Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.2 Lisboa abr. 2017
https://doi.org/10.1159/000450875
ORIGINAL ARTICLE
Health-Related Quality of Life in Portuguese Patients with Chronic Hepatitis C
Qualidade de Vida Relacionada com a Saúde em Doentes Portugueses com Hepatite C Crónica
Andreia Reia, Marta Rochab, Isabel Pedrotoa, b
aInstituto de Ciências Biomédicas Abel Salazar (ICBAS), Medical College, University of Porto (UP), and bGastroenterology Department, Hospital de Santo António (HSA), Centro Hospitalar do Porto (CHP), Porto, Portugal
* Corresponding author.
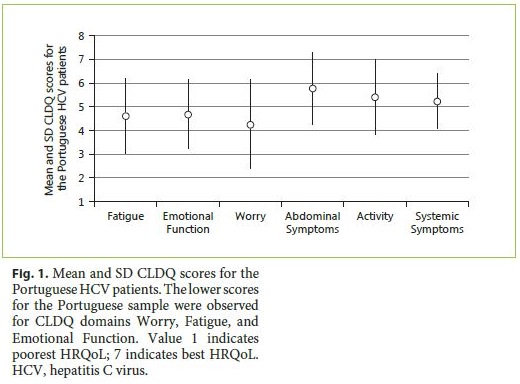
ABSTRACT
Introduction: Chronic hepatitis C virus (HCV) infection impacts multiple health and psychosocial dimensions and encompasses a significant overall burden as it progresses to advanced stages of hepatic disease. Aims: To evaluate for the first time health-related quality of life (HRQoL) of a subset of Portuguese adult patients with chronic hepatitis C using the Portuguese versions of generic, Short-Form 12 Health Survey (SF-12v2), and disease-specific, Chronic Liver Disease Questionnaire (CLDQ), instruments; to assess psychometric properties of CLDQ, Portuguese version. Methods: HRQoL was evaluated in Portuguese adult outpatients with chronic hepatitis C attending the Hepatology Clinic at Centro Hospitalar do Porto, using SF-12v2 and CLDQ. This transversal study was conducted between April and October 2015. Results: Eighty outpatients with chronic hepatitis C were enrolled, with mean age 57 years (standard deviation 11), 67.5% male, all Caucasian, 76.3% diagnosed for >10 years, 66.3% with C virus genotype 1, 65.0% with hepatic cirrhosis (94.2% of which Child-Pugh A), and 46.3% under current antiviral treatment. For CLDQ internal consistency, Cronbachs α was 0.88; for construct validity, correlations ranged from 0.36 to 0.80 ( p < 0.01). Mean CLDQ scores ranged from 4.25 (Worry) to 5.78 (Abdominal Symptoms). Lower scores were observed for Worry, Fatigue, and Emotional Function domains. Statistically significant differences were found in median values of Worry (CLDQ) and Role Emotional (SF-12) ( p < 0.05) for current antiviral treatment, with higher scores for patients that concluded therapy. Conclusion: HRQoL was negatively affected in several domains in Portuguese patients with chronic hepatitis C; oral antiviral treatment correlated with better quality of life, assuring its benefits on this population; the CLDQ Portuguese version revealed adequate psychometric properties, and was useful in assessing quality of life in Portuguese HCV patients.
Keywords: Health surveys; Hepatitis C, chronic; Portugal; Psychometrics; Quality of life
RESUMO
Introdução: A infeção crónica por vírus da hepatite C (VHC) afeta múltiplas dimensões da saúde física e psicossocial e tem um impacto global significativo à medida que progride para estadios mais avançados de doença hepática crónica. Objetivos: Avaliar, pela primeira vez, a qualidade de vida relacionada com a saúde (QdVS) em uma amostra de doentes portugueses, adultos, com hepatite C crónica, usando as versões Portuguesas de um instrumento genérico, Short-Form 12 Health Survey (SF-12v2), e de um instrumento específico da doença, Chronic Liver Disease Questionnaire (CLDQ); estudar as propriedades psicométricas da versão portuguesa do CLDQ. Métodos: Foi avaliada a QdVS de doentes adultos com hepatite C crónica seguidos em consulta de Hepatologia no Centro Hospitalar do Porto, recorrendo às versões portuguesas dos instrumentos de qualidade de vida, SF-12v2 e CLDQ. Este estudo transversal decorreu entre Abril e Outubro de 2015. Resultados: Foram avaliados 80 doentes, 67.5% do sexo masculino, idade média 57 ± 11 anos, 76.3% com infeção diagnosticada há mais de 10 anos, 66.3% Genótipo 1 VHC, 65.0% com cirrose hepática (94.2% destes Child-Pugh A), 46.3% sob terapêutica antiviral oral atual e 12.5% com terapêutica já concluída. Como consistência interna obteve-se um α-Cronbach de 0.88; as correlações de validade de constructo variaram entre 0.36– 0.80 ( p < 0.01). Os scores médios de qualidade de vida do CLDQ variaram entre 4.25 (Preocupação) e 5.78 (Sintomas abdominais). Obtiveram-se resultados inferiores nos domínios Preocupação, Fadiga e Função emocional. Na variável terapêutica antiviral oral verificaram-se diferenças significativas nos valores medianos dos domínios Preocupação/ CLDQ e Desempenho emocional/SF-12 ( p < 0.05), com valores mais elevados para o subgrupo com terapêutica antiviral já concluída. Conclusão: A QdVS revelou ser negativamente influenciada nos doentes portugueses com hepatite C crónica; o tratamento antiviral oral associou-se a melhor qualidade de vida, reafirmando os seus benefícios nesta população; a versão portuguesa do CLDQ revelou propriedades psicométricas adequadas, sendo útil na avaliação da qualidade de vida em doentes portugueses com hepatite C crónica.
