Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa out. 2017
https://doi.org/10.1159/000454987
CLINICAL CASE STUDY
Endoscopic Management of Colonic Perforation due to Ventriculoperitoneal Shunt: Case Report and Literature Review
Abordagem endoscópica de perfuração do cólon por cateter de derivação ventrículo-peritoneal: caso clínico e revisão da literatura
Ana Rita Alvesa, Sofia Mendesa, Sandra Lopesa, Alexandre Monteirob, David Perdigotoa, Pedro Amaroa, Luís Toméa
aGastroenterology Department and bGeneral Surgery A Department, Coimbra Hospital and University Centre, Coimbra, Portugal
* Corresponding author.
ABSTRACT
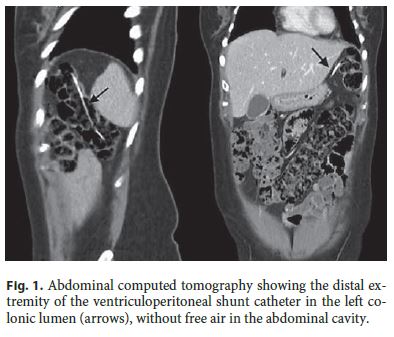
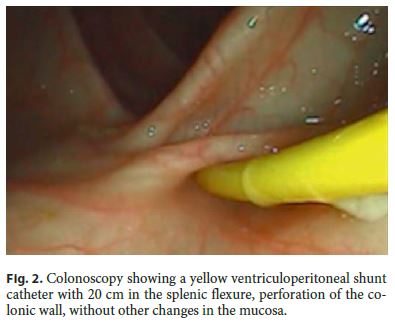
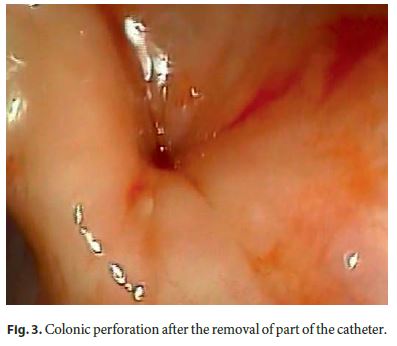
The authors report the case of a 41-year-old woman with a colonic perforation due to a ventriculoperitoneal shunt (VPS) catheter. Left-sided colonic perforation was diagnosed by abdominal computed tomography 28 years after shunt placement, following acute meningitis caused by Escherichia coli . The proximal end of the VPS was exteriorized and it was decided to remove the distal end by colonoscopy. After pulling out the catheter with a polypectomy snare, it broke at the site where it was entering the colon, leaving a small perforation in the colonic wall which was closed with 2 endoclips. The endoluminal fragment of the catheter, being 20 cm in length, was removed through the rectum. The patient is asymptomatic at the 12-month follow-up. A review of the literature regarding 9 endoscopically managed cases of digestive tract perforation caused by VPS is presented.
Keywords: Ventriculoperitoneal shunt; Intestinal perforation; Colonoscopy
RESUMO
Os autores descrevem o caso de uma mulher de 42 anos com perfuração do cólon por cateter de derivação ventrículo-peritoneal (DVP) colocado 28 anos antes. No contexto de meningite aguda a Escherichia coli , o estudo complementar com tomografia computadorizada abdominal identificou a extremidade distal do cateter de DVP no interior do lúmen do cólon esquerdo. Após remoção da extremidade ventricular do cateter, optou-se pela tentativa de extração da extremidade intra-cólica por colonoscopia. Durante a extração do cateter com ansa de polipectomia, constatou-se secção do mesmo no local de entrada na parede cólica, observando-se um pequeno orifício. Procedeu-se ao encerramento da perfuração com 2 endoclips e extração do fragmento livre endoluminal do cateter, com cerca de 20 cm, pelo reto. A doente permanece assintomática após 12 meses de seguimento. Uma revisão da literatura identificou 9 casos de perfuração do tubo digestivo por cateter de DVP tratados com endoscopia.
Palavras-Chave: Derivação ventrículo-peritoneal; perfuração cólica;·colonoscopia
Introduction
Ventriculoperitoneal shunts (VPS) are associated with several complications, including obstruction, infection, migration, and perforation [1]. The incidence of gastrointestinal tract perforation is rare, occurring in 0.1–0.7% of patients [2]. Colon is the most frequent site of perforation and clinical manifestations can range from asymptomatic to life-threatening conditions [3]. Treatment must be individualized and depends on clinical presentation. Conservative management, endoscopy, and surgery have been performed [3, 4].
