Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.4 Lisboa ago. 2017
https://doi.org/10.1159/000452690
CLINICAL CASE STUDY
Intestinal Obstruction by Giant Meckels Diverticulum
Oclusão Intestinal por Divertículo de Meckel Gigante
Gustavo Capelão, Miguel Santos, Sandra Hilário, Mónica Laureano, João Nobre, Inês Gonçalves
General Surgery Department, Centro Hospitalar de Leiria/Pombal, Leiria, Portugal
* Corresponding author.
ABSTRACT
Background: Meckels diverticulum is the most common congenital anomaly of the small bowel and is caused by the incomplete obliteration of the omphalomesenteric duct during the eighth week of gestation. Methods: We report the case of a 51-year-old male who presented to the emergency department with epigastric pain, vomiting, and abdominal distension. Clinically, he had a high intestinal obstruction without any mechanical cause on computed tomography scan. A median laparotomy was proposed. Results: An internal ileum hernia was identified twisted around a giant Meckels diverticulum with a mesodiverticular artery, coursing from the base of the mesentery to the diverticulum. A small bowel segmental resection was performed, containing the diverticulum. Histology revealed a 15-cm long Meckels diverticulum with no heterotopic mucosa. Conclusion: Small bowel obstruction due to an internal ileum hernia twisted around a giant Meckels diverticulum with a mesodiverticular artery is very rare, and its diagnosis is challenging, requires a high level of suspicion, and it is only performed by exploratory surgery.
Keywords: Intestinal obstruction; Meckels diverticulum; Internal hernia; Mesodiverticular artery
RESUMO
Contexto: O divertículo de Meckel é a malformação congénita mais frequente do intestino delgado e deve-se ao encerramento incompleto do canal onfalomesentérico cerca da 8ª semana de gestação. Métodos: Apresentamos o caso de um doente de 51 anos de idade que recorre ao serviço de urgência por dor epigástrica, vómitos e distensão abdominal. Apresentava um quadro clínico de oclusão intestinal alta sem evidência na tomografia computorizada de causa mecânica para a oclusão. Foi proposta laparotomia exploradora. Resultados: Identificouse uma hérnia interna de intestino delgado em torno de um divertículo de Meckel gigante cuja ponta estava aderente ao mesentério devido a persistência de uma artéria divertículo-mesentérica. Realizámos resseção segmentar de intestino delgado, contendo o divertículo. A anatomia patológica foi compatível com divertículo de Meckel com 15 cm sem presença de mucosa heterotópica. Discussão: A oclusão intestinal de Intestino Delgado devido a hérnia interna em torno de um divertículo de Meckel gigante com persistência da artéria diverticulomesentérica é muito raro e o seu diagnóstico é dificil, requer alto nível de suspeição e só é feito após cirurgia exploradora.
Palavras-Chave: Oclusão intestinal; Divertículo de Meckel;·Hérnia interna; Artéria diverticulo-mesentérica
Introduction
Meckels diverticulum is a true diverticulum that arises from the antimesenteric border of the small bowel, and it is known by the rule of twos [1], as its length and diameter usually do not exceed 5 cm (2 inches) and 2 cm, respectively, and in the vast majority of cases, it is located 60 cm (2 feet) from the ileocecal valve [2]. Moreover, most of them (53%) are diagnosed in the first 2 years of life, and the probability of becoming symptomatic decreases with age. Its incidence is about 2% according to autopsy reviews [3], the male:female ratio is 2: 1, and only 2–4% become symptomatic [1]. The main clinical presentations are gastrointestinal bleeding, intestinal obstruction, and diverticulitis [1].
In children, gastrointestinal bleeding is the most frequent clinical presentation [4], mainly due to the presence of heterotopic acid-secreting gastric mucosa in the diverticulum, although pancreatic, jejunal, and endometrial mucosa can also be found in the diverticulum [5].
In adults, intestinal obstruction is the most frequent clinical presentation [4, 6], mainly due to intussusceptions or intestinal volvulus and rarely due to diverticulitis, diverticular torsion, or Littrés hernia (abdominal wall hernia that involves the Meckels diverticulum).
With this clinical case, we present an even more unusual presentation of Meckels diverticulum due to the presence of a mesodiverticular artery, also known as vitelline artery, coursing from the base of the mesentery to the diverticulum, under which the small bowel became entrapped and incarcerated [2].
Clinical Case
A 51-year-old male with diabetes, dyslipidemia, and overweight presented to the Emergency Department due to abdominal distension, vomitus, and epigastric pain which had started 16 h before. He had no fever, no respiratory distress, and a normal blood pressure (127/68 mm Hg) and heart rate (70 bpm). The abdomen had no palpable hernias, was distended with diffuse pain on palpation, and had no signs of peritonitis. There was a worsening of pain intensity despite prescribed analgesia. Rectal exam was normal and abdominal sounds were increased with metallic tones. Blood analyses (hemogram, amylase, lipase, cardiac enzymes, and C-reactive protein) were within normal values.
