Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa out. 2017
https://doi.org/10.1159/000478940
ORIGINAL ARTICLE
Quality in Colonoscopy: Beyond the Adenoma Detection Rate Fever
Qualidade em Colonoscopia: Para além da Febre da Taxa de Deteção de Adenomas
Filipe Taveiraa, Miguel Areiaa, b, Luís Elvasa, Susana Alvesa, Daniel Britoa, Sandra Saraivaa, Ana Teresa Cadimea
aDepartment of Gastroenterology, Portuguese Oncology Institute, Coimbra, and bCINTESIS – Center for Research in Health Technologies and Information Systems, Faculty of Medicine, University of Porto, Porto, Portugal
* Corresponding author.
ABSTRACT
Background: Colonoscopy quality is a hot topic in gastroenterological communities, with several actual guidelines focusing on this aspect. Although the adenoma detection rate (ADR) is the single most important indicator, several other metrics are described and need reporting. Electronic medical reports are essential for the audit of quality indicators; nevertheless, they have proved not to be faultless. Aim: The aim of this study was to analyse and audit quality indicators (apart from ADR) using only our internal electronic endoscopy records as a starting point for improvement. Methods: An analysis of electronically recorded information of 8,851 total colonoscopies from a single tertiary centre from 2010 to 2015 was performed. Results: The mean patient age was 63.4 ± 8.5 years; 45.5% of them were female, and in 14.6% sedation was used. Photographic documentation was done in 98.4% with 10.7 photographs on average, and 37.4% reports had <8 pictures per exam. Bowel preparation was rated as adequate in 67%, fair in 27% and inadequate in 4.9% of cases. The adjusted caecal intubation rate (CIR) was 92%, while negative predictors were inadequate preparation (OR 119, 95% CI 84–170), no sedation (OR 2.39, 95% CI 1.81–3.15), female gender (OR 1.61, 95% CI 1.38–1.88) and age ≥ 65 years (OR 1.56, 95% CI 1.34–1.82). In 28% of patients, a snare polypectomy was performed, correlating with adequate preparation (OR 5.75, 95% CI 3.90–8.48), male gender (OR 1.82, 95% CI 1.64–2.01) and age ≥ 65 years (OR 1.25, 95% CI 1.13–1.37; p < 0.01) as positive predictors. An annual evolution was observed with improvements in photographic documentation (10.7 vs. 12.9; p < 0.001), CIR (91 vs. 94%; p = 0.002) and adequate bowel preparation ( p = 0.004). Conclusions: There is much more to report than the ADR to ensure quality in colonoscopy practice. Better registry systematization and integrated software should be goals to achieve in the short term.
Keywords: Colonoscopy; Quality of health care; Quality improvement; Electronic health records; Gastroenterology standards
RESUMO
Introdução: A qualidade em colonoscopia tem sido um tópico de importante discussão com várias orientações publicadas nesta área. Embora a taxa de deteção de adenomas (ADR) seja o indicador mais importante, vários outros indicadores estão descritos e precisam ser estudados/publicados. Os registos médicos eletrónicos são essenciais para a auditoria de indicadores de qualidade, mas provaram não ser infalíveis. Objetivo: Analisar e auditar os indicadores de qualidade, além do ADR, recorrendo apenas à base de dados de endoscopia do nosso centro, como ponto de partida para a melhoria. Métodos: Análise do registo eletrónico de 8,851 colonoscopias totais realizadas em um único centro no período 2010–2015. Resultados: A idade média dos pacientes foi de 63.4 ± 8.5 anos, 45.5% do sexo feminino. Em 14.6%, foi utilizada sedação. Documentação fotográfica em 98.4%, com média de 10.7 fotografias por exame e 37.4% com menos de 8 fotos por exame. A preparação intestinal foi avaliada como adequada em 67%, razoável em 27% e inadequada em 4.9%. A taxa de intubação cecal ajustada (CIR) foi de 92%, com preparação inadequada (OR 119, 95% CI 84–170), exame sem sedação (OR 2.39, 95% CI 1.81–3.15), sexo feminino (OR 1.61, 95% CI 1.38–1.88) e idade ≥ 65 (OR 1.56, 95% CI 1.34–1.82) como preditores negativos. Em 28%, foi realizada polipectomia, correlacionando-se com preparação adequada (OR 5.75, 95% CI 3.90–8.48), sexo masculino (OR 1.82, 95% CI 1.64–2.01) e idade ≥ 65 (OR 1.25, 95% CI 1.13–1.37; p < 0.01). Da evolução anual destacar melhorias na documentação fotográfica (10.7 vs. 12.9; p < 0.001), taxa de intubação cecal (91 vs. 94%; p = 0.002) e preparação intestinal adequada ( p = 0.004). Conclusões: Há muito mais para reportar, além do ADR, de modo a garantir colonoscopias com qualidade. Uma maior sistematização no registo e softwares integrados devem ser objetivos a alcançar no curto prazo.