Palavras-Chave: Hepatite C Crónica; Portugal; Psicometria; Qualidade de Vida; Questionários de Saúde
Introduction
Hepatitis C virus (HCV) chronic infection constitutes a serious, well-recognized global public health issue, mainly due to the high rate of progression to advanced chronic liver disease (CLD) with significant morbidity and mortality. It impacts a range of dimensions that go far beyond each patients physical and psychosocial health and clinical management, extending to community and health policy settings [1].
The true prevalence of hepatitis C in Portugal is unknown, although in clinical practice hepatitis C is increasing, being the most reported among viral hepatitis infections. An incidence of at least 1: 100,000 HCV infections and a prevalence between 1 and 1.5% are estimated in Portugal, yet with a diagnostic rate of 30% [1]. The burden of the disease is appreciable, with Portugal being one of the European countries with higher rates of disability- adjusted life years (DALYs) associated with HCV(152.2 DALYs/100,000 persons). Also the financial impact has been substantial and predominantly associated with complications of advanced hepatic disease [1]. Bearing epidemiological data on HCV infection, an increase is expectable in the reported chronicity, associated complications, and overall burden of disease in forthcomingyears [1].
Assessment of health-related quality of life (HRQoL) has become a frequent and valuable outcome measure in clinical research with patients facing chronic diseases, including CLD [2–5]. This multidimensional concept refersto a patients subjective and dynamic assessment and perception of his/her own state of health. It integrates physical, mental and social health-related contexts [6]. It can influence therapeutic management and encourage patients to engage in the decision-making process [4–7].
The progression of HCV infection to more advanced stages of hepatocellular dysfunction has proved to negatively affect HRQoL, but this impact can be appreciable at any stage of severity [5, 8–10]. The assessment of HRQoL in HCV patients might help to better understand the burden of extrahepatic manifestations and treatment outcomes,and thus provide improved support to these patients [6].
The assessment of HRQoL comprises the use of generic or specific instruments. The generic, like the Short-Form 36 Health Survey (SF-36) and Short-Form 12 Health Survey (SF-12), are universally applied across different diseases and populations, allowing for comparisons [6, 11]. The specific measures are more comprehensive and focus on possible changes occurring in the course of disease [6, 11]. A particular specific instrument is the Chronic Liver Disease Questionnaire (CLDQ), developed by Younossi et al. [8]. It is useful in all etiologies of liver disease at any severity stage [2, 3] and appears to provide a valuable measure of HRQoL in CLD across different cultures [2, 3, 12–15].
Combining both generic and disease-specific instruments can provide additional evidence on HRQoL and thus a more comprehensive clinical approach [2, 3]. The HRQoL of Portuguese patients with chronic HCV is largely unknown, although it is central to clinical management, promoting a more active enrollment and therapeutic compliance [4, 5].
The aims of this study were to evaluate HRQoL in a subset of Portuguese adult patients with chronic HCV using the Portuguese versions of a generic (SF-12) and a disease-specific (CLDQ) instrument, and to assess the psychometric properties of the CLDQ Portuguese version.
Materials and Methods
Patients and Study Design
This study was conducted at the Hepatology Clinic, Hospital de Santo Antonio (HSA), Centro Hospitalar do Porto (CHP), Porto, Portugal, between April and October 2015. It is a descriptive, clinical and epidemiological, observational transversal study. It was aimed at the population of adult outpatients with chronic HCV attending Hepatology Clinic at this referral center. Eligible patients were consecutive outpatients aged ≥ 18 years old with the diagnosis of chronic HCV. Exclusion criteria were: co-infection with other hepatitis viruses or/and human immunodeficiency viruses; coexistence of other forms of hepatic disease (namely alcoholic, autoimmune, or genetic/metabolic); a recent episode of decompensation of the liver disease (ascites, variceal hemorrhage, hepatic encephalopathy, or spontaneous bacterial peritonitis in the previous 6 months); extremely low literacy level or cognitive status precluding reliable participation.
Patients were asked to complete 3 self-administered questionnaires during a regular outpatient visit, with an estimated response time of 10–20 min. A trained interviewer was available to assist patients as needed and to confirm full completion of questionnaires. All patients received oral and written explanation of the study and signed an informed consent form to participate after full clarification of the studys aims and requirements. Privacy was respected, and every patient was assured about the confidentiality of data. The study was reviewed and approved by the Hospital EthicalCommittee, Research Coordinator Office, and authorized by the CHP Administration Board.
