Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.22 no.5 Lisboa out. 2015
https://doi.org/10.1016/j.jpge.2015.05.005
CLINICAL CASE
Finding a Needle in a Haystack: The Diagnosis of a Rectal Neuroendocrine Tumor by Transrectal Prostate Biopsy
Tumor Neuroendócrino do Reto Diagnosticado por Biopsia Prostática
Rosa Coelhoa,∗, Susana Rodriguesa, Roberto Silvab, Helena Baldaiab, Guilherme Macedoa
a Gastroenterology Department, Centro Hospitalar São João, Porto, Portugal
b Pathology Department, Centro Hospitalar São João, Porto, Portugal
* Corresponding author.
ABSTRACT
Introduction: Prostate biopsy, usually performed by a transrectal approach, is executed when there is a suspicion of prostate cancer. Neuroendocrine tumors (NETs) are epithelial neoplasms with predominant neuroendocrine differentiation and only 19% of them are localized in the rectum.
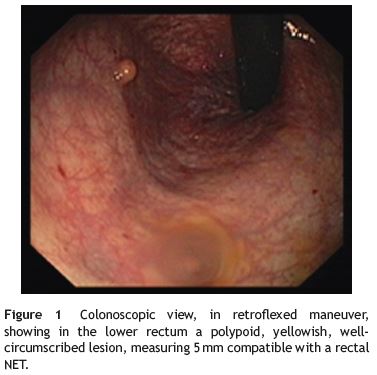
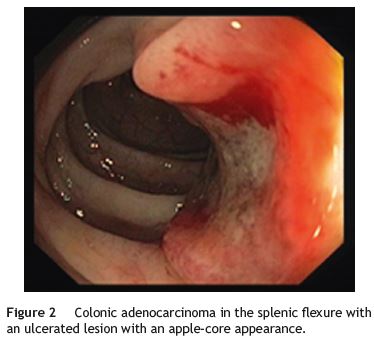
Case report: The authors describe a 73-year-old man without a significant past medical history that underwent a prostate biopsy because of urinary complaints and elevated serum levels of prostate specific antigen. The histology revealed a well-differentiated NET characterized as a low-grade tumor (G1). A total colonoscopy revealed a 5mm sessile rectal polyp and in the splenic flexure a sessile lesion with central ulceration with 5 cm with histological features compatible with an adenocarcinoma.
Conclusion: This is the first case reported in the literature of a rectal NET diagnosed by transrectal prostate biopsy. This case is particularly unique because the diagnosis of the NET lead to the subsequent timely detection of a colonic adenocarcinoma.
Keywords: Biopsy; Carcinoma, Neuroendocrine; Prostate/pathology; Rectal Neoplasms
RESUMO
Introdução: A biópsia prostática transretal é realizada na suspeita de cancro da próstata. Os tumores neuroendócrinos (TNE) são neoplasias epiteliais com diferenciação predominante neuroendócrina e em 19% dos casos localizam-se no reto.
Caso: Os autores descrevem o caso de um homem, 73 anos de idade, sem antecedentes médicos prévios, que por elevação dos níveis séricos de antigénio específico prostático realizou biópsia prostática transretal. A histologia revelou TNE bem diferenciado de baixo grau (G1). Foi realizada posteriormente colonoscopia total onde se observou pólipo séssil de 5mm no reto distal. No ângulo esplénico observou-se ainda um lesão séssil de 5 cm com ulceração central cujas biopsias foram compatíveis com o diagnóstico de adenocarcinoma.
Conclusão: Este é o primeiro caso relatado na literatura de um TNE retal diagnosticado por biópsia prostática transretal. Este caso é peculiar dado que o diagnóstico do TNE do reto permitiu a deteção de um adenocarcinoma do cólon num estadio inicial.