Palavras-Chave: Colonoscopia; Qualidade em saúde; Registo eletrónico; Normas em gastrenterologia
Introduction
Colonoscopy is widely used for the screening, diagnosis and treatment of lower gastrointestinal tract disorders (with emphasis on colon and rectum cancer as leading causes of morbidity and mortality), being generally safe and accurate. Estimates say that around a third of all colonoscopies are for screening purposes [1, 2]. Colonoscopy quality is a hot topic now as both the American Society for Gastrointestinal Endoscopy (ASGE) and the European Society of Gastrointestinal Endoscopy (ESGE) have developed and reviewed guidelines in this area, with continuous efforts in improving not only colonoscopy quality but also the adherence to the goals proposed [3–5].
The adenoma detection rate (ADR) is the most described and studied quality indicator for screening colonoscopy, considered to be the single most relevant indicator with an influence, for example, on the appearance of interval cancer [5, 6]. However, many other indicators have been published as goals to achieve in a quality colonoscopy (not only for screening purposes). For example, bowel preparation results or caecal intubation rates (CIRs) and other performance measures need to be studied and publicized. In fact, work based on public reporting of colonoscopy quality indicators appears to improve endoscopists results and patients trust [7, 8]. The report of colonoscopy quality metrics is often dependent on electronic medical records. Lieberman et al. [9] (in 2007) were one of the first groups to provide an integrative colonoscopy report proposing the need to mention several aspects, such as the patients medical background, risk assessment (e.g., American Society of Anesthesiologists [ASA] score), procedure indication, technical description and findings of the exam. An initial assessment and follow-up plan should be mentioned in the report. Recently, Bretthauer et al. [10] introduced several recommendations, on behalf of the ESGE, suggesting the use of electronic reporting integrated in the patients medical records and with a connection with other databases, such as pathology results. The audit of colonoscopy reports has been the focus of some recent studies which found multiple insufficiencies; an example is a recent Canadian work suggesting that almost 20% of the reports evaluated were classified as poor, leading to a call for additional research in the area [11, 12]. Also, a recent review on this topic found that incomplete reporting and lack of interoperability of health-care electronic systems seem to be a major problem to solve in colonoscopy report quality [13].
Our goal was to analyse and audit quality indicators, apart from the ADR, using only our internal electronic endoscopy records as a starting point to improve the care provided at our endoscopic unit.
Methods
We retrospectively analysed all colonoscopies performed between January 2010 and December 2015 at our department, accessing only the electronic endoscopy database of the Gastroenterology Department of the Portuguese Oncology Institute of Coimbra.
Patients
All patients referred for colonoscopy were enrolled in this work during the above-mentioned period. Patients were all ≥ 18 years of age, and indications for colonoscopy were polyp removal, surveillance after resection of colorectal lesions or cancer treatment and screening due to a positive family history of colorectal cancer or adenomas. All patients had a previous appointment at the hospital, and written informed consent for the procedure was obtained. Bowel preparation was accomplished using verbal and written information.
