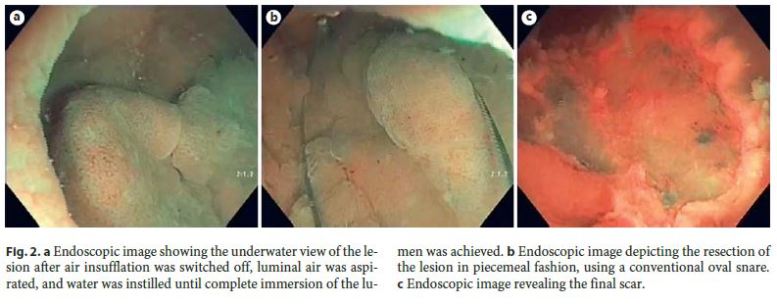

Water immersion preserves the circular configuration of the muscularis propria of the colon while folds of mucosa and submucosa project into the lumen away from the muscle layer, avoiding the need for submucosal injection used in conventional EMR [1, 2]. Bleeding during UEMR is uncommon, and the point of originis clearly identified underwater [1].
Adenoma with misplaced epithelium is a rare entity formerly known as pseudoinvasive adenoma, which corresponds to an extension of the adenomatous glands of an adenoma into the submucosa through minor defects of the muscularis mucosae [3, 4]. The distinction of this entity from an invasive cancer in which neoplastic epithelium, such as desmoplasia, frank atypia, or pleomorphism, is present in the submucosa may be difficult but is crucial as the management and prognosis of an adenoma with misplaced epithelium is identical to an adenomatous polyp [3, 4].
References
1 Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S: Underwater EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc 2012;75:1086–1091. [ Links ]
2 Uedo N, Nemeth A, Johansson GW, Toth E, Thorlacius H: Underwater endoscopic mucosal resection of large colorectal lesions. Endoscopy 2015;47:172–174. [ Links ]
3 Ferreira da Silva MJ, Pinho R, Wen X, Tente D, Leite S, Carvalho J: Adenoma with pseudoinvasion – a crucial differential diagnosis for invasive adenocarcinoma. Gastroenterol Hepatol 2017;4D:96–98. [ Links ]
4 Rodrigues J, Pinho R, Wen X: Two synchronous pseudoinvasive adenomas – twice the caution? GE Port J Gastroenterol 2016;23:324–325. http://dx.doi.org/10.1016/j.jpge.2016.03.005. [ Links ]
Statement of Ethics
This case required informed consent but did not require review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Ana Ponte
Department of Gastroenterology, Centro Hospitalar Vila Nova de Gaia/Espinho
Rua Conceição Fernandes
PT–4434-502 Vila Nova de Gaia (Portugal)
E-Mail ana.ilponte@gmail.com
Received: December 5, 2016; Accepted after revision: February 13, 2017