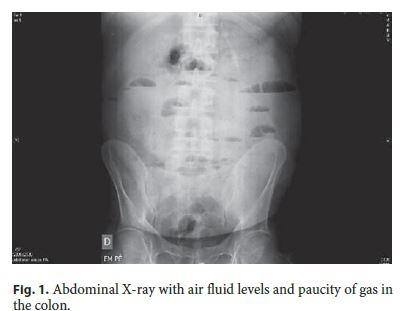
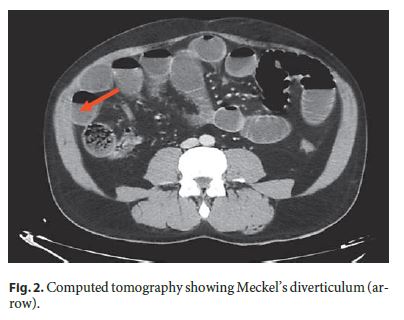
Abdominal X-ray (Fig. 1) revealed small bowel with air fluid levels and paucity of gas in the colon, and abdominopelvic computed tomography showed an abrupt stop of the small bowel without a clear cause (Fig. 2).
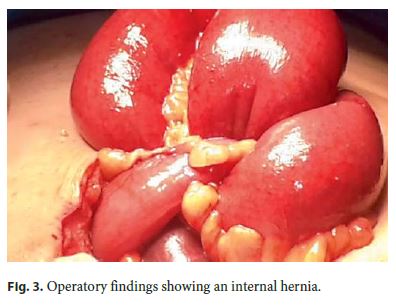
Intravenous fluids were administered and a nasogastric tube was inserted with immediate drainage of stasis liquid. A median laparotomy was performed, as laparoscopy was not practicable. Operatory findings were an internal small bowel hernia (Fig. 3), which was reduced (Fig. 4), and a 15-cm long Meckels diverticulum with the presence of a mesodiverticular artery, which was ligated (Fig. 5), followed by segmental small bowel resection including the diverticulum with a primary termino-terminal manual anastomosis. The pathologic findings revealed a Meckels diverticulum with no heterotopic mucosa.


Discussion
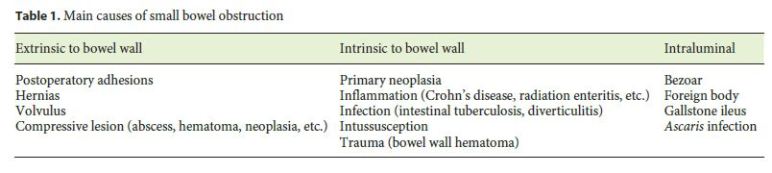
Meckels diverticulum results from the incomplete obliteration of the omphalomesenteric duct between the 5th and 7th week of gestation and is the most common anomaly (90%) resulting from this incomplete obliteration [7], although it is a rare cause of small bowel obstruction in adulthood. Small bowel obstructions can be divided into 3 main groups [8] (Table 1).
Postoperatory adhesions are the main cause (60–85%) of small bowel obstruction, followed by neoplasms (20%) and hernias (10%) [9].
Obstructions due to internal hernias represent only 5% of all obstructions caused by abdominal hernia [10], as inguinal, umbilical, epigastric, incisional, femoral, and diaphragmatic hernias account for the remaining 95%. Internal hernias can result either from trauma/surgery (40%) or are due to congenital anomalies (60%).
This last type results from the incomplete mesenteric fixation to the retroperitoneum during gestation, most of them are paraduodenal and are responsible for 1% of small bowel obstructions [9]. Therefore, the other group of internal hernias due to congenital anomalies (foramen of Winslow, supravesical, mesenteric, etc.) where the internal hernia is included due to the presence of a mesodiverticular artery, accounts for less than 1% of small bowel obstruction cases.
Despite the rarity of this kind of hernia, symptoms are similar to the vast majority of causes of small bowel obstruction: nausea, vomiting, abdominal distension, constipation, and abdominal pain refractory to painkillers [11]. The diagnosis is not only clinical but also confirmed by imaging exams [12]. Abdominal X-ray with air fluid levels in the small bowel and paucity of gas in the colon is very typical. According to the literature, abdominopelvic computed tomography has a 90–95% sensibility and a 96% specificity for small bowel obstruction, and in 95% of the cases, it provides not only information about the exact location and etiology of the obstruction, but also indirect signs of small bowel suffering [12].