Settings
The Portuguese Oncology Institute of Coimbra is a tertiary referral centre mainly for patients with cancer or premalignant conditions. The Endoscopy Unit of the Gastroenterology Department comprises 3 endoscopy rooms, provides upper and lower endoscopies as well as endoscopic ultrasonography exams and was equipped with Olympus Evis Exera II (Olympus, Tokyo, Japan) video processors and 160 and 180 series endoscopes during the study period (2010–2015). Most endoscopic exams in Portugal are still performed without any sedation; thus, we had anaesthetic support available in only 1 room 3 days per week, and there was a recovery room with a capacity for 3 patients. During the study period, the staff was composed of 5 gastroenterology consultants and 1 resident. In cases of Propofol sedation, an anaesthesiologist and a second nurse dedicated to sedation were present in the room.
Definitions
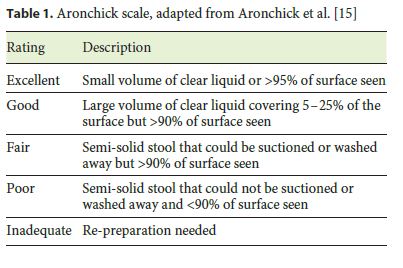
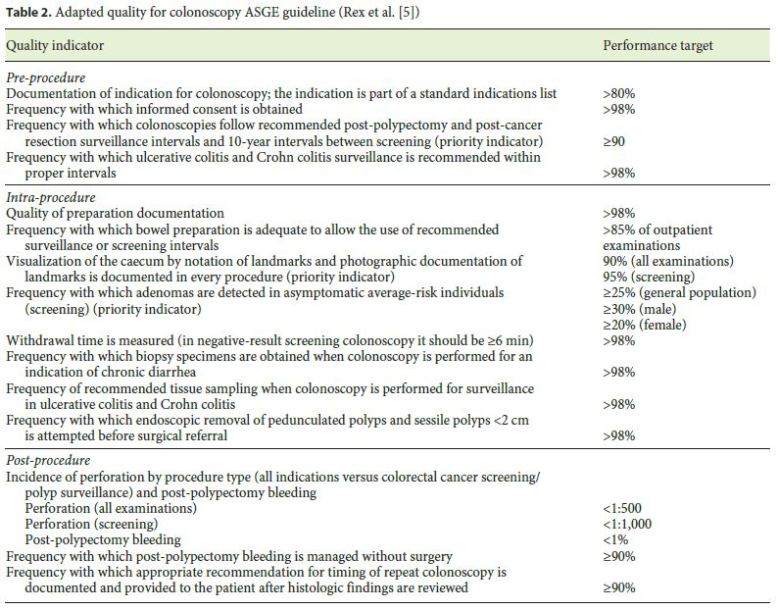
Demographic data, full registry completion, duration of the exam, iconographic documentation, overall polyp detection rate, percentage of exams using sedation and identification of the equipment used were directly obtained after consultation of the endoscopy database. We assumed a minimum of 8 pictures per exam to be necessary to achieve a proper documentation [14]. Bowel preparation was graded by the endoscopist according to the Aronchick scale (Table 1) as adequate (excellent or good), fair or inadequate (poor or inadequate) [15]. CIR was defined as photographic documentation of caecal landmarks and was adjusted for inadequate bowel preparations and stenosis according to the ASGE guidelines [5]. An estimated polyp detection rate was defined as the percentage of exams with at least 1 snare polypectomy. Not only screening procedures but also all other indications were reported; however, the electronic database does not allow the identification of diminutive polyps removed by biopsy forceps. Thus, this rate cannot be judged as the polyp detection rate described in the literature. All colonoscopy quality indicators were analysed using the recommendations by the ASGE guidelines (Table 2) [5].
Statistical Analysis
Results were expressed as means and standard deviations for continuous variables with a normal distribution or proportions and 95% CI for categorical variables. Differences in proportions were analysed by the χ 2 test. Multivariate logistic regression analysis was performed to identify factors associated with the detection of polyps and with reaching the caecum. A p value <0.05 was considered as statistically significant. All statistical analyses were performed using the SPSS software package, version 23 (Statistical Package for the Social Sciences, IBM Corporation, Armonk, NY, USA).
