Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.2 Lisboa abr. 2017
https://doi.org/10.1159/000450902
ENDOSCOPIC SNAPCHOT
Dieulafoys Lesion: The Role of Endoscopic Ultrasonography as a Roadmap
Lesão de Dieulafoy: Papel do Mapeamento por Ecoendoscopia
Rita Barosaa, Sara Piresb, Pedro Pinto-Marquesa, José António Pereirac, Tiago Bilhimc
aDepartment of Gastroenterology, Hospital Garcia de Orta, Almada, bGastroenterology Department, Hospital do Espírito Santo, Évora, and cRadiology Department, Hospital de São José, Centro Hospitalar de Lisboa Central, Lisbon, Portugal
* Corresponding author.
Keywords: Gastrointestinal endoscopy; Endosonography;·Gastrointestinal hemorrhage; Vascular malformations
Palavras-Chave: Endoscopia gastrointestinal; Endossonografia;·Hemorragia gastrointestinal; Malformações vasculares
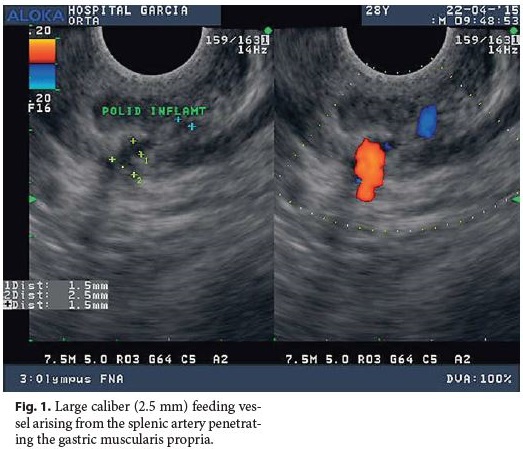
A 28-year-old man without any remarkable past medical history presented with hematemesis and hemodynamic instability. There was no significant past medical history. He denied any medication intake, namely nonsteroidal anti-inflammatory drugs, alcohol abuse, or smoking habits. Upper gastrointestinal endoscopy (UGE) revealed fresh blood and a giant clot covering the gastric body and fundus. Repeated UGE showed no mucosal defect. Radial endoscopic ultrasound (EUS) was performed, indicating a submucosal vessel arising in the greater curvature of the proximal gastric body which identified a Dieulafoys lesion as the possible source of bleeding. Considering clinical stability, EUS-guided therapy with linear scope was planned for the next morning when the scope was available, but rebleeding occurred. UGE was performed with a therapeutic scope, as the site of bleeding was already identified and active bleeding was expected. Thus, the advantages of a dual channel scope, which is more easily maneuvered, would outweigh the advantagesof using the echoendoscope, which has the main benefit when the Dieulafoys lesion cannot be identified on UGE because it is no longer bleeding. UGE revealed an adherent clot in the suspected Dieulafoys lesion location previously described on EUS. After the first clip deployment, massive bleeding occurred. Hemostasis was achieved after adrenalin and polidocanol injection and clipping. EUS was performed to confirm vessel obliteration but still identified a large caliber (2.5 mm) feeding vessel arising from the splenic artery penetrating the gastric muscularis propria (Fig. 1). Selective splenic artery angiogram as determined by EUS was performed, revealing a short gastric artery ectasia and hypervascularization (Fig. 2, large arrow) ending in the previously endoscopically placed clips (Fig. 2, small arrow). Superselective transcatheter arterial embolization (TAE) was performed, and the patient presented no further episodes of gastrointestinal bleeding at the 1-year follow-up.
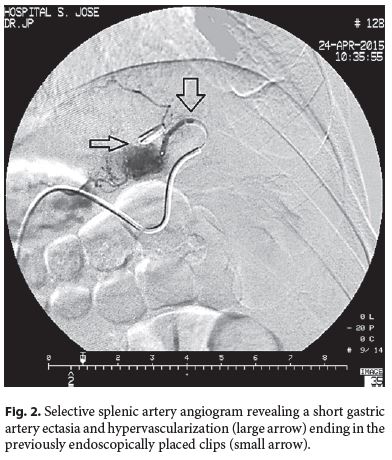
Dieulafoys lesion is a relatively rare cause of upper gastrointestinal bleeding which may be difficult to detect on endoscopy in the case of nonactive bleeding [1]. EUS may be used to identify a nonactively bleeding Dieulafoys lesion, to perform EUS-guided therapy, and to monitor therapy effectiveness [1, 2]. In fact, it is our practice to perform EUS after inconclusive UGE in a severe upper gastrointestinal bleeding setting, clinically suggestive of Dieulafoys lesion origin, and we also systematically perform EUS after endoscopic therapy to confirm effective vessel obliteration [3]. When refractory to endoscopic treatment, surgery and TAE should be considered [1]. Marking the lesion with a metallic clip has accurately guided the endovascular intervention in cases of nonactive bleeding ulcer and may be equally useful in the treatment of Dieulafoys lesions [4]. With this case, we emphasize the role of EUS as a roadmap for other interventions, such as selective TAE.
References
1 Nojkov B, Cappell MS: Gastrointestinal bleeding from Dieulafoys lesion: clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc 2015;7:295–307. [ Links ]
2 Law R, Fujii-Lau L, Wong Kee Song LM, Gostout CJ, Kamath PS, Abu Dayyeh BK, et al: Efficacy of endoscopic ultrasound-guided hemostatic interventions for resistant nonvariceal bleeding. Clin Gastroenterol Hepatol 2015;13:808–812. [ Links ]
3 Pinto-Marques P, Gíria J, Brito M, Camacho R, Loureiro R: Unusual cause for upper GI bleeding: a splenic artery aneurysm mimicking a Dieulafoy lesion. Role for systematic EUS assessment? Gastrointest Endosc 2010;71:845–846. [ Links ]
4 Eriksson LG, Sundbom M, Gustavsson S, Nyman R: Endoscopic marking with a metallic clip facilitates transcatheter arterial embolization in upper peptic ulcer bleeding. J Vasc Interv Radiol 2006;17: 959–964. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Rita Barosa
Department of Gastroenterology, Hospital Garcia de Orta
Avenida Torrado da Silva
PT–2801-951 Almada (Portugal)
E-Mail a.rita.b@gmail.com
Received: July 22, 2016; Accepted after revision: September 16, 2016














