Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa out. 2017
https://doi.org/10.1159/000478938
CLINICAL CASE STUDY
Uncommon Solid Pancreatic Neoplasm: The Role of New Modalities of Ultrasound Endoscopy
Neoplasia sólida pancreática incomum: o papel das novas modalidades de ultrassonografia endoscópica
Cátia Leitão, Helena Ribeiro, João Pinto, Ana Caldeira, Eduardo Pereira, António Banhudo
Department of Gastroenterology, Amato-Lusitano Hospital, ULSCB, Castelo Branco, Portugal
* Corresponding author.
ABSTRACT
Undifferentiated carcinoma with osteoclast-like cells is a rare pancreatic neoplasm with unique ultrasound endoscopic features. A 59-year-old female presented with a 3-month history of weight loss. Abdominal computed tomography and endoscopic ultrasound showed a large pancreatic tumor with a heterogeneous echotexture and liver metastasis. Endoscopic ultrasound fine needle aspiration was used to establish the diagnosis. In this case report, we review the endoscopic, clinical, and pathological features of this type of tumor and describe for the first time the endoscopic features of real-time elastography and contrast enhancement. Realtime elastography revealed a heterogeneous predominantly blue pattern suggestive of pancreatic malignancy, and the contrast-enhanced endosonography showed a hypervascular mass and distinctive vascular (solid) and avascular (liquid/ necrotic) components of the lesion, guiding the fine needle aspiration.
Keywords: Undifferentiated carcinoma osteoclast-like cells; Endoscopic ultrasound; Real-time elastography; Contrast enhancement; Pancreas
RESUMO
O carcinoma indiferenciado de células do tipo osteoclástico é uma neoplasia rara com achados únicos de ultrassonografia endoscópica. Mulher, de 59 anos de idade, com história de perda ponderal nos últimos 3 meses. A tomografia computorizada e a ultrassonografia endoscópica mostraram um volumoso tumor pancreático com uma ecotextura heterogénea e metástases hepáticas. A punção aspirativa com agulha fina por ultrassonografia endoscópica estabeleceu o diagnóstico. Este caso clínico fará uma revisão dos achados endoscópicos, clínicos e histológicos deste tipo de tumor e descrever pela primeira vez os achados endoscópicos da elastografia em tempo real e do contraste por ultrassonografia. A elastografia em tempo real revelou um padrão heterogéneo predominante azul, sugestivo de malignidade pancreática e o contraste por ultrassonografia mostrou uma massa hipervascular, diferenciando o componente vascular (sólido) do não vascular (tecido necrótico/líquido) da lesão, orientando a punção com agulha fina.
Palavras-Chave: Carcinoma indiferenciado de células do tipo osteoclástico; ultrassonografia endoscópica; elastografia em tempo real; contraste; pâncreas
Introduction
Undifferentiated carcinoma with osteoclast-like cells (UCOC) accounts for less than 1% of exocrine pancreatic malignancies, with only few reported cases in the literature [1–6]. The true origin of these lesions remains unclearand difficult to evaluate given the rarity of this tumor [3, 4]. These lesions have a distinct appearance when imaged with endoscopic ultrasound (EUS), and they canbe diagnosed via EUS-guided fine needle aspiration [5, 6].
In this case report, we aim to highlight unique ultrasound endoscopic findings of this type of tumor from two new advanced technologies – real-time elastography and contrast enhancement.