Results
Between 2010 and 2015, a total of 8,851 colonoscopies were recorded at our unit database and were considered for this analysis. Board-certified specialists or supervised fellows in training performed all colonoscopies (Table 3).
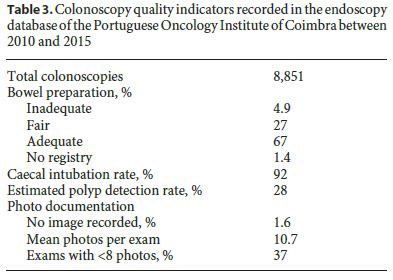
The mean patient age was 63.4 ± 8.5 years; 45.5% were women. Approximately 99% of all colonoscopies were performed according to an indication that is included in a standard list of internationally accepted appropriate indications. At our unit, most colonoscopies are done without any sedation. Accordingly, only 14.6% of all procedures were done under sedation with Propofol, administered by a certified anaesthesiologist, and in <1% of colonoscopies benzodiazepine sedation was administered by the gastroenterologist. In all cases, vital signs were permanently monitored. The average exam time was 27 ± 8.5 min with an absent record in 1.1% of the exams. Unfortunately, withdrawal time is not recorded in our database. Iconographic documentation was present in 98.4% of the exams, with an average of 10.7 pictures per exam, and in our colonoscopy database, 37.4% had 7 pictures or less. The unique identification of the equipment used in every exam was recorded in 97.7% of cases.
Bowel preparation results were classified as adequate in 66.7%, fair in 27% and inadequate in 4.9% of patients. Evaluation of the bowel cleanliness was missing in 1.4% of the cases. The split-dose regimen was introduced in late 2015 as a systematically recommended bowel preparation scheme and provided a rise to 91% for adequate preparations.
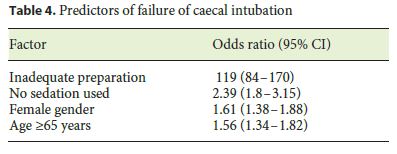
CIR was classified according to the ASGE guidelines with an overall adjusted result of 92% of the exams after removal of inadequate preparations and stenosis. Predictors for failure to reach the caecum were inadequate preparation (OR 119, 95% CI 84–170), exams with no use of sedation (OR 2.39, 95% CI 1.8–3.15), female gender (OR 1.61, 95% CI 1.38–1.88) and age ≥ 65 years (OR 1.56, 95% CI 1.34–1.82) (Table 4).
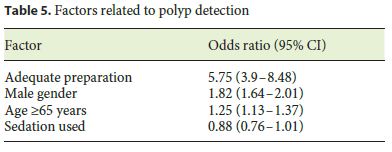
Polypectomy was performed in 2,473 colonoscopies with an estimated 28% polyp detection rate for all indications and not just for screening exams. Finding a polyp was related with several factors, such as adequate preparation (OR 5.75, 95% CI 3.9–8.48), male gender (OR 1.82, 95% CI 1.64–2.01) and age ≥ 65 years (OR 1.25, 95% CI 1.13–1.37) (Table 5). Sedation had no influence on polyp detection (OR 0.88, 95% CI 0.76–1.01). All polyps larger than 2 cm ( n = 148) were removed by endoscopic approach, with only 2% of them needing a subsequent surgical approach.