Instrument Measures
The following self-administered instruments were used: a sociodemographic and clinical data questionnaire and Portuguese versions of the SF-12 (generic) and CLDQ (disease specific) HRQoL questionnaires. The sociodemographic and clinical data are described in the next section. Some specifications of the HRQoL measures are presented in Table 1 .
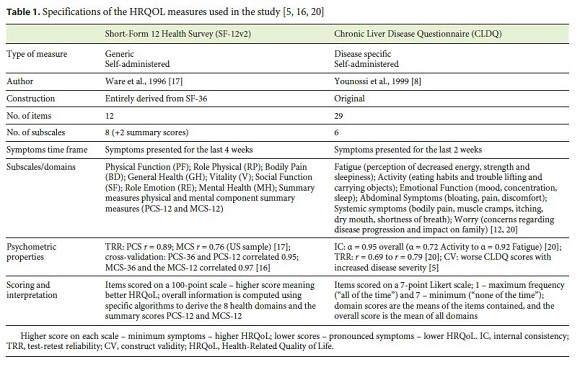
The CLDQ is applicable to all etiologies and severity stages of CLD. CLDQ was translated and validated in several languages, and has been reported as a useful measure of HRQoL in clinical trials across different cultures [2, 3, 8].
A written license agreement to use the certified Portuguese (Portugal) version of CLDQ was obtained by the first author from Dr. Zobair Younossi in December 2014. The translation and linguistic validation process of CLDQ into the Portuguese (Portugal) language was previously undertaken in 2008 by PharmaQuest ® Ltd., following accurate methodology. As far as we are concerned, the CLDQ has not yet been validated in a Portuguese population. Although this study aimed to report some CLDQ psychometric properties, the validation of this measure in Portuguese HCV patients is beyond its scope.
The SF-12 Health Survey was developed as a shorter alternative to the original SF-36, when the latter is considered too long and imposes a great burden on respondents. The SF-12 retains the comprehensiveness of the content and psychometric efficiency, particularly in large-scale studies focused on physical and mental health assessments [16, 17].
The SF-36 Health Survey is a reliable and valid measure for assessing domains of health status. It was considered by some authors as the most appropriate generic HRQoL instrument for use in hepatology due to its psychometric properties [13]. SF-36 was validated in the Portuguese language by Ferreira [7, 18]. The SF-12 is entirely a subset of the SF-36, covering the same 8 domains of health and correlating well with SF-36 summary scores, thus providing good reproduction of these [16].
In our study, a trial with SF-36 was completed with the first 10 eligible HCV patients. There was a lack of compliance due to the length of the questionnaire and associated fatigue. As we could not obtain valid responses, after this trial we adopted the shorter form SF-12, which improved compliance.
The remaining clinical data were assessed from medical records, including: HCV genotype, severity of disease (cirrhosis and Child-Pugh score), indirect assessment of hepatic fibrosis (Fibroscan ® ); current antiviral therapy, type and duration; comorbidities.
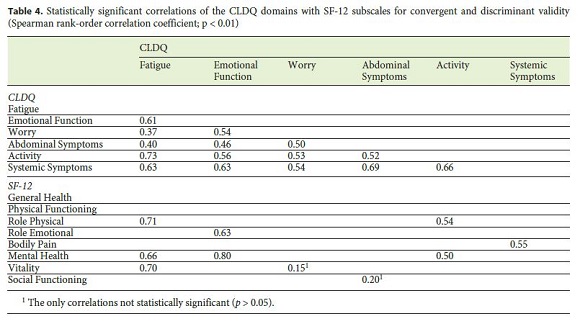
CLDQ Portuguese Version: Psychometric Properties
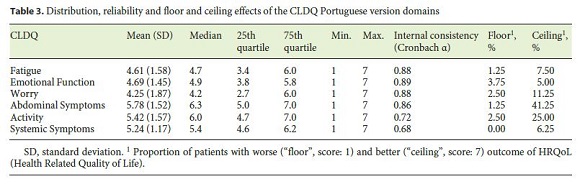
The following psychometric properties of the CLDQ Portuguese version were assessed: internal consistency, construct validity (convergent and discriminant), and floor or ceiling effects. Internal consistency refers to the extent to which items in a domain are correlated, thus measuring the same concept. According to Terwee et al. [19] a Cronbachs α between 0.70 and 0.95 is considered an adequate measure of internal consistency. Convergent validity measures the extent to which domains in an instrument correlate with others that assess a similar concept, according to derived hypotheses [19]. In accordance with previous work correlating CLDQ with SF-12 domains [12, 20], we hypothesized high correlations ( r > 0.70) between: Fatigue (CLDQ) and Vitality (SF-12); Activity (CLDQ) and Physical Functioning (SF-12); Emotional Function (CLDQ) and Mental Health (SF-12) [12, 20]. Discriminant validity refers to the extent to which a measure does not correlate too strongly with measures intended to assess different traits. We hypothesized low correlations ( r < 0.50) between the domains: Abdominal symptoms (CLDQ) and Role emotional (SF-12); Worry (CLDQ), with Physical Functioning, Role Physical and Bodily pain (SF-12) [12, 20].
If more than 15% of patients achieved the lowest or the highest possible score on CLDQ domains, floor and ceiling effects, respectively, were considered to be present. They suggest missing items at the lower or upper end of the domain and thus limited content validity [19].