Case Report
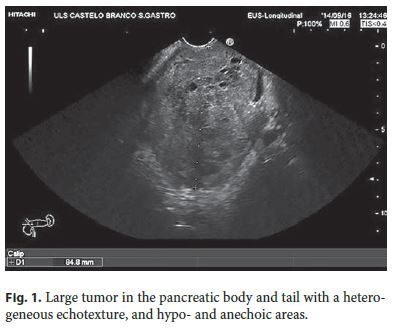
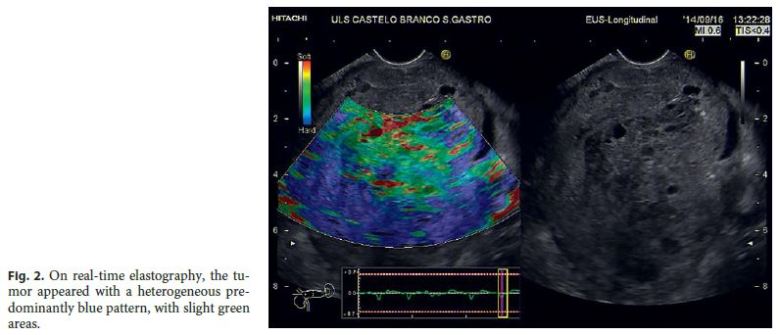
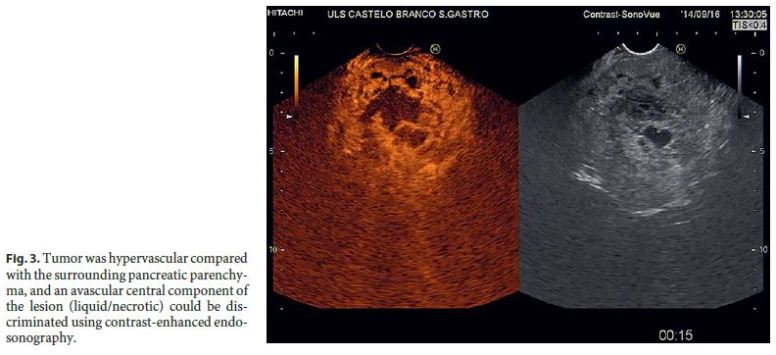
A 59-year-old female was referred to the Gastroenterology Department with weight loss over 3 months and a large pancreatic mass detected on the abdominal computed tomography. There was no previous history of alcohol or tobacco use and no significant past medical or family history. On physical examination, her abdomen was slightly tender in the epigastric area. Laboratory tests revealed mild elevation of transaminases (AST 150 U/L and ALT 83 U/L; normal range, AST <59 U/L and ALT <72 U/L). Otherbiochemical indices were normal. Among the tumor markers examined, carbohydrate antigen 19-9 and carcinoembryonic antigen were increased to 700 U/mL (normal range, 0–37 U/mL) and 1,385 ng/mL (normal range, <5 ng/mL), respectively. Abdominal computed tomography showed a large mass in the pancreatic tail with a cyst-like low-density area and an area of necrosis and liver metastases. On EUS, the tumor was a large lesion in the pancreatic body and tail, with a mean diameter of 84 mm and a heterogeneous echotexture, with hypo- and anechoic areas (Fig. 1). Increased vascularity was assessed by power color Doppler ultrasound. Realtime elastography was used in order to assess the relative stiffness of tumor tissue compared to the surrounding pancreatic parenchyma; it showed a heterogeneous predominantly blue pattern, with slight green areas (Fig. 2). After baseline EUS examination, a bolus of 2.4 mL of SonoVue ® (Bracco Imaging, Milan, Italy) was administered intravenously, and contrast-enhanced endosonography (CE-EUS) was performed according to the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) guidelines and recommendations on the clinical practice of Contrast Enhanced Ultrasound on nonhepatic applications [7]. CE-EUS revealed a hypervascularized tumor compared to the surrounding pancreatic parenchyma and discriminated an avascular central component of the lesion, corresponding to a necrotic area. Therefore, the use of CE-EUS allowed us to select the best areas to puncture, avoiding the necrotic area with great improvement of the diagnostic yield (Fig. 3). The tumor was sampled twice using a 22-gauge aspiration needle (Cook Medical Inc., Bloomington, IN, USA). Abundant specimens were obtained for cytological and histopathological examination. A part of the material was preserved for cell block.
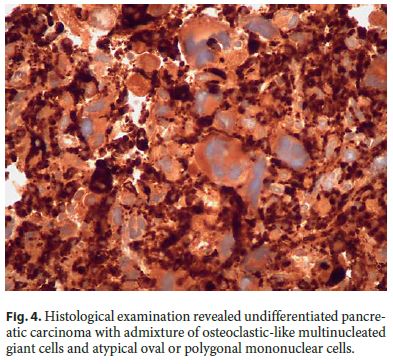
Histological examination revealed undifferentiated pancreatic carcinoma with admixture of osteoclastic-like multinucleated giant cells and atypical oval or polygonal mononuclear cells. The hematoxylin and eosin and CKAE1/AE3 immunohistochemical stain images showed glands invaded by inflammatory cells including osteoclast-like giant cells. Additional immunohistochemical study revealed positivity for vimentin and CD68 and keratin, favoring mesenchymal and epithelial origin (Fig. 4).
The patient underwent two cycles of gemcitabine (1,480 mg). Chemotherapy was stopped because of pancytopenia. The patient died 2 months after the diagnosis.
Discussion
Pancreatic giant cell tumors are rare tumors of debatable origin. There are three histopathological subtypes: osteoclast-like giant cell tumor, pleomorphic giant cell carcinoma, and mixed varieties [7]; however, since 2010, the World Health Organization has grouped them together as UCOC [8].