We report the case of a 41-year-old woman with a colonic perforation due to a migrated VPS treated with colonoscopy. The perforation was diagnosed by abdominal computed tomography (CT), following 2 episodes of acute meningitis due to Escherichia coli , 28 years after VPS placement. A review of the literature regarding endoscopically managed cases was performed.
Clinical Case
A 41-year-old woman presented to the emergency department with headache, fever, vomiting, and phonophobia in the previous 24 h. She had neck stiffness and blood laboratory tests showed a slight increase in C-reactive protein. The patient had a past history of acute meningitis caused by E. coli 4 months earlier treated with ceftriaxone and placement of a VPS 28 years earlier, after surgery to remove a brain tumor. She was chronically medicated with omeprazole. Head CT in the emergency department showed a collection next to the ventricular extremity of the VPS, suggesting an abscess. Lumbar puncture revealed turbid cerebrospinal fluid, decreased glucose levels, increased protein levels and increased polymorphonuclear neutrophils. The patient was admitted with the diagnosis of acute meningitis complicated by a brain abscess. Empirical therapy with ceftriaxone, vancomycin and metronidazole was initiated and cerebrospinal fluid analysis was later positive for E. coli . A complementary study with abdominal and pelvic CT showed that the distal extremity of the VPS catheter was located within the colonic lumen of the left hypochondriac region, without free air in the abdominal cavity (Fig. 1). The proximal part of the catheter was removed by neurosurgery and a temporary external diversion was placed. The patient denied recent abdominal pain or in any other moment since the VPS placement and there was no identified previous event or change in her chronic medication. She presented a favorable clinical course and was discharged 44 days after admission. Following a combined evaluation between general surgery and gastroenterology, it was decided to perform a colonoscopy with the purpose of removing the distal end of the catheter, which remained in the abdominal cavity and colonic lumen. The procedure was performed 1 month after the second episode of acute meningitis, under deep sedation with propofol, with bowel preparation and prophylactic antibiotherapy with amoxicillin and clavulanate, given the possibility of contamination of the abdominal cavity with bowel contents during the procedure. Colonoscopy revealed a yellow tube with about 2 0 cm in the splenic flexure, perforation of the colonic wall, without other changes in the mucosa (Fig. 2). After one attempt of removal by pulling out the catheter distally with a polypectomy snare, the catheter broke at the site of entrance in the colonic wall, leaving a small orifice (Fig. 3). The patient remained stable, without abdominal distention or signs of peritoneal irritation throughout the procedure. Colonic perforation was closed with 2 endoclips (Fig. 4) and the remaining free fragment of the catheter in the colonic lumen was extracted with the snare. Abdominal X-ray 6 h later did not show free air in the abdominal cavity. The patient was discharged 2 days after the procedure and was asymptomatic at the 12-month follow-up, maintaining regular clinical evaluation.

Discussion
VPS is a standard device used to correct hydrocephalus and its components are a proximal catheter, which is placed into the cerebral ventricle, a valve, and a distal catheter, which is placed in the peritoneal cavity [3]. VPS-related complications include infection (peritonitis, ventriculitis, and meningitis), obstruction, migration, and perforation [1, 5]. Complications are reported in 24–47% of cases, with about 25% of these being abdominal complications [3, 5]. Migration of the peritoneal end of the catheter can occur into the abdominal wall, gastrointestinal tract, bladder, vagina, scrotum, and mediastinum [5]. Bowel perforation is a rare complication, occurring in 0.1–0.7% of patients [2]. Colon is the most common site of perforation, which can result in potentially serious complications. Death is reported in up to 15% of cases. Nonetheless, signs of peritonitis occur in less than 25% of patients and most of the cases are asymptomatic or exhibit catheter protrusion through the anus or mouth [3, 6]. This patient denied abdominal pain and there were no radiological signs of free air in the abdominal cavity. Surgical exploration has documented abundant chronic fibrous tissue around the site where the catheter enters the colon. This fibrosis does not permit the spillage of bowel contents into the peritoneal cavity and may explain why these perforations can occur without acute presentation [3].