For a qualitative analysis, we aimed to gather the patients perception regarding easiness and relevance of the CLDQ Portuguese version. Patients were asked about overall opinion and whether any item was difficult to understand.
HRQoL Assessment
Mean and standard deviation (SD) CLDQ scores were calculated.
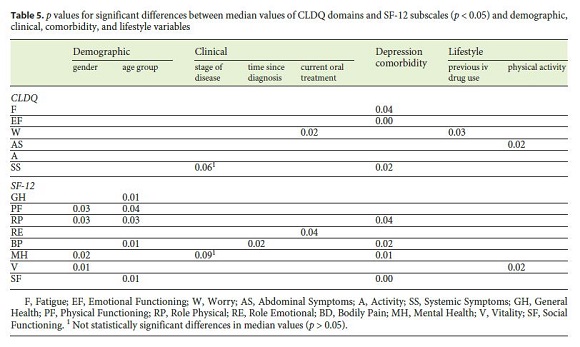
Several variables were analyzed for significant differences in median values of CLDQ and SF-12 domains (using the nonparametric tests Mann Whitney U and Kruskal-Wallis; p < 0.05), namely: gender, age group, stage of disease, time since diagnosis, current antiviral oral treatment, comorbidities (depression) and lifestyle variables (previous intravenous drug use; physical activity). Some of the hypotheses we derived were supported by previous studies: (a) male patients were expected to present better HRQoL scores, especially in the domains related to emotional traits and physical dimensions [6, 12, 21] ; (b) younger patients were expected to present better HRQoL scores, and patients with longer time since diagnosis were expected to have lower HRQoL scores, especially on items related to physical symptoms and activity levels [1, 12, 22] ; (c) no significant differences were expected regarding stage of disease, as 94% of the patients with cirrhosis had compensated disease (Child-Pugh A) [8, 13, 23] ; (d) patients with concluded antiviral treatment were expected to have higher HRQoL scores [24, 25] ; (e) patients with depression were expected to have lower HRQoL scores, mainly on emotional traits [4] ; (f) patients with previous intravenous drug use were expected to have lower HRQoL scores due to prevailing stigma [6, 26] ; (g) patients practicing exercise were expected to present higher HRQoL scores on physical domains [27, 28].
Statistical Analysis
Data were analyzed using Microsoft Office Excel 2013 and the IBM ® Statistical Package for Social Sciences for Windows-SPSS ® version 22.0. Distributions of continuous variables were analyzed, and Kolmogorov-Smirnov tests were performed to assess their deviation from a normal distribution. Quantitative variables were summarized as mean and SD, or as median and 25th and 75th quartiles for variables exhibiting skewed distributions. Such variables were compared using nonparametric tests. In order to allow for comparisons with other studies, some continuous variables were presented as mean and SD. The level of significance was set at p < 0.05 or p < 0.01.
Results
A total of 80 patients with chronic HCV were enrolled in the study, with a mean age of 57 years (SD 11), 67.5% of which were male, all Caucasian, 76.3% with HCV diagnosed for longer than 10 years, 66.3% with HCV genotype 1, 65.0% with hepatic cirrhosis (94.2% of which Child-Pugh A), 46.3% under current antiviral treatment, and 12.5% with concluded treatment; 32.5% of patients had a history of past intravenous drug use and 25.0% had depressive syndrome. The detailed sociodemographic, clinical, and lifestyle characteristics of the sample are presented in Table 2 . Most patients readily self-completed the questionnaires, but 14 patients required some assistance mainly due to uncorrected visual impairment.
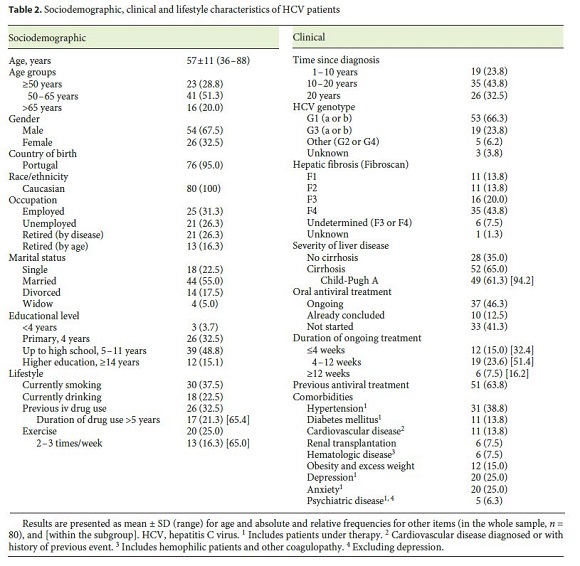
Regarding the assessment of CLDQs psychometric properties, data on the internal consistency of the CLDQ scales are presented in Table 3 . Mean Cronbachs α was 0.88, ranging from 0.68 to 0.89. For construct validity, some of the correlations between the CLDQ and SF-12 domains are presented in Table 4 . For convergent validity, correlations were all statistically significant, ranging from 0.36 to 0.80 ( p < 0.01), except those between Worry (CLDQ) and Vitality (SF-12) and between Abdominal Symptoms (CLDQ) and Social Functioning (SF-12). The highest correlations were found between: Emotional Function (CLDQ) and Mental Health (SF-12) ( r = 0.80, p < 0.01); Fatigue (CLDQ) and Role Physical (SF-12) ( r = 0.71, p < 0.01); Fatigue (CLDQ) and Vitality (SF-12) ( r = 0.70, p < 0.01). For discriminant validity, correlations between scales hypothesized as less-comparable ranged between 0.25 and 0.42. These lowest correlations were found between: Worry (CLDQ) and Physical Functioning (SF-12) ( r = 0.25, p < 0.05); Worry (CLDQ) and Role Physical (SF-12) ( r = 0.26, p < 0.05); Abdominal Symptoms (CLDQ) and Role Emotional (SF-12) ( r = 0.35, p < 0.01). The proportion of floor effects (presented in Table 3) was low and below the 15% criteria on every CLDQ domain. The proportion of ceiling effects was overall low, except for Abdominal Symptoms and Activity CLDQ domains (41.3 and 25.0%, respectively).