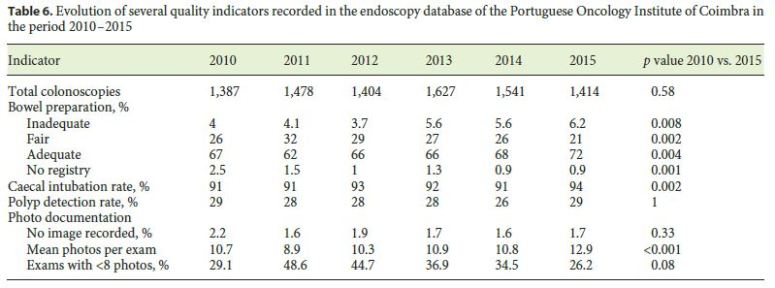
We followed the evolution of several parameters during the studied time, which are summarized in Table 6. Globally, we came up with a positive trend, highlighting the improvement in photographic documentation (mean number of photos per exam: 10.7 vs. 12.9; p < 0.001) and CIR (91 vs. 94%; p = 0.002). Moreover, in this period, a statistically significant improvement in adequate preparations was accomplished (67 vs. 72%; p = 0.004).
Discussion
This study was implemented due to the necessity at our endoscopy unit to perceive the quality metrics of the work we make and the care we provide to our patients. Nowadays, the number of audits in health care is growing, and colonoscopy is not exempted from that development, with reports showing a positive relationship between the public reporting of quality indicators, endoscopists practice and associated results [8].
We report all the quality indicators that our electronic database allows to retrieve directly. Our bowel preparation results seem to agree with the levels recommended by the ASGE. In fact, >98% of the reports had a documented bowel cleanliness, and there were <15% of inadequate preparations [5]. However, the use of less validated evaluations of bowel cleanliness, such as the Aronchick scale, can mask the true preparation results, with a large proportion of fair preparation results being in a grey area with possibly great variability between professionals assessment. This problem can be easily solved by implementing in the software the currently most validated scale for bowel preparation evaluation, the Boston Bowel Preparation Scale [16]. In fact, the correct reporting of segmental bowel preparation is fundamental for detecting colonic lesions and for increasing the alertness of the endoscopist in future colonoscopies [17]. Our overall results for bowel preparation are similar to the published data on standard bowel preparation regimens, with a great improvement in these results after the introduction of the split-dose regimen for all our exams in late 2015 [18]. In the study period, a statistically significant improvement in adequate preparations was accomplished (67 vs. 72%; p = 0.004), but there was also a significant increase (4 vs. 6%; p = 0.008) in poor preparations, at this time with no obvious justification. A possible explanation would be the patients difficulties in understanding the new split-dose regimen, but as we have shown, from these preparations >90% were adequate. In fact, in recent years, bowel preparation has been a concern at our unit, and efforts have been made in terms of educational incentives for our patients, with good results in improving overall bowel preparation results [19].
The Aronchick scale for bowel preparation was used at our unit during the study period, as at that time no ideal scale was defined, and it was the one available in the software. In addition, it was used in an ongoing randomized trial about bowel preparation at our unit [19]. Later, with publications demonstrating the superiority of the Boston Bowel Preparation Scale in terms of reproducibility, we started to use that scale in 2016, and it now is the scale adopted by an updated version of the software.
Our CIR is globally satisfying with a recent improvement of our results and a positive trend during the study period ( p = 0.002). The predictive factors of CIR failure we studied are in line with the published literature, namely sedation, age and bowel preparation; we identified female sex as a risk factor for colonoscopy incompleteness; however, some inconsistencies in the literature seem to exist [20, 21]. Note that for a proper CIR we need to have iconographic documentation of the caecum and associated landmarks to guarantee the quality of our performance [5]. We assumed that at least 8 pictures per exam are necessary for a proper evaluation of all findings and landmarks, following some previous European recommendations and some in-house experience [14]. At least 3 photographs for the segmental documentation of bowel preparation, at least 2 photographs to document the caecum and ileocaecal valve, and 3 photographs for the documentation of findings and other important landmarks are needed. This policy was first implemented in 2015, and we could observe an immediate improvement in our photographic documentation results, with a statistically significant improvement in the mean number of photographs per exam (10.7 vs. 12.9; p < 0.001). We still have a large proportion of exams with <8 photos, but there is a trend for a positive progress (29.1 vs. 26.2%; p = 0.08). Although there is no previous work to strongly justify the 8-pictures cut-off, a good documentation of caecal landmarks has shown a positive correlation with the improvement of colonoscopy quality metrics, such as the polyp detection rate [22].