Pancreatic giant cell tumors have unique clinical and pathological characteristics. Similar to pancreatic adenocarcinoma, UCOC of the pancreas tend to occur in the elderly with similar prevalence in women and men [4]. Most patients present with epigastric pain, abdominal distension and jaundice related to malignant biliary obstruction. In this case, the patient presented only weight loss. The patient did not report any alcohol or tobacco use, and she had no history of pancreatitis, similar to the reports in the literature, suggesting that the risk factors may differ from those of pancreatic adenocarcinoma [6].
EUS is an indispensable method for detection, characterization, and differential diagnosis of solid pancreatic lesions [9]. EUS fine needle aspiration established the diagnosis in our case report. The EUS appearance was different from the typical adenocarcinoma. UCOC tended to be larger and appeared markedly heterogeneous with well-demarcated hyper- and hypoechoic areas closely opposed within the same lesion. Using advanced technologies such as real-time elastography and contrast enhancement, pancreatic ductal adenocarcinoma and other solid lesions (including rare neoplasms and benign lesions) may be distinguished [9, 10]. UCOC showed a heterogeneous predominantly blue pattern on real-time elastography, present mainly in pancreatic malignant tumors. UCOC was a hypervascular mass when compared to the surrounding parenchyma, in contrast towhat is described for pancreatic adenocarcinoma [9, 10]. Other differential diagnoses to consider were neuroendocrine tumors and serous microcystic neoplasia as they typically appear as hyperenhancing masses in the arterial phase, like we described in our case [11]. To the best of our knowledge, this is the first case reported in the literature describing the endoscopic features of these new EUS techniques.
The prognosis in patients with UCOC appears similar to that seen in pancreatic adenocarcinoma overall [4]. It is possible that patients with pleomorphic mononuclear and multinucleated giant cells follow an aggressive course with early metastasis and poor prognosis, as was the case in our patient, who died 2 months after the diagnosis [4–6]. Unfortunately, due to the rarity of this neoplasm, there is a lack of large studies or individual experience concerning the management of this tumor.
References
1 Pimentel A, Leitão S, Dias N, Cipriano MA, Leite J, Santos RM, et al: Undifferentiated osteoclastic-type giant cell carcinoma. Acta Med Port 2010;23: 931–936. [ Links ]
2 Shah S, Mortele KJ: Uncommon solid pancreatic neoplasms: ultrasound, computed tomography, and magnetic resonance imaging features. Semin Ultrasound CT MRI 2007;28:357–370. [ Links ]
3 Leighton CC, Shum DT: Osteoclastic giant cell tumor of the pancreas. Am J Clin Oncol 2001;24:77–80. [ Links ]
4 Moore JC, Hilden K, Bentz JS, Pearson RK, Adler DG: Osteoclastic and pleomorphic giant cell tumors of the pancreas diagnosed via EUS-guided FNA: unique clinical, endoscopic, and pathological findings in a series of 5 patients. Gastrointest Endosc 2009;69:162–165. [ Links ]
5 Temesgen WM, Wachtel M, Dissanaike S: Osteoclastic giant cell tumor of the pancreas. Int J Surg Case Rep 2014;5:175–179. [ Links ]
6 Nai GA, Amico E, Gimenez VR, Guilmar M: Osteoclast-like giant cell tumor of the pancreas associated with mucus-secreting adenocarcinoma. Pancreatology 2005;5:279–284. [ Links ]
7 Piscaglia F, Nelsoe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, et al: The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 2012;33:33–59. [ Links ]
8 Lüttges J: Whats new? The 2010 WHO Classification for Tumours of the Pancreas. Pathologe 2011;32(suppl 2):332–336. [ Links ]
9 Saftoiu A, Gheonea DI, Cartana T, Streba C: Advanced endoscopic ultrasound imaging: contrast-enhanced endoscopic ultrasound (low MI, high MI), including 3D techniques in Pancreatic imaging. Video J Encycl GI Endosc 2013;1(suppl 2):534–536. [ Links ]
10 Iglesias-Garcia J, Larino-Noia J, Abdulkader I, Forteza J, Dominguez-Munoz JE: Quantitative endoscopic ultrasound elastography: an accurate method for the differentiation of solid pancreatic masses. Gastroenterology 2010;139:1172–1180. [ Links ]
11 Dietrich CF, Sharma M, Hocke M: Contrastenhanced endoscopic ultrasound. Endosc Ultrasound 2012;1:130–136. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors declare no conflict of interest.
* Corresponding author.
Dr. Cátia Leitão
Department of Gastroenterology, Amato-Lusitano Hospital, ULSCB
Avenida Pedro Álvares Cabral
PT–6000-080 Castelo Branco (Portugal)
E-Mail catia.f.leitao@gmail.com
Received: October 3, 2016; Accepted after revision: December 14, 2016