Considering HRQoL, mean CLDQ scores for Portuguese HCV patients are presented in Figure 1 . Mean scores ranged from 4.25 (Worry) to 5.78 (Abdominal Symptoms). The lower CLDQ scores pertain to Worry, Fatigue, and Emotional Function domains. The highest CLDQ scores refer to Abdominal Symptoms and Activity domains. In the analysis of HRQoL, where statistically significant differences in the median values of CLDQ domains were considered (Table 5), significant differences were not found in gender, age group, stage of disease, and time since diagnosis (all p > 0.05). In contrast, significant differences by gender were found in the median values of Physical Functioning, Role Physical, Mental Health, and Vitality (SF-12), with highest values (meaning better HRQoL) in males ( p < 0.05). Statistically significant differences by age group were also found in median values of General Health, Physical Functioning, Role Physical, Bodily pain and Social Functioning (SF-12), with highest values (better HRQoL) in age group ≤ 50 years. For time since diagnosis, significant differences were found in the median values of Bodily Pain (SF-12), with significantly lower value (indicating worse HRQoL) for the subgroup with >20 years since diagnosis (p < 0.05). For stage of disease, statistically significant differences were not found in the median values of neither domain, although there was a tendency towards significant differences in Systemic Symptoms (CLDQ) and Mental Health (SF-12). In current antiviral oral treatment, statistically significant differences were found in median values both for Worry (CLDQ) and Role Emotional (SF-12), with significantly higher values (indicating better HRQoL) for the subgroup that already concluded therapy. Significant differences were still found for Worry (CLDQ) when comparing patients admitted to treatment (ongoing or already concluded) with those without treatment, with higher HRQoL scores for the former. For depression, statistically significant differences were found in the median values of Emotional Functioning, Systemic Symptoms, and Fatigue (CLDQ) and Mental Health, Bodily Pain, Role Physical and Social Functioning (SF-12), with significant lower values (indicating worse HRQoL) for the subgroup with depression. For previous intravenous drugs use, statistically significant differences were found in median values of Worry (CLDQ), with significant lower scores for patients with past intravenous drug use. For physical activity, significant differences were observed in the median values of Abdominal Symptoms (CLDQ) and Vitality (SF-12), with significant higher scores for patients engaging physical activity.
Most patients found the CLDQ easy to understand and relevant. Two patients referred the relevance of an item covering apathy (meaning lack of concern/interest). The last item, regarding concern about availability of a liver transplant if needed, was described as overstated by some patients.
Discussion and Conclusions
Chronic HCV infection remains a global health concern, with multiple and significant impact associated with disease progression [1, 4]. In Portugal, the overall burden of HCV is appreciable and is expected to rise in forthcoming years [1]. Assessment of HRQOL combining general and disease-specific instruments is lacking in Portuguese HCV patients, thus being the main goal of this study.
The assessed CLDQs psychometric properties were overall adequate. Namely, for internal consistency, mean Cronbachs α fitted the defined criteria [19], which was consistent with reports from the original CLDQ [8, 20] and European CLDQ validation studies [12, 13]. Retest reliability was not assessed, which should be regarded as a limitation of this study.
Most of the hypothesized correlations for convergent and discriminant validity [20] were confirmed. As predicted, we found high correlations ( r > 0.70) between CLDQ and SF-12 domains assumed to measure a similar concept. The Activity (CLDQ) and Physical Functioning (SF-12) domains were only moderately correlated, but we found instead high correlation with Role Physical (SF-12). As all of these domains reasonably assess limited accomplishments in activities [17], they are strongly correlated. For discriminant validity, as predicted [20] we found low correlations ( r < 0.50) between: Worry (CLDQ) and Physical Functioning (SF-12); Worry (CLDQ) and Role Physical (SF-12). These expectedly assess different traits: Physical Functioning and Role Physical explored levels of difficulty and limitations in physical activities or diminished activity accomplishments, respectively. In contrast, Worry involved concerns about developing more severe and progressive symptoms and the impact on family [17, 20]. We also found lower correlations in Abdominal Symptoms (CLDQ) and Role Emotional (SF-12) domains, as the former assessed presence of abdominal bloating, discomfort or pain, and the latter involved interference of emotional issues [17, 20].
