Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.5 Lisboa out. 2016
https://doi.org/10.1016/j.jpge.2015.12.007
ENDOSCOPIC SNAPSHOT
Small Bowel GIST: Clinical Presentation as Intussusception and Obscure Bleeding
GIST do Intestino Delgado: Apresentação Simultânea Sob a Forma de Invaginação e Hemorragia Digestiva Obscura
Sílvia Giestasa, * , Nuno Almeida a, Ruben Martins b, Ana Canhoto b, Pedro Oliveira c, Pedro Figueiredo a, Carlos Sofia a
a Gastroenterology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
b Surgery B Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
c Radiology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
* Corresponding author.
Keywords: Gastrointestinal Hemorrhage. Gastrointestinal Stromal Tumors. Small Intestine. Intussusception.
Palavras-chave: Hemorragia Gastrointestinal. Tumores do Estroma Gastrointestinal. Intestino Delgado. Invaginação.
1. Introduction
Gastrointestinal stromal tumors (GISTs) are rare clinical entities, representing less than 0.2% of all gastrointestinal tumors and only 0.04% of small intestinal malignant neoplasms. GISTs may occur anywhere along gastrointestinal tract, but most commonly arise in the stomach (40–60%) and jejunum/ileum (25–30%).1,2
The clinical presentation of GISTs is highly variable depending on their size, location and presence of mucosal ulceration. Abdominal pain and gastrointestinal bleeding (when mucosal ulceration is present) are the most common symptoms or signs although persistent significant bleeding is unusual. Intussusception and subsequent obstruction is a very uncommon presentation of these lesions because of their tendency to grow in an extraluminal fashion.3,4 Very few cases of small bowel intussusceptions from stromal tumor in adults have been described in medical literature.1–5 Intussusception is rather infrequent in adults, accounting for 0.1% of all surgical admissions and 1–5% of mechanical bowel obstructions. In contrast to childhood, where intussusception is idiopathic in 90% of cases, in adults a definable pathologic lesion is established in over 90% of cases, with neoplasms considered to be the cause in 65% of them. Preoperative diagnosis is often difficult because the symptoms are nonspecific.1–3 Intussusception is correctly diagnosed preoperatively in only one-third of cases.1,3
The relative rarity of GISTs combined with nonspecific presentation results in delayed diagnosis. Frequently, this is only possible after surgery and histological examination.2,3,5
We report an unusual case of jejunojejunal intussusception caused by a GIST which first presentation was a long-standing obscure gastrointestinal bleeding, incorrectly established as determined by a small bowel angyodisplasia after capsule endoscopy examination.
2. Case description
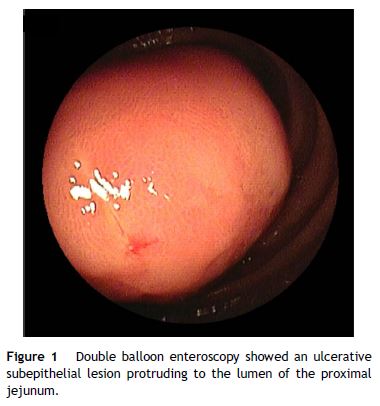
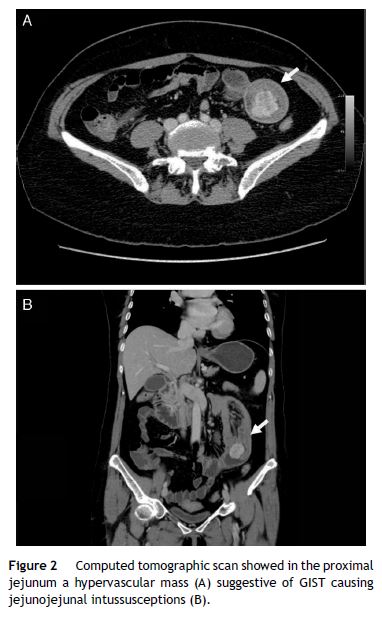
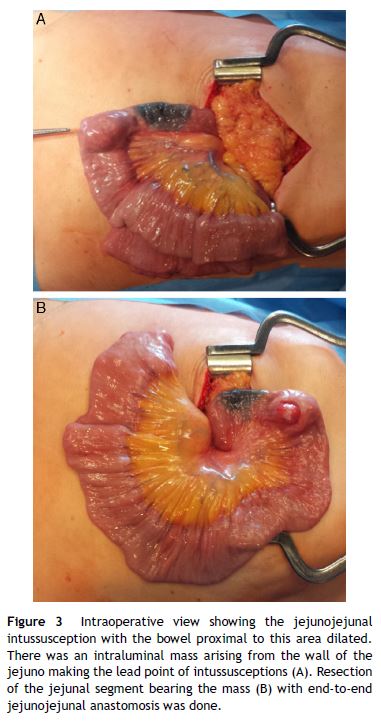
A 58-year-old woman was previously hospitalized for gastrointestinal bleeding (melena) requiring frequent blood transfusion. Standard gastrointestinal endoscopic study (upper endoscopy, colonoscopy) revealed no gastrointestinal lesions. The patient underwent capsule endoscopy, which identified an angiodysplasia in the mid-jejunum. She was referred to double balloon enteroscopy for specific thermal therapy. While waiting for this intervention the patient started persistent nausea and postprandial vomiting, suggesting a suboclusive lesion. The enteroscopy revealed an ulcerative subepithelial lesion protruding to the lumen of the proximal jejunum (Fig. 1). Biopsies were performed (which were inconclusive) and the lesion, that was partially obstructive, was marked with India ink tattoo. Computed tomographic scan showed in the proximal jejunum a hypervascular mass with 3 cm suggestive of GIST conditioning intussusception in this segment (Fig. 2A and B). The patient underwent laparotomy that identified a jejunojejunal intussusception secondary to jejunal tumor (Fig. 3A and B). The lesion was resected and histological examination revealed a GIST tumor (R0). The recovery was uneventful and the patient was discharged on the 7th postoperative day. There was no clinical or radiologic evidence of recurrence at follow-up (Stage I-T2, N0, M0).
This case reveals a false negative of capsule endoscopy in a large proximal small bowel tumor, the simultaneous presentation of a GIST lesion as an intestinal intussusception and gastrointestinal bleeding as well as the importance of balloon enteroscopy and abdominal CT in the evaluation of these patients.
References
1. Kakaria A, Daradkeh S. Jejunojejunal intussusception induced by a gastrointestinal stromal tumor. Case Rep Surg. 2012;2022:173680. [ Links ]
2. Sankey RE, Maatouk M, Mahmood A, Mazhar R. Case report: jejunal gastrointestinal stromal tumour, a rare tumour, with a challenging diagnosis and a successful treatment. J Surg Case Rep. 2015;5:1-3. [ Links ]
3. Rabbani K, Narjis Y, Finech B, Elidrissi A. Unusual malignant cause of adult intussusception: stromal tumor of the small bowel. J Emerg Trauma Shock. 2010;3:306. [ Links ]
4. Martis J, Rajeshwara K, Murulya K, Raghavendra B, Alex K. A rare cause of jejunojejunal intussusception in an adult. Indian J Surg. 2013;75:18-20. [ Links ]
5. Dhull A, Kaushal V, Dhankhar R, Atri R, Singh H, Marwah N. The inside mystery of jejunal gastrointestinal stromal tumor. Case Rep Oncol Med. 2011;10:1155. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
* Corresponding author.
E-mail address: silviagiestas@gmail.com (S. Giestas).
Received 9 November, 2015; accepted 17 December 2015