Palavras-Chave: Biopsia; Carcinoma Neuroendócrino; Neoplasias do Reto; Próstata/patologia
1. Introduction
Prostate cancer is the leading cancer site in males after lung cancer,1 however screening the general population remains a controversial issue, since improved patient outcomes have not been demonstrated.2-3 Prostate biopsy, typically performed by an urologist, is a minimally invasive procedure in which tissue samples are obtained through two different anatomic approaches: transrectal (the most common) and transperineal.4 Patients are referred to prostate biopsy in the presence of abnormal digital rectal exam or when repeated abnormal prostate specific antigen (PSA) values are found.5
Neuroendocrine tumors (NETs) are epithelial neoplasms with predominant neuroendocrine differentiation.6 There are two major categories: well and poorly differentiated gastrointestinal NETs. NETs of the digestive system are relatively rare and 19% of them are localized in the rectum.11 Despite the low frequency of colorectal NETs, they are frequently associated with synchronous or metachronous other tumors, with an annual incidence reported of 3-15%.7,8
The authors describe a case report where a polypoid rectum NET with 5mm of major diameter was diagnosed by prostate transrectal biopsy. The patient was submitted to a total colonoscopy that revealed not only the rectal lesion, that was removed with a snare, but also a colonic adenocarcinoma in the splenic flexure. This is the first case reported in the literature of a rectal NET diagnosed by transrectal prostate biopsy.
2. Case presentation
We describe the case of a 73-year-old man that complained of nocturia and pollakiuria and had high PSA level. A transrectal prostate biopsy was performed and revealed a well-differentiated NET characterized as a low-grade tumor (G1).
Total colonoscopy showed, in the distal rectum, a polypoid, yellowish, well-circumscribed lesion, measuring 5mm (Fig. 1) removed with a diathermic snare. Biopsies were taken from a 5-cm ulcerated lesion observed in the splenic flexure occupying half of the circumference of the lumen (Fig. 2).
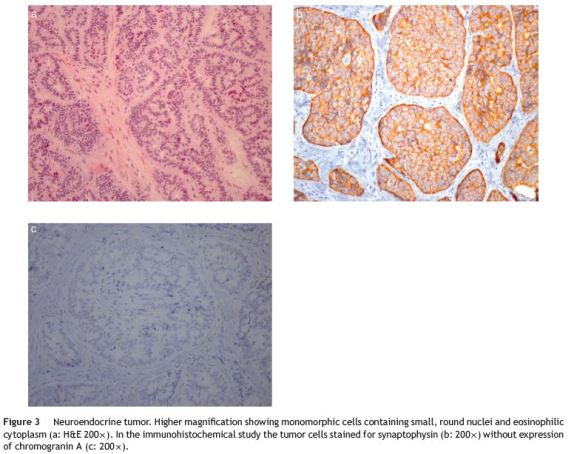
Histologically, the rectal lesion was a tumor centered in submucosa and focally in the mucosa with a trabecular and acinar pattern composed by small and monomorphic cells with round and hyperchromatic nuclei and eosinophilic cytoplasm (Fig. 3a). There was no necrosis or lymphovascular invasion. The immunohistochemical study revealed strong and diffuse staining of the tumor cells for synaptophysin without expression of chromogranin A (Fig. 3b and Fig. 3c). Mitotic index was less than 1 mitosis per 10 high-power field. The proliferative index by Ki-67 was less than 1%. With these histological and immunohistochemical features the diagnosis of a well-differentiated of low-grade NET was made.
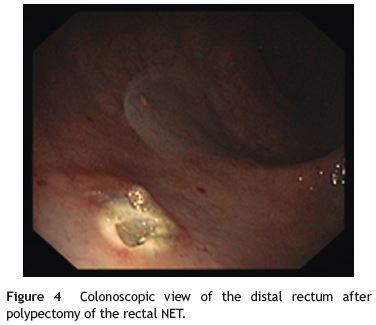
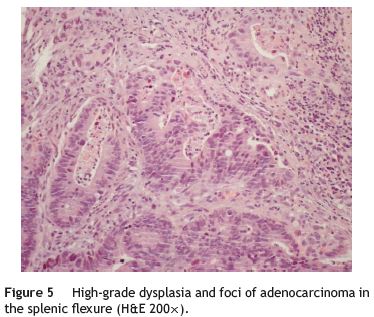
The rectal NET was completely excised with a diathermic snare without complications (Fig. 4). Colonic biopsies from the splenic flexure lesion showed tubulovillous adenoma with high-grade dysplasia and foci of intramucosal adenocarcinoma (Fig. 5).
Thoracic, abdominal and pelvic computed tomography was performed and revealed no metastases nor lymphadenopathies. Laparoscopic left hemicolectomy was successfully performed and the colonic adenocarcinoma was staged as pT2N0M0.