Given the potentially life-threatening presentation, clinicians should be aware of the possibility of bowel perforation in patients with VPS [3]. Diagnosis is obvious when anal or oral protrusion of the catheter occurs, but some situations should raise the suspicion of this complication, namely ventriculitis or meningitis due to an unusual enteric organism, such gram-negative or anaerobic, or a CT scan showing pneumocephalus without another cause [3, 7]. This patient had 2 episodes of acute meningitis due to E. coli a very long time after VPS placement (28 years). This highlights the importance of a high index of suspicion for early recognition and prompt management [3].
The treatment of a VPS perforating the bowel must be individualized, taking into account the clinical presentation [3, 4, 7, 8]. Three principles are important: external drainage of the proximal part until the cerebrospinal fluid is biochemically near-normal and sterile on culture, intravenous antibiotics, and removal of the perforating part of the catheter [2, 3]. If there is no peritonitis or abdominal abscess, percutaneous or endoscopic removal of the abdominal end of the catheter can be performed without surgery. Surgery must be performed in cases of intraabdominal infection or when the fistulous tract does not close spontaneously after percutaneous or endoscopic removal. Laparotomy, laparoscopy and transanal repair of colonic perforation have been reported [3, 4, 9]. Our patient was first submitted to the removal of the ventricular end of the catheter and external drainage. The distal end was not completely removed, since it broke at the site where it was entering the colonic wall. This could imply some risk of contamination of the peritoneal cavity. However, the communication between peritoneal cavity and colonic lumen was interrupted. Additionally, leaving the distal end of a malfunctioning shunt within the abdomen is a common practice in some patients in whom a shunt revision is necessary. These segments are frequently referred to as abandoned VPS. Reports of complications of abandoned VPS are rare and the morbidity and mortality of such complications are unknown [1]. Conservative management of asymptomatic patients has already been described with progressive migration of an abandoned VPS during 7 years from the abdominal cavity to the hepatic flexure, liver parenchyma and gastric antrum, documented in serial CT scans [1].
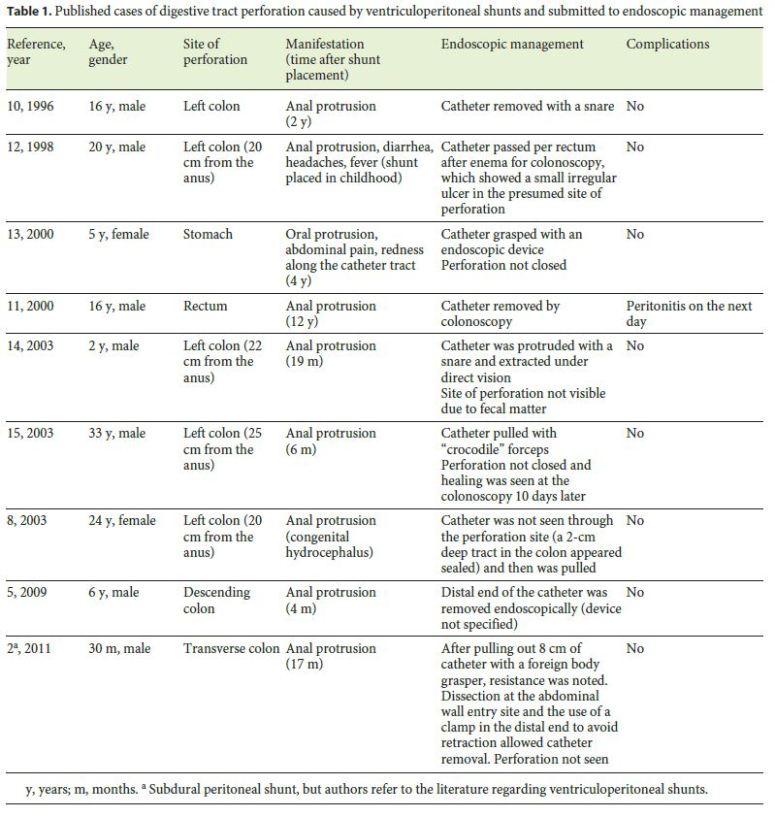
To our knowledge, 9 cases of endoscopic management of VPS perforating the digestive tract have been published in English (Table 1). Patients age, time between VPS placement and presentation, site of perforation, clinical manifestations, and endoscopic devices for catheter removal are described. Closure of the perforation was not performed in most cases; in 1 case, the site was not seen in the colonoscopy because of fecal matter and in some cases this detail was not mentioned. It is believed that the perforation site can seal off spontaneously, because penetration is a chronic process whereby the catheter tip gradually erodes the wall of the viscus and is sealed by a fibrous sheath at the site of entry [8, 10]. Nonetheless, there is a report of subsequent peritonitis requiring laparotomy and temporary colostomy after endoscopic removal of the distal catheter from an asymptomatic bowel perforation [11]. Therefore, leaving the bowel perforation unrepaired may still render the patient at risk of subsequent peritonitis [4]. The application of endoclips, when feasible, is a simple endoscopic procedure that may prevent this rare complication and may have contributed to the favorable outcome of this patient.
