Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.6 Lisboa dez. 2016
https://doi.org/10.1016/j.jpge.2016.03.003
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Small Bowel Stricture Mimicking Megacolon in a Patient with Crohn's Disease
Estenose do Intestino Delgado Mimetizando Megacólon num Doente com Doença de Crohn
Samuel Raimundo Fernandes*, Luís Araújo Correia, José Velosa
Gastroenterology and Hepatology Department, Hospital de Santa Maria, Centro Hospitalar Lisboa Norte, Lisbon, Portugal
* Corresponding author.
Keywords: Crohn's Disease/complications. Constriction, Pathologic. Intestine, Small. Megacolon
Palavras-chave: Doença de Crohn/complicações. Constrição Patológica. Intestino Delgado. Megacólon
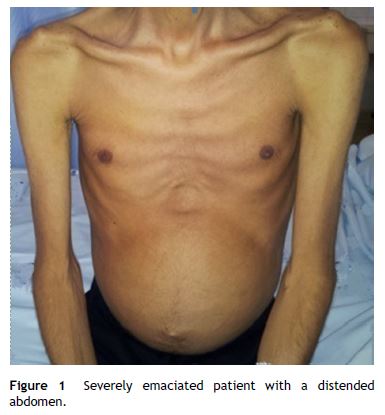
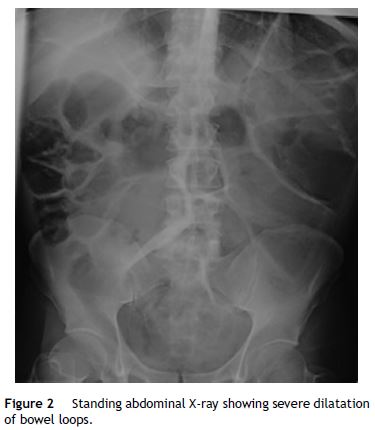
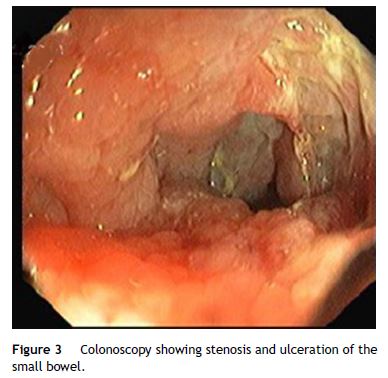
A 38-year-old man with a 20-year history of Crohn's disease presented with weight loss, abdominal distention and vomiting. He had been medicated from diagnosis with 5-aminosalicylic acid and later with azathioprine, which he intentionally stopped 2 years later. His last colonoscopy, dating 5 years before, revealed severe ulceration in the ascending and sigmoid colon. On physical examination the patient was severely emaciated. His abdomen was distended, non-tender, and showed markedly reduced bowel sounds (Fig. 1). His vital signs were normal. Laboratory tests showed mild anemia (12.7 g/dL) and C-reactive protein (22 mg/L), with normal serum electrolytes. Upright abdominal X-ray showed severely distended bowel loops (Fig. 2), later confirmed by abdominal computed tomography. These findings raised our suspicion for the presence of megacolon. As the patient did not presence signs of systemic toxicity we adopted a conservative approach with intravenous steroids, antibiotics, fluid support, daily abdominal X-ray and evaluation by a dedicated surgeon. On the third day of admission, a colonoscopy was performed showing an ulcerated stricture in the terminal ileum that did not allow passage of the endoscope (Fig. 3). The colon showed no signs of active inflammation. Unexpectedly, MRI-enterography showed severe distention (up to 8 cm) of a wide segment of the small bowel proximal to a long stricture. The large bowel appeared not to be significantly distended (Fig. 4). The anatomopathologic examination of the small bowel biopsies showed severe transmural inflammation and architectural distortion compatible with Crohn's Disease. There were also multiple nuclear and cytoplasmic inclusions compatible with cytomegalovirus (CMV) infection. As there was suggestion that the stricture could partially be inflammatory and that the patient might benefit from medical therapy, he was started on ganciclovir and Infliximab. Unfortunately, by the 14th week of therapy there was no significant improvement. Due to progressive weight loss, the patient was scheduled for surgery. Examination of the resection specimen confirmed the long 11 cm stricture with severe distention of both the small bowel (11 cm) and ascending colon (9.5 cm).

Crohn's disease is a chronic progressive inflammatory disease. Over time, up to 25% of patients will develop stricturing disease anywhere in the bowel.1,2 While some strictures might temporarily benefit from medical treatment, most will ultimately require surgery.2,3 This case highlights an uncommon but severe complication of Crohn's disease. Due to the rarity and outstanding radiologic findings, the clinical picture was confused with a megacolon, a severe and potential fatal complication, more commonly seen in patients with severe ulcerative colitis.
References
1. Wolters FL, Russel MG, Sijbrandij J, Ambergen T, Odes S, Riis L, et al. Phenotype diagnosis predicts recurrence rates Crohn's disease. Gut. 2006;55:1124e30. [ Links ]
2. Chang C-W, Wong J-M, Tung C-C, Shih I-L, Wang H-Y, Wei S-C. Intestinal stricture in Crohn's disease. Intest Res. 2015;13:19-26. [ Links ]
3. Parkes M, Jewell DP. Review article: the management of Crohn's disease. Aliment Pharmacol Ther. 2001;15:563-73. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
* Corresponding author.
E-mail address: samuelrmfernandes@gmail.com (S. R. Fernandes).
Received 8 January 2016; accepted 4 March 2016
Authors’ contribution
Samuel Raimundo Fernandes and Luís Araújo Correia elaborated the manuscript. José Velosa reviewed the manuscript.