3. Discussion
Prostate cancer is the second most frequent cancer in men, however screening the general population remains a controversial issue.1,2 Prostate biopsy is an invasive procedure made usually through transrectal approach.3 We describe a patient with a histological diagnosis of NET (G1) after a prostate biopsy. The diagnosis was confirmed performing a colonoscopy that revealed in the distal rectum a polypoid, yellowish, well-circumscribed lesion measuring 5mm. The colonoscopy performed showed an ulcerated lesion in the splenic flexure compatible with colonic adenocarcinoma. The authors describe a case of a successful diagnosis of a rectum NET made by prostate transrectal biopsy that allowed an adenocarcinoma colonic diagnosis.
The NET, traditionally referred as carcinoid, often has the appearance of well circumscribed round lesions in the submucosa or extending to the muscular layer. As shown in Fig. 3, the cut surface sometimes has a yellowish color reflecting the high lipid content of these lesions. The colonoscopy performed in order to confirm the histology of prostate biopsy revealed another neoplasm - a colonic adenocarcinoma of the splenic flexure. In fact, as many as 29% of gastrointestinal carcinoids exhibit a synchronous or metachronous association with other tumors, usually adenocarcinomas of the colon.9 Our patient performed thoracic and abdominopelvic computed tomography that excluded the presence of metastasis. A somatostatin receptor scintigraphy was also performed and did not reveal significant changes. Imaging by positron-emission tomography is not routinely recommended for NETs because most of these tumors are well differentiated and have a low metabolic rate.10
According to the TNM staging system of the American Joint Committee on Cancer/Union for International Cancer Control the tumor was classified as T2N0M0 (tumor invades muscularis propria without regional lymph node metastasis and no distant metastasis).11 The surgical resection is the primary treatment modality for these patients with localized colorectal cancer. A laparoscopic left hemicolectomy was performed without complications.
Taking into consideration this case we think that patients could be submitted to screening colonoscopy or flexible sigmoscopy before performing prostate biopsy. In fact, even if it is low, the risk of tumor dissemination during the prostate biopsy in the presence of rectal tumors must be considered.
4. Conclusion
To the best of our knowledge, in the literature this is the first rectum NET diagnosed by prostate transrectal biopsy. Although prostate biopsy is a relatively frequent procedure, this is the first case of a NET diagnosed in this manner. This case is particularly unique because the diagnosis of the NET lead to the subsequent timely detection of a colonic adenocarcinoma.
References
1. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9-29. [ Links ]
2. Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360:1320-8. [ Links ]
3. Andriole GL, Crawford ED, Grubb RL 3rd, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360:1310-9. [ Links ]
4. Ismail MT, Gomella LG. Transrectal prostate biopsy. Urol Clin N Am. 2013;40:457-72. [ Links ]
5. Greene KL, Albertsen PC, Babaian RJ, Carter HB, Gann PH, Han M, et al. Prostate specific antigen best practice statement: 2009 update. J Urol. 2013;189:S2-11. [ Links ]
6. Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin N Am. 2011;40:1-18. [ Links ]
7. Moore JR, Greenwell B, Nuckolls K, Schammel D, Schisler N, Schammel C, et al. Neuroendocrine tumors of the rectum: a 10-year review of management. Am Surg. 2011;77:198-200. [ Links ]
8. Ballantyne GH, Savoca PE, Flannery JT, Ahlman MH, Modlin IM. Incidence and mortality of carcinoids of the colon: data from the Connecticut Tumor Registry. Cancer. 1992;69:2400-5. [ Links ]
9. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;15:934-59. [ Links ]
10. Kocha W, Maroun J, Kennecke H, Law C, Metrakos P, Ouellet JF, et al. Consensus recommendations for the diagnosis and management of well-differentiated gastroenterohepatic neuroendocrine tumours: a revised statement from a Canadian National Expert Group. Curr Oncol. 2010;17:49-64. [ Links ]
11. AJCC American Joint Committee on Cancer. In: Edge SB, Byrd DR, Compton CC, editors. Cancer staging manual. 7th ed. New York: Springer; 2010. p. 143. [ Links ]
Abbreviations: NET, neuroendocrine tumor; PSA, prostate specific antigen; TNM, tumor node metastases.
* Corresponding author.
E-mail address: rosacoelhoabrantes@hotmail.com (R. Coelho).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 20 February 2015; accepted 19 May 2015














