Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa out. 2017
https://doi.org/10.1159/000460299
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
A Rare Cause of Dysphagia
Uma causa rara de disfagia
Joana Carvalho, Nídia Zózimo, Fátima Serejo, Margarida Dias, José Velosa
Gastroenterorology Department, Hospital de Santa Maria, Centro Hospital de Lisboa Norte, Lisbon, Portugal
* Corresponding author.
Keywords: Dysphagia; Crohn disease; Esophageal
Palavras-Chave: Disfagia; Doença de Crohn; Esófago
A 21-year-old male patient presented with bloody diarrhea, weight loss (10% of body weight), diffuse abdominal pain, and intermittent solid food dysphagia of 6 months duration. His past medical history was not significant; he had no positive family history and was not taking any medication. The patient was apyretic, had tachycardia and a diffusely painful abdomen without rebound tenderness. Laboratory tests revealed anemia with iron deficiency with a hemoglobin value of 12.4 g/dL and elevated inflammatory parameters (29,470 white blood cells/U, C-reactive protein 18.6 mg/dL, and erythrocyte sedimentation rate 43 mm/h). Abdominal computed tomography revealed diffuse bowel wall thickening of the colon and terminal ileum. Serological screening for cytomegalovirus, human immunodeficiency virus, hepatitis B virus infection, and interferon gamma release assay were negative. The Widal test and bacteriological and parasitological blood/stool tests were negative. Upper endoscopy revealed hyperemia, small erosions, and pseudopolyps of the distal esophagus (Fig. 1), and mild antral hyperemia. Colonoscopy showed edema, deep ulcers and pseudopolyps of all colonic segments. Esophageal biopsies revealed giant multinucleated cells and granulomas suggestive of esophageal Crohn disease (CD). Gastric biopsies revealed diffuse nonatrophic mild gastritis with the presence of Helicobacter pylori . Colonic biopsies were also compatible with active CD. The patient was treated with proton pump inhibitor and systemic corticosteroids, which resulted in complete resolution of the symptoms. The patient remained asymptomatic with maintenance therapy with azathioprine.
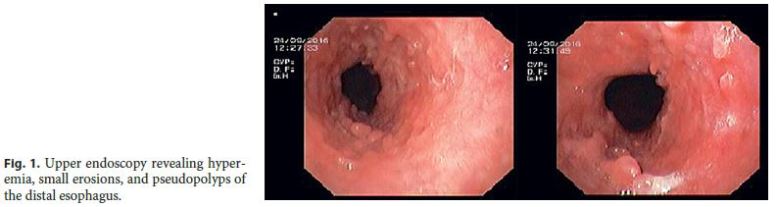
CD is a chronic inflammatory disease that can affect the whole digestive tract. The proximal involvement of the esophagus and stomach is rare (0.5–13% of patients with ileocolic disease) [1]. CD of the esophagus without involvement of the stomach and duodenum is very uncommon (0.2–3% in patients with coexisting ileocolonic disease) and usually does not present with dysphagia [2]. There are no pathognomonic endoscopic findings and the differential diagnosis is with reflux esophagitis, infectious esophagitis, pill esophagitis, tuberculosis, sarcoidosis, Behçet disease, and malignancy [2, 3]. Treatment consists of proton pump inhibitor with systemic corticosteroids or thiopurines/methotrexate. Given the poor prognosis of CD with proximal involvement, a lower threshold for starting anti-TNF therapy is recommended [4]. This report illustrates the endoscopic findings of a rare case of esophageal CD presenting with intermittent dysphagia.
References
1 Zezos P, Kouklakis G, Oikonomou A, Pitiakoudis M, Simopoulos C: Esophageal Crohns disease treated topically with swallowed aerosolized budesonide. Case Rep Med 2010;2010:1–4. [ Links ]
2 Wang W, Ni Y, Ke C, Cheng Q, Lu Q, Li X: Isolated Crohns disease of the esophagus with esophago-mediastinal fistula formation. World J Surg Oncol 2012;10:208–211. [ Links ]
3 Van Hogezand RA, Witte AM, Veenendaal RA, Wagtmans MJ, Lamers CB: Proximal Crohns disease: review of the clinicopathologic features and therapy. Inflamm Bowel Dis 2001;74:328–337. [ Links ]
4 Dignass A, Van Assche G, Lindsay JO, Lémann M, Söderholm J, Colombel JF, et al: The second European evidence-based consensus on the diagnosis and management of Crohns disease: current management. J Crohns Colitis 2010;4:28–62. [ Links ]
Statement of Ethics
Protection of Human and Animal Subjects
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of Data, Right to Privacy, and Informed Consent
The authors declare that no patient data appear in this article.
Disclosure Statement
The authors declare that they have no conflicts of interest.
* Corresponding author.
Dr. Joana Carvalho
Gastroenterorology Department, Hospital de Santa Maria
Centro Hospital de Lisboa Norte, Avenida Professor Egas Moniz
PT–1649-035 Lisbon (Portugal)
E-Mail joana.rita.carvalho@gmail.com
Received: September 26, 2016; Accepted after revision: January 6, 2017
Author Contributions
All authors contributed equally to the elaboration and review of the manuscript.














