Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.6 Lisboa dez. 2016
https://doi.org/10.1016/j.jpge.2016.02.003
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Upper Gastrointestinal Kaposi's Sarcoma in an HIV-Infected Patient
Sarcoma de Kaposi Gástrico em Doente Infetado pelo VIH
Marco Silvaa,*, Tiago Maiab, Guilherme Macedoa
aGastroenterology Department, Centro Hospitalar de São João, Faculty of Medicine of the University of Porto, Porto, Portugal
bPathology Department, Centro Hospitalar de São João, Faculty of Medicine of the University of Porto, Porto, Portugal
* Corresponding author.
Keywords: Gastrointestinal Neoplasms; HIV Infections; Portugal; Sarcoma, Kaposi
Palavras-chave: Neoplasias Gastrointestinais; Infecções por VIH; Portugal; Sacroma de Kaposi
A 32-year-old male was evaluated in the emergency department for worsening asthenia, dizziness, headache and photophobia for the past five days. Physical examination revealed purple and brown lesions in the inner thigh and penis, suggestive of cutaneous Kaposi's sarcoma (KS). His past medical history was remarkable for acquired immunodeficiency syndrome (AIDS) diagnosed five years before with erratic follow-up in outpatient clinic. He was hospitalized three months before due to disseminated cryptococcosis complicated with meningitis, disseminated tuberculosis with intestinal and pulmonary involvement, cytomegalovirus disseminated infection and neurosyphilis. After discharge, he started highly active antiretroviral therapy (HAART), however the patient referred that he was complying with anti-tuberculostatic drugs but he was not taking HAART nor prophylactic antibiotics/antifungals.
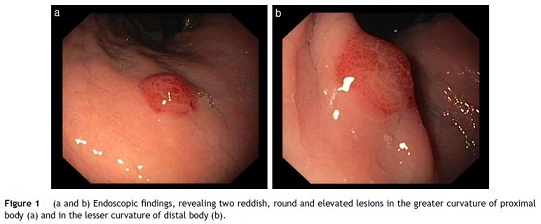
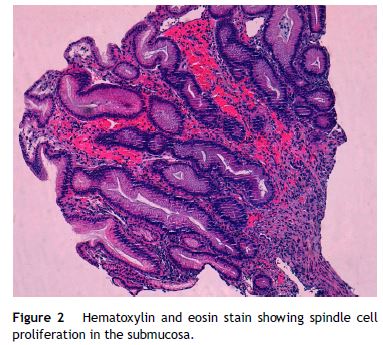
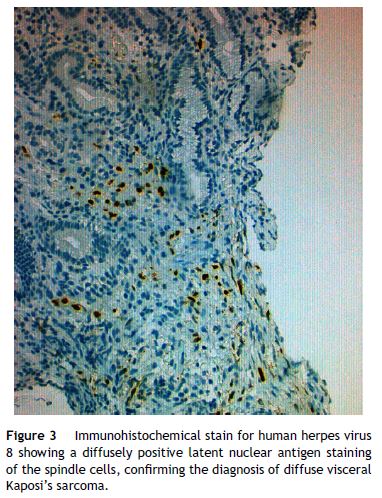
He was admitted for recurrent cryptococcal meningitis and started amphotericin B and flucytosine. To evaluate the extension of KS, an upper endoscopy was performed and revealed two reddish, round and elevated lesions in the body of stomach (Fig. 1), suggestive of KS lesions. The histological exam showed a spindle-cell proliferation in the submucosa (Fig. 2), highlighted with immunochemistry for CD31 and multiple cells positive for human herpesvirus 8 (HHV8), confirming the diagnosis (Fig. 3). The skin lesions size decreased with HAART, precluding the necessity of systemic chemotherapy. After nearly one month of intense therapy for infectious complications, the patient status improved and he was discharged.
KS is a vascular tumor associated with HHV8 infection and, while rare in immunocompetent host, it is the most common neoplasm among HIV-infected patients.1–3
Visceral disease is uncommon and, most commonly, the lung and gastrointestinal (GI) tract are involved.2,3
Most patients with GI involvement are asymptomatic, but may present with non-specific symptoms such as weight loss, diarrhea and abdominal pain.4 In some cases, it may lead to hemorrhage, abdominal pain, gastric outlet obstruction or intussusception.1 GI-KS is endoscopically evident by appearance which ranges from a red maculopapular lesion to a darker, nodular or polypoid lesion.5 In more severe disease, patients may present with a volcanolike mass with a central umbilication or ulceration which can bleed on contact.5
The diagnosis is usually based on the characteristic appearance of cutaneous or mucosal lesions, and confirmatory testing with histopathology and immunohistochemistry.2,5 On histopathology, KS is characterized as spindle cell proliferation that forms irregular vascular channels in the submucosal layer.5 To make a diagnosis of KS, the presence of HHV8 is necessary and immunohistochemical testing is recommended for all specimens with spindle cell morphology.2,5
KS usually responds to HAART, nevertheless, administration of systemic cytotoxic chemotherapy is warranted in patients with advanced, symptomatic or rapidly progressive disease.2,4
Endoscopic evaluation is required in AIDS patients that present with GI symptoms.2 However, in patients that are asymptomatic, the benefit of endoscopy remain a topic of debate. Nevertheless, early endoscopic evaluation allows a proper KS staging and selection of the appropriate therapeutic options, preventing complications associated with progression of the disease.
References
1. Rezende RE, Kahwage RL, da Costa TV, Machado AA, Brunaldi MO, Kemp R, et al. Upper gastrointestinal Kaposi's sarcoma in HIV-infected patients: ten years of endoscopy observation at a single Brazilian center. Int J Infect Dis. 2015;39:110-5. [ Links ]
2. Bower M, Palfreeman A, Alfa-Wali M, Bunker C, Burns F, Churchill D, et al. British HIV Association guidelines for HIV-associated malignancies 2014. J Clin Oncol. 2010;28:250-1. [ Links ]
3. Attia S, Dezube BJ, Torrealba JR, Sosman JM, McHaffie DR, Pfau PR, et al. AIDS-related Kaposi's Sarcoma of the gastrointestinal tract. Am J Transplant. 2013;4:93-106. [ Links ]
4. Rodriguez S, Zapatier J, Allende D, Schneider A. Kaposi's sarcoma an unusual cause of gastric outlet obstruction. ACG Case Rep J. 2013;1:19-21. [ Links ]
5. Lee AJ, Brenner L, Mourad B, Monteiro C, Vega KJ, Munoz JC. Gastrointestinal Kaposi's sarcoma: case report and review of the literature. World J Gastrointest Pharmacol Ther. 2015;6:89-95. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
* Corresponding author.
E-mail address: marcocostasilva87@gmail.com (M. Silva).
Received 8 January 2016; accepted 3 February 2016
Acknowledgments
The authors wish to thank Dr. Margarida Marques and Dr. João Magalhães from the Gastroenterology and Pathology departments, for the support in their work.














