Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.3 Lisboa jun. 2017
https://doi.org/10.1159/000453071
ENDOSCOPIC SNAPSHOT
Sporadic Jejunal Lateral Spreading Tumor: A Rare Cause of Recurrent Jejunojejunal Intussusception
Lesão em tapete esporádica no jejuno: causa rara de invaginação jejunojejunal recorrente
Ana Pontea, Rolando Pinhoa, Adélia Rodriguesa, Amélia Tavaresb, Joana Ferreirab, Miguel Mendesb, Silvia Costab, João Carvalhoa
Departments of aGastroenterology and bGeneral Surgery, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
* Corresponding author.
Keywords: Deep enteroscopy; Lateral spreading tumor; Enteric invagination
Palavras-Chave: Enteroscopia profunda; lesão em tapete; invaginação entérica
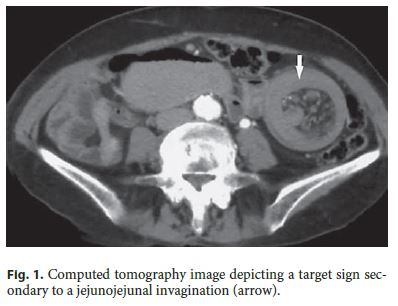
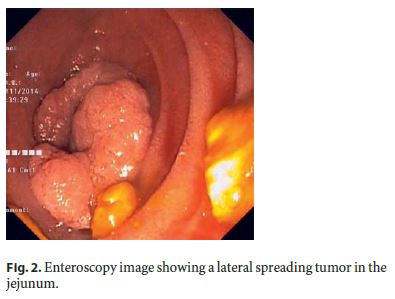
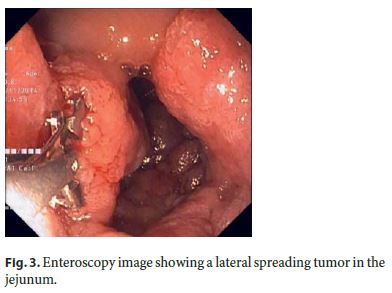
A previously healthy 74-year-old woman with no relevant family medical history was referred to our department to investigate a jejunojejunal intussusception incidentally diagnosed in an abdominal ultrasound performed for evaluation of self-limited episodes of abdominal pain and vomiting. To further investigate the ultrasound findings, computed tomography (CT) was performed and revealed a target sign resulting from an extensive jejunojejunal invagination that involved a large edematous jejunal segment and mesenteric blood vessels and leading to proximal dilation of small-bowel loops with air-fluid levels inside (Fig. 1). Due to partial obstruction and absence of an underlying lesion identified on CT, the patient was referred to antegrade single balloon enteroscopy (Olympus SIF-Q180, Japan) that revealed a type 0-IIa (Paris classification) granular lateral spreading tumor, measuring approximately 4 cm and occupying four fifths of the luminal circumference in the proximal jejunum (Fig. 2 , 3). As endoscopic mucosal resection (EMR) was considered high risk, tattooing was performed and biopsy samples were obtained. Histology revealed a tubulovillous adenoma with low-grade dysplasia and foci of high-grade dysplasia. The patient underwent a laparoscopic enterectomy, whose histology confirmed the initial diagnosis. After surgery, the patient remained asymptomatic.
In adult intussusception there is an underlying cause in more than 90% of the cases, with tumors representing the most frequent etiology [1]. Benign and malignant small-bowel tumors are rare and account for approximately 3–6% of all gastrointestinal neoplasms [2]. With the advent of capsule endoscopy and deep enteroscopy (DE), the reported incidence of small-bowel tumors has increased [2]. Although it accurately identifies adult intussusception, CT may be unrevealing in the evaluation of incomplete small-bowel obstruction and small-bowel tumors [1, 3] . In these cases, DE may provide additional diagnostic information [4] . Moreover, DE allows biopsy sampling and therapeutic interventions [2, 3]. Removal of small-bowel adenomas is advisable due to their predisposition for malignancy.
The boundaries of therapeutic enteroscopy are being continuously expanded [4] and include nowadays smallbowel EMR, as described in a recent series [5] . In this case, EMR was considered high risk, given the longitudinal and circular extension of the lesion, which could be associated with a high rate of incomplete resection, perforation, or delayed stenosis. Hence, laparoscopic surgery was considered a safer therapeutic option.
References
1 Honjo H, Mike M, Kusanagi H, Kano N: Adult intussusception: a retrospective review. World J Surg 2015;39:134–138. [ Links ]
2 Islam RS, Leighton JA, Pasha SF: Evaluation and management of small-bowel tumors in the era of deep enteroscopy. Gastrointest Endosc 2014;79:732–740. [ Links ]
3 Sun B, Shen R, Cheng S, Zhang C, Zhong J: The role of double-balloon enteroscopy in diagnosis and management of incomplete small-bowel obstruction. Endoscopy 2007;39:511–515. [ Links ]
4 Pinho R: The vanishing frontiers of therapeutic enteroscopy. GE Port J Gastroenterol 2015;22:133–134. [ Links ]
5 Kröner PT, Sancar A, Fry LC, Neumann H, Mönkemüller K: Endoscopic mucosal resection of jejunal polyps using double-balloon enteroscopy. GE Port J Gastroenterol 2015;22:137–142. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval
by the appropriate ethics committee.
Disclosure Statement
The authors have nothing to disclose.The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Ana Ponte
Department of Gastroenterology, Centro Hospitalar Vila Nova de Gaia
Rua Conceição Fernandes
PT–4434-502 Vila Nova de Gaia (Portugal)
E-Mail ana.ilponte@gmail.com
Received: September 26, 2016; Accepted after revision: October 12, 2016