The presence of moderate to low correlations between some CLDQ and SF-12 domains is valuable and suggests that CLDQ provided additional relevant HRQoL information concerning HCV patients not covered by generic instruments such as SF-12 [12, 13].
The percentages of floor and ceiling effects in CLDQ domains were reasonably adequate [19]. The ceiling effect on the Activity domain was also found in a previous study [12], suggesting that extreme items (regarding better symptoms) might be missing to better discriminate patients.
Considering HRQoL assessed by CLDQ, our sample of Portuguese HCV patients revealed lower levels of HRQoL in the Fatigue, Worry, and Emotional Function domains. As fatigue represents one of the most frequent and disabling features in CLD and HCV [29, 30], low levels were point fatigue as an independent predictor of low HRQoL [4]. Disease-related worries have been claimed as having an impact on HRQoL of HCV patients [31]. Also, the strong perceived stigma associated with this infection can affect self-esteem, social functioning and raise uncertainty and increased concerns about the future and disease progression [32, 33]. These might explain the low HRQoL levels in CLDQ Worry domain. The outcome on Emotional Function might be related to the presence of diagnosed depression and anxiety (in 25.0% of the patients each). The significant overlap of depressive or anxiety syndromes in this population is widely reported [4, 29, 34]. Depression was documented in 28.0% of HCV-naive patients [34], and anxiety in 24.0% of HCV patients [4], which closely resembled the proportion found in our sample. Depression in these patients is associated with higher levels of subjective physical symptoms, higher stigma, and lower coping strategies [34], and thus with lower HRQoL [4, 35]. As expected, significant worse HRQoL was found for depressed patients on Emotional Functioning, Systemic Symptoms, and Fatigue (CLDQ) and in several SF-12 subscales.
In contrast, better HRQoL scores were found in Abdominal Symptoms and Activity domains, which could relate to sample characteristics. Thirty-five percent of patients did not have cirrhosis, and considering the cirrhotic patients, 94.2% had compensated disease. Following the natural history of CLD, patients may remain mild symptomatic for a long course or have unspecific complaints [6, 22]. Eventually compensated patients could report less abdominal symptoms and higher activity indices, compared with patients with decompensated disease. From the variables compared for statistically significant differences regarding CLDQ and SF-12 domains, most of the hypotheses were corroborated. Better HRQoL was found for male gender in some SF-12 subscales, like in some previous studies [6, 12]. In accordance, a Portuguese study on the definition of SF-36 Portuguese norms [21] concluded that the female gender independently correlated significantly with lower (meaning worse) self-perception of health state.
The outcome of better HRQoL in the younger age group ( ≤ 50 years) and with less time since diagnosis could be explained by the CLD natural history; these groups were expected to be less symptomatic, to have fewer complications and a better HRQoL. Patients with longer diagnosis are more prone to more advanced and symptomatic disease (thus the significant difference in Bodily Pain subscale scores) [1, 22]
As expected, we found no significant differences in the median values of CLDQ or SF-12 domains regarding stage of disease. This outcome is consistent with other studies [12, 13], where significant differences were only found when comparing patients with more advanced liver disease (Child-Pugh B and C). In our study, 35.0% of patients did not have cirrhosis, and from those who developed cirrhosis, 94.2% had compensated disease (Child-Pugh A).
Considering the variable current antiviral oral treatment, significantly better HRQoL was found on Worry (CLDQ) and Role Emotional (SF-12) in patients that already concluded antiviral treatment. This suggests that this subgroup became less concerned about the severity of symptoms and disease progression, probably due to the reduced symptoms and the confidence geared by an effective treatment. In this subgroup 6 patients were female, 6 were aged 50–65 years, all but 1 with <20 years since diagnosis and none with previous EV drug use. Six patients had cirrhosis and 8 concluded 24 weeks of therapy. This is a particularly relevant outcome, as it shows that oral antiviral treatment can be correlated with HRQoL increases, particularly on domains among those who scored lower for our Portuguese patients. Recent studies on the impact of treatment with direct antiviral agents corroborate this evidence [24, 25, 36].
Previous drug use is associated with higher stigma, and thus the levels of HRQoL can decrease, especially on domains relating to concerns for disease and for the future [32, 33] ; physical activity has been claimed to increase the scores in HRQoL physical domains and thus is recommended [27, 28].
The Portuguese CLDQ version demonstrated good acceptability and ease of administration. The adequacy of the last item was already discussed in a study with HCV patients [14], where it was omitted for not reflecting a predominant concern for this population. However, as the CLDQ integrates all severity CLD stages, it should include concern about treatment for end-stage disease, even though it lacks sensitivity for compensated disease.
The relevance of this study should be emphasized, as it aimed to characterize HRQoL in Portuguese HCV patients and surpass the limited knowledge regarding health perception in this population. Combining generic and disease-specific instruments was intended to provide a more accurate assessment, and the presence of moderate to low correlations between some CLDQ and SF-12 domains emphasized such complementarity. The CLDQ is becoming an increasingly useful instrument in this setting, confirmed by its widespread use across different cultures and properly validated versions. As the CLQD was not yet validated in Portuguese, this study also aimed to build knowledge on some psychometric properties of the Portuguese version.