Enteroclysis is seldom used because of the prevalence of computed tomography. Although, when computed tomography is unavailable and when X-ray and clinical findings are nondiagnostic, enteroclysis can give diagnostic and prognostic information. If the contrast appears in the colon 6–24 h after the exam, treatment with medical therapy is highly possible [12], with intravenous fluids and decompression with nasogastric tube. If there is no evidence of strangulated hernia or bowel suffering, two thirds will be cured medically. In the other one third, surgical therapy is mandatory [11].
Conclusion
Small bowel obstruction due to an internal ileum hernia twisted around a giant Meckels diverticulum with a mesodiverticular artery is very rare, and its diagnosis is challenging, requires a high level of suspicion, and it is only performed by exploratory surgery.
References
1 Kliegman R, Stanton B, St Geme J, Schor N: Intestinal duplications, Meckel diverticulum, and other remnants of the omphalomesenteric duct; in Behrman R, (ed): Nelson Textbook of Pediatrics, ed 20. Philadelphia, Elsevier, 2016, pp 1804–1805. [ Links ]
2 Holcomb G, Murphy J, Ostlie D: Meckel diverticulum; in Peter S (ed): Ashcrafts Pediatric Surgery, ed 6. New York, Elsevier Saunders, 2014, pp 548–552. [ Links ]
3 Zani A, Eaton S, Rees C, Pierro A: Incidentally detected Meckel diverticulum: to resect or not to resect? Ann Surg 2008;247:276–281. [ Links ]
4 Cameron J, Cameron A: The management of diverticulosis of the small bowel; in DeFrancesco K (ed): Current Surgical Therapy, ed 11. Philadelphia, Elsevier Saunders, 2014, pp 128–132. [ Links ]
5 Ferri F: Meckel diverticulum; in Ferri F (ed): Ferris Clinical Advisor 2016, ed 1. Philadelphia, Elsevier, 2016, p 774. [ Links ]
6 Akbulut S, Yagmur Y: Giant Meckels diverticulum: an exceptional cause of intestinal obstruction. World J Gastrointest Surg 2014; 6:47–50. [ Links ]
7 Snyder C: Meckel diverticulum; in Coran A, Adzick N, Krummel T, Laberge J, Shamberger R, Caldamone A (eds): Pediatric Surgery, ed 7. Philadelphia, Elsevier Saunders, 2012, pp 1085–1092. [ Links ]
8 Roline C, Reardon R: Disorders of the small intestine; in Marx J, Hockberger R, Walls R, Biros M, Danzl D, Gausche-Hill M, et al (eds): Rosens Emergency Medicine, ed 8, Philadelphia, Elsevier Saunders, 2014, pp 1216–1224. [ Links ]
9 Mizell J, Turnage R: Intestinal obstruction; in Feldman M, Friedman L, Brandt L (eds): Sleisenger and Fordtrans Gastrointestinal and Liver Disease, ed 10, Philadelphia, Elsevier Saunders, 2016, pp 2154–2170. [ Links ]
10 Dunbar K, Jeyarajah D: Abdominal Hernias and Gastric Volvulus; in Feldman M, Friedman L, Brandt L (eds): Sleisenger and Fordtrans Gastrointestinal and Liver Disease, ed 10, Philadelphia, Elsevier Saunders, 2016, pp 407–425. [ Links ]
11 Rosen M, Ponsky J, Townsend C, Evers B: Meckel diverticulectomy; in Champagne B (ed): Atlas of surgical techniques for the upper GI tract and small bowel, ed 1. Philadelphia, Saunders, 2010, pp 224–227. [ Links ]
12 Ferri F: Small bowel obstruction; in Ferri F (ed): Ferris Clinical Advisor 2016, ed 1. Philadelphia, Elsevier, 2016, pp 1141–1142. [ Links ]
Statement of Ethics
The procedures followed comply with the ethical standards of the human experimentation committee responsible and are in accordance with the World Medical Association and the Declaration of Helsinki. The authors followed their institutions protocols to access to the patient data, and it was done with the unique purpose of the scientific investigation and scientific disclosure. No patient data appears in this article, and the patient authorized the submission and publication of this work.
Disclosure Statement
The authors declare that there are no conflicts of interests in this article. This work received no contributions, subsidy, or bourse.
* Corresponding author.
Dr. Gustavo Capelão
General Surgery Department, Centro Hospitalar de Leiria/Pombal
Rua das Olhalvas
PT–2410-197 Leiria (Portugal)
E-Mail gustavocapelao@gmail.com
Received: July 26, 2016; Accepted after revision: September 23, 2016