Regarding adenoma or polyp detection, as we cannot access histology reports from our endoscopy database, an estimation of the polyp detection rate was only possible because all snare polypectomies were registered in that database. In addition, the polyp and adenoma detection rates used in many studies are from screening colonoscopies only, while we used our entire database, not looking at the indication due to the very low prevalence of screening colonoscopies in our database. Some of the factors described in the literature for higher polyp detection rates were confirmed in our study, such as male gender or age ≥ 65 years and the dubious contribution of sedation [23, 24]. Consequently, we can answer the question if a global objective for polyp detection in colonoscopy is possible, regardless of the indication, since every colonoscopy offers a therapeutic opportunity.
Our study has several limitations, the first being its retrospective nature, based on information present only in our database, relying solely on what the endoscopist registered at the moment of the exam. Although a limitation, we understand it as an opportunity for improvement, and a recent review from the ESGE makes recommendations about the criteria an endoscopy unit program needs to fulfil in order to guarantee quality, such as an electronic registry with a connection with the patient record and pathology databases, restricting the areas for free text entries, greater emphasis on patients comfort, reporting of quality indicators and follow-up instructions [10]. Due to this work, we realized that our unit software lacks several indicators, for example, valuable information for our internal quality audits is missing, such as pathologic diagnosis, validated scales, a measure of withdrawal time or polypectomy removal identification per exam. In fact, like other national and worldwide endoscopy units, we still do not have a direct connection with pathology databases, the inability to retrieve our ADR being another important limitation. In addition, the frequency with which colonoscopies were performed following the recommended post-polypectomy and post-cancer resection surveillance intervals was not measured, since these data are also not automatically extracted from the software. Improvements of this problem should be pursued at our unit but also nationally, for example, promoted by the national Portuguese Society of Digestive Endoscopy (SPED), with proposals for the standardization of reports and available software solutions [25, 26].
In conclusion, quality in endoscopy is a current hot topic in gastroenterology practice and should be a concern of every endoscopy unit. The systematization of registries should be a major concern, including proper connections with pathology and internal patient programs, searching the best technological solutions, and preservation of ethical and moral concerns. In fact, we have shown that there is more beyond the ADR to worry about in colonoscopy quality metrics, and reporting our own experience is intended to be a wake-up call to improve the quality of care we are eager to provide.
References
1 Peery AF, et al: Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143:1179–1187.e1–e3. [ Links ]
2 Global Burden of Disease Cancer Collaboration, et al: Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol 2017;3:524–548. [ Links ]
3 Rembacken B, et al: Quality in screening colonoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE). Endoscopy 2012;44:957–968. [ Links ]
4 Rutter MD, et al: The European Society of Gastrointestinal Endoscopy Quality Improvement Initiative: developing performance measures. United European Gastroenterol J 2016;4:30–41. [ Links ]
5 Rex DK, et al: Quality indicators for colonoscopy. Gastrointest Endosc 2015;81:31–53. [ Links ]
6 Kaminski M, Regula J, Kraszewska E: Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 2010;362:1795–1803. [ Links ]
7 Kahi CJ, et al: Impact of a quarterly report card on colonoscopy quality measures. Gastrointest Endosc 2013;77:925–931. [ Links ]
8 Abdul-Baki H, et al: Public reporting of colonoscopy quality is associated with an increase in endoscopist adenoma detection rate. Gastrointest Endosc 2015;82:676–682. [ Links ]
9 Lieberman D, et al: Standardized colonoscopy reporting and data system: report of the Quality Assurance Task Group of the National Colorectal Cancer Roundtable. Gastrointest Endosc 2007;65:757–766. [ Links ]