Some limitations of this study should also be noted. Regarding methodology, adopting SF-12 might have compromised psychometric efficiency, particularly in the absence of a large-scale study with focus on physical and mental health summary scores. However, for our purpose, it was more useful to derive the 8 health SF-36 subscales to gather more detailed clinical data for meaningful comparisons. Another limitation pertained to the presentation of continuous data from skewed distributions as mean and SD to allow for comparisons with similar studies. The tradeoff is that cautious assumptions should be drawn from these comparisons. Considering sample characteristics, it would be better to have a larger sample size and more balanced subgroups with an equivalent size, namely for gender, stage of disease, and current treatment variables. Our sample mainly included patients without cirrhosis or with compensated disease, which precluded analysis regarding the impact of more severe disease on HRQoL. Following previous studies, we focused on demographic and clinical variables that could relate to and explain differences in HRQoL in this population. Bearing the effect of treatment on HRQoL, it would have been preferable to apply the questionnaires to the same patients before, during, and after oral antiviral therapy, to enable paired tests. Perhaps the most clear-cut limitation is the inability to objectively compare HRQoL scores due to the absence of standardized norms. It precludes a more objective definition of acceptable HRQoL scores and extent of HRQoL deviations for this population. Further studies are clearly needed to better understand the impact of HCV on HRQoL, to validate the CLDQ Portuguese version and to build standardized norms for the Portuguese population.
Finally, we can conclude that HRQoL, as assessed by CLDQ and SF-12, was negatively affected in several domains in Portuguese HCV patients, in line with previous findings. Some particular outcomes stand out from our study. The fact that oral antiviral treatment could be correlated with HRQoL increases in some domains provides growing evidence for the multiple benefits of appropriately treating these patients. Due to the high prevalence and negative impact of mood disorders (namely depression) on HRQoL, it might be valuable to screen and provide suitable psychosocial interventions in a multidisciplinary setting. The CLDQ Portuguese version revealed adequate psychometric properties and good acceptability, being a useful instrument to assess HRQoL in Portuguese HCV patients.
References
1 Anjo J, Cafe A, Carvalho A, Doroana M, Fraga J, Giria J, et al: O impacto da hepatite C em Portugal. GE J Port Gastrenterol 2014;21:44–54. [ Links ]
2 Martin LM, Younossi ZM: Health-related quality of life (HRQL) in chronic liver disease. Dig Liver Dis 2005;37:819–820. [ Links ]
3 Martin LM, Dan AA, Younossi ZM: Measurement of health-related quality of life in patients with chronic liver disease. Liver Transpl 2006;12:22–23. [ Links ]
4 Younossi Z, Kallman J, Kincaid J: The effects of HCV infection and management on healthrelated quality of life. Hepatology 2007;45:806–816. [ Links ]
5 Gutteling JJ, de Man RA, Busschbach JJ, Darlington AS: Overview of research on healthrelated quality of life in patients with chronic liver disease. Neth J Med 2007;65:227–234. [ Links ]
6 Strauss E, Dias Teixeira MC: Quality of life in hepatitis C. Liver Int 2006;26:755–765. [ Links ]
7 Ferreira PL: Development of the Portuguese version of MOS SF-36. I. Cultural and linguistic adaptation. Acta Med Port 2000;13:55–66. [ Links ]
8 Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D: Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut 1999;45:295–300. [ Links ]
9 Spiegel BM, Younossi ZM, Hays RD, Revicki D, Robbins S, Kanwal F: Impact of hepatitis C on health related quality of life: a systematic review and quantitative assessment. Hepatology 2005; 41: 790–800. [ Links ]
10 Younossi ZM, Boparai N, Price LL, Kiwi ML, McCormick M, Guyatt G: Health-related quality of life in chronic liver disease: the impact of type and severity of disease. Am J Gastroenterol 2001;96:2199–2205. [ Links ]
11 Foster GR: Quality of life considerations for patients with chronic hepatitis C. J Viral Hepat 2009;16:605–611. [ Links ]
12 Ferrer M, Cordoba J, Garin O, Olive G, Flavia M, Vargas V, et al: Validity of the Spanish version of the Chronic Liver Disease Questionnaire (CLDQ) as a standard outcome for quality of life assessment. Liver Transpl 2006;12:95–104. [ Links ]
13 Hauser W, Schnur M, Steder-Neukamm U, Muthny FA, Grandt D: Validation of the German version of the Chronic Liver Disease Questionnaire. Eur J Gastroenterol Hepatol 2004;16:599–606. [ Links ]
14 Rucci P, Taliani G, Cirrincione L, Alberti A, Bartolozzi D, Caporaso N, et al: Validity and reliability of the Italian version of the Chronic Liver Disease Questionnaire (CLDQ-I) for the assessment of health-related quality of life. Dig Liver Dis 2005;37:850–860. [ Links ]