Perforation of the digestive tract caused by VPS is a rare event. Since endoscopy has been used to manage some cases, gastroenterologists may have an increased role in the nonsurgical management of these patients.
References
1 Rinker EK, Osborn DA, Williams TR, Spizarny DL: Asymptomatic bowel perforation by abandoned ventriculoperitoneal shunt. J Radiol Case Rep 2013;7:1–8. [ Links ]
2 Oliveira SB, Monteiro IM: Endoscopic management of transanal protrusion of subdural peritoneal shunt in a child. J Pediatr Gastroenterol Nutr 2011;53:465–467. [ Links ]
3 Birbilis T, Zezos P, Liratzopoulos N, Oikonomou A, Karanikas M, Kontogianidis K, et al: Spontaneous bowel perforation complicating ventriculoperitoneal shunt: a case report. Cases J 2009;2:8251. [ Links ]
4 Chiang LL, Kuo MF, Fan PC, Hsu WM: Transanal repair of colonic perforation due to ventriculoperitoneal shunt: case report and review of the literature. J Formos Med Assoc 2010;109:472–475. [ Links ]
5 Vuyyuru S, Ravuri SR, Tandra VR, Panigrahi MK: Anal extrusion of a ventriculo peritoneal shunt tube: endoscopic removal. J Pediatr Neurosci 2009;4:124–126. [ Links ]
6 Thiongo GM, Luzzio C, Albright AL: Ventriculoperitoneal shunt perforations of the gastrointestinal tract. J Neurosurg Pediatr 2015;16:36–41. [ Links ]
7 Hai A, Rab AZ, Ghani I, Huda MF, Quadir AQ: Perforation into gut by ventriculoperitoneal shunts: a report of two cases and review of the literature Indian Assoc Pediatr Surg 2011;16:31–33. [ Links ]
8 Yousfi MM, Jackson NS, Abbas M, Zimmerman RS, Fleischer DE: Bowel perforation complicating ventriculoperitoneal shunt: case report and review. Gastrointest Endosc 2003;58: 144–148. [ Links ]
9 Knuth J, Detzner M, Heiss MM, Weber F, Bulian DR: Laparoscopy for a ventriculoperitoneal shunt tube dislocated into the colon. JSLS 2013; 17: 675–678. [ Links ]
10 Brown SR, Gourlay R, Battersby RD: Sigmoidoscopic neurosurgery? Treatment of an unusual complication of ventriculoperitoneal shunting. Br J Neurosurg 1996;10:419–420. [ Links ]
11 Chen HS: Rectal penetration by a disconnected ventriculoperitoneal shunt tube: an unusual complication. Chang Gung Med J 2000;23:180–184. [ Links ]
12 Brownlee JD, Brodkey JS, Schaefer IK: Colonic perforation by ventriculoperitoneal shunt tubing: a case of suspected silicone allergy. Surg Neurol 1998;49:21–24. [ Links ]
13 Park CK, Wang KC, Seo JK, Cho BK: Transoral protrusion of a peritoneal catheter: a case report and literature review. Childs Nerv Syst 2000;16:184–189. [ Links ]
14 Sharma A, Pandey AK, Radhakrishnan M, Kumbhani D, Das HS, Desai N: Endoscopic management of anal protrusion of ventriculoperitoneal shunt. Indian J Gastroenterol 2003;22:29–30. [ Links ]
15 Pikoulis E, Psallidas N, Daskalakis P, Kouzelis K, Leppäniemi A, Tsatsoulis P: A rare complication of a ventriculoperitoneal shunt resolved by colonoscopy. Endoscopy 2003;35:463. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Ana Rita Alves
Serviço de Gastrenterologia
Centro Hospitalar e Universitário de Coimbra
Av. Bissaya Barreto e Praceta Prof. Mota Pinto
PT–3000-075 Coimbra (Portugal)
E-Mail alvess.anarita@gmail.com
Received: September 26, 2016; Accepted after revision: December 6, 2016