10 Bretthauer M, et al: Reporting systems in gastrointestinal endoscopy: requirements and standards facilitating quality improvement: European Society of Gastrointestinal Endoscopy position statement. United European Gastroenterol J 2016;4:172–176. [ Links ]
11 Beaulieu D, Barkun A, Martel M: Quality audit of colonoscopy reports amongst patients screened or surveilled for colorectal neoplasia. World J Gastroenterol 2012;18:3551–3557. [ Links ]
12 Hadlock SD, et al: The quality of colonoscopy reporting in usual practice: are endoscopists reporting key data elements? Can J Gastroenterol Hepatol 2016;2016:1929361. [ Links ]
13 Sharma RS, Rossos PG: A review on the quality of colonoscopy reporting. Can J Gastroenterol Hepatol 2016;2016:9423142. [ Links ]
14 Rey JF, Lambert R; ESGE Quality Assurance Committee: ESGE recommendations for quality control in gastrointestinal endoscopy: guidelines for image documentation in upper and lower GI endoscopy. Endoscopy 2001;33:901–903. [ Links ]
15 Aronchick CA, et al: A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc 2000;52:346–352. [ Links ]
16 Calderwood AH, Jacobson BC: Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc 2010;72:686–692. [ Links ]
17 Jain D, et al: Importance of reporting segmental bowel preparation scores during colonoscopy in clinical practice. World J Gastroenterol 2015;21:3994–3999. [ Links ]
18 Bucci C, et al: Optimal bowel cleansing for colonoscopy: split the dose! A series of metaanalyses of controlled studies. Gastrointest Endosc 2014;80:566–576.e2. [ Links ]
19 Elvas L, et al: Impact of personalised patient education on bowel preparation for colonoscopy: prospective randomised controlled trial. GE Port J Gastroenterol 2017;24:22–30. [ Links ]
20 Dafnis G, et al: Patient factors influencing the completion rate in colonoscopy. Dig Liver Dis 2005;37:113–118. [ Links ]
21 Hsu CM, et al: Factors that influence cecal intubation rate during colonoscopy in deeply sedated patients. J Gastroenterol Hepatol 2012;27:76–80. [ Links ]
22 Thoufeeq MH, Rembacken BJ: Meticulous cecal image documentation at colonoscopy is associated with improved polyp detection. Endosc Int Open 2015;3:E629–E633. [ Links ]
23 Barret M, Boustiere C, Canard JM, Arpurt JP, et al: Factors associated with adenoma detection rate and diagnosis of polyps and colorectal cancer during colonoscopy in France: results of a prospective, nationwide survey. PLoS One 2013;8:e68947. [ Links ]
24 Nakshabendi R, Berry AC, Munoz JC, John BK: Choice of sedation and its impact on adenoma detection rate in screening colonoscopies. Ann Gastroenterol 2016;29:50–55. [ Links ]
25 Raju GS, et al: Natural language processing as an alternative to manual reporting of colonoscopy quality metrics. Gastrointest Endosc 2015;82:512–519. [ Links ]
26 Imler TD, et al: Multi-center colonoscopy quality measurement utilizing natural language processing. Am J Gastroenterol 2015;110: 543–552. [ Links ]
Statement of Ethics
The authors have no ethical conflicts to disclose. Written informed consent for the procedure was obtained from the patients.
Disclosure Statement
The authors declare no conflicts of interest.
* Corresponding author.
Dr. Filipe Taveira
Portuguese Oncology Institute of Coimbra
Av. Bissaya Barreto, 98
PT–3000-075 Coimbra (Portugal)
E-Mail fctav@hotmail.com
Received: February 7, 2017; Accepted after revision: June 20, 2017
Author Contributions
Filipe Taveira: conception and design of the work, analysis and interpretation of data for the work, drafting the work, final approval of the version to be published and agreement to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and solved.
Miguel Areia: conception and design of the work, analysis and interpretation of data for the work, revising critically the draft for important intellectual content, final approval of the version to be published and agreement to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Luis Elvas, Susana Alves, Daniel Brito, Sandra Saraiva, and Ana Teresa Cadime: acquisition of data for the work, revising critically the draft for important intellectual content, final approval of the version to be published and agreement to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.