15 Mucci S, de Albuquerque Citero V, Gonzalez AM, Geocze L, Geocze S, de Jesus Lopes Filho G, et al: Validation of the Brazilian version of Chronic Liver Disease Questionnaire. Qual Life Res 2013;22:167–172. [ Links ]
16 Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al: Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998;51:1171–1178. [ Links ]
17 Ware J Jr, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–233. [ Links ]
18 Ferreira PL: Development of the Portuguese version of MOS SF-36. II. Validation tests. Acta Med Port 2000;13:119–127. [ Links ]
19 Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al: Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34–42. [ Links ]
20 Schulz KH, Kroencke S, Ewers H, Schulz H, Younossi ZM: The factorial structure of the Chronic Liver Disease Questionnaire (CLDQ). Qual Life Res 2008;17:575–584. [ Links ]
21 Ferreira PL, Santana P: Health status perception and quality of life in the working population: towards a definition of normative data. Rev Port Saude Publica 2003;21:12. [ Links ]
22 Jacobson IM, Davis GL, El-Serag H, Negro F, Trepo C: Prevalence and challenges of liver diseases in patients with chronic hepatitis C virus infection. Clin Gastroenterol Hepatol 2010;8:924–933; quiz e117. [ Links ]
23 Bjornsson E, Verbaan H, Oksanen A, Fryden A, Johansson J, Friberg S, et al: Health-related quality of life in patients with different stages of liver disease induced by hepatitis C. Scand J Gastroenterol 2009;44:878–887. [ Links ]
24 Younossi Z, Henry L: Systematic review: patient-reported outcomes in chronic hepatitis C – the impact of liver disease and new treatment regimens. Aliment Pharmacol Ther 2015;41:497–520. [ Links ]
25 Soriano V, Labarga P, Fernandez-Montero JV, de Mendoza C, Esposito I, Benitez-Gutierrez L, et al: Hepatitis C cure with antiviral therapy – benefits beyond the liver. Antivir Ther 2016;21:1–8. [ Links ]
26 Foster GR, Goldin RD, Thomas HC: Chronic hepatitis C virus infection causes a significant reduction in quality of life in the absence of cirrhosis. Hepatology 1998; 27: 209–212. [ Links ]
27 Painter P, Krasnoff J, Paul SM, Ascher NL: Physical activity and health-related quality of life in liver transplant recipients. Liver Transpl 2001;7:213–219. [ Links ]
28 McKenna O, Blake C: Management of hepatitis C: the potential benefits of exercise. Phys Ther Rev 2007;12:271–276. [ Links ]
29 Jacobson IM, Cacoub P, Dal Maso L, Harrison SA, Younossi ZM: Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol 2010;8:1017–1029. [ Links ]
30 Poynard T, Cacoub P, Ratziu V, Myers RP, Dezailles MH, Mercadier A, et al: Fatigue in patients with chronic hepatitis C. J Viral Hepat 2002;9:295–303. [ Links ]
31 Hauser W, Zimmer C, Schiedermaier P, Grandt D: Biopsychosocial predictors of health-related quality of life in patients with chronic hepatitis C. Psychosom Med 2004;66:954–958. [ Links ]
32 Marinho RT, Barreira DP: Hepatitis C, stigma and cure. World J Gastroenterol 2013;19:6703–6709. [ Links ]
33 Conrad S, Garrett LE, Cooksley WG, Dunne MP, MacDonald GA: Living with chronic hepatitis C means you just havent got a normal life any more. Chronic Illn 2006;2:121–131. [ Links ]
34 Golden J, ODwyer AM, Conroy RM: Depression and anxiety in patients with hepatitis C: prevalence, detection rates and risk factors. Gen Hosp Psychiatry 2005;27:431–438. [ Links ]
35 Dan AA, Martin LM, Crone C, Ong JP, Farmer DW, Wise T, et al: Depression, anemia and health-related quality of life in chronic hepatitis C. J Hepatol 2006;44:491–498. [ Links ]
36 Marinho RT, Vitor S, Velosa J: Benefits of curing hepatitis C infection. J Gastrointestin Liver Dis 2014;23:85–90. [ Links ]
Statement of Ethics
Protection of Human and Animal Subjects
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of Data
The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to Privacy and Informed Consent
The authors have obtained written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Isabel Pedroto
Servico de Gastrenterologia, Hospital de Santo António
Centro Hospitalar do Porto, Largo Prof. Abel Salazar
PT–4099-001 Porto (Portugal)
E-Mail ipedroto@gmail.com
Received: June 26, 2016; Accepted after revision: July 26, 2016
Acknowledgments
The authors would like to express their immense gratitude to Dr. Zobair Younossi and the CLDQ group for giving permission to use the CLDQ Portuguese version in our Portuguese HCV patients. The authors also gratefully acknowledge the help of the following persons: Margarida Lima, MD, PhD, from CHP and ICBAS/UP, for the support with the conceptualization and planning of the project, supervising the study, and writing of the manuscript; Odete Lima from Hepatology Outpatient Clinic, for assisting with questionnaire administration; and Isabel Fonseca from CHP-DEFI for the support with the statistical analysis of data. Also, the authors acknowledge the logistic support of Instituto de Ciências Biomédicas Abel Salazar (ICBAS)/ University of Porto (UP) Medical School.














