Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.22 no.3 Lisboa jun. 2015
https://doi.org/10.1016/j.jpge.2015.03.003
ORIGINAL ARTICLE
Impact of Bariatric Surgery on Patients from Goiás, Brazil, Using the BAROS Method - A Preliminary Study
Impacto da Cirurgia Bariátrica em Pacientes de Goiás, Brasil, Usando Metodologia BAROS - Um Estudo Preliminar
Emmeline Flor Ribeiro∗,1, Renato Ivan de Ávila ∗,1, Rosineide Ribeiro de Sousa Santos, Clévia Ferreira Duarte Garrote
Faculty of Pharmacy, Universidade Federal de Goiás, Goiânia, Brazil
* Corresponding authors.
ABSTRACT
Introduction: As obesity is currently a major public health problem, bariatric surgery has been widely indicated due to the difficulties involved in the clinical management of obese adults.
Objectives: Assess the quality-of-life (QOL) of patients who had undergone Roux-en-Y Gastric Bypass (RYGB) in the State of Goiás, Brazil, where as yet no studies have been published on the QOL of patients who underwent bariatric surgery.
Methods: A retrospective study, using the Bariatric Analysis and Reporting Outcome System (BAROS), was carried out in Goiânia and Rio Verde, Goiás, Brazil, with 50 over 18-year-old patients of both genders, who had undergone RYGB and had at least three months of postoperative time.
Results: Before RYGB, 48% of the individuals were classified as morbidly obese. Average weight and body mass index (BMI) of the 50 patients interviewed were 119.37±18.44 kg and 43.54±5.33 kg/m2, respectively. By contrast, after the RYGB these parameters decreased significantly to 78.01±11.06 kg and 28.46±3.61 kg/m2, respectively, mainly from the 3rd to 85th month of postoperative time (p < 0.0001). As well as that, 78% reported having presented preoperative comorbidities, especially hypertension (44%), rheumatism (34%), dyslipidemia (24%) and diabetes (20%). However, after surgery, the resolution rates were 77, 24, 100 and 100%, respectively, for these same clinical conditions. In terms of QOL, some patients reported feeling better (8%) or much better (92%) after RYGB. The outcome of the BAROS method for those patients was classified as fair (2%), good (8%), very good (24%) and excellent (66%).
Conclusions: Preliminary results indicated that RYGB could be a successful surgical procedure to promote satisfactory and sustained reduction in the body measurements of morbidly obese patients from Goiás, Brazil. Furthermore, the final BAROS score showed improvements in associated comorbidity and also in the QOL of these patients.
Keywords: Bariatric Surgery; Brazil; Obesity, Morbid; Quality of Life
RESUMO
Introdução: Como a obesidade é atualmente um grande problema de saúde pública, a cirurgia bariátrica tem sido amplamente indicada devido às dificuldades envolvidas no manejo clínico de adultos obesos.
Objetivos: Avaliar a qualidade de vida (QDV) de pacientes submetidos ao Desvio Gástrico em Y-de-Roux (DGYR) no Estado de Goiás, Brasil, onde ainda não há estudos sobre a QDV de pacientes submetidos à cirurgia bariátrica.
Métodos: Um estudo retrospectivo, utilizando o Bariatric Analysis and Reporting Outcome System (BAROS), foi realizado em Goiânia e Rio Verde, Goiás, Brasil, com 50 pacientes com idade superior a 18 anos, de ambos os gêneros, que realizaram DGYR com tempo pós-operatório mínimo de três meses.
Resultados: Antes da DGYR, 48% dos indivíduos foram classificados como obesos mórbidos. A média de peso e índice de massa corporal (IMC) dos 50 pacientes entrevistados foram 119,37±18,44Kg e 43,54±5,33Kg/m2, respectivamente. Em contrapartida, após a DGYR, esses parâmetros diminuíram significativamente para 78,01±11,06 kg e 28,46±3,61 kg/m2, respectivamente, principalmente do 3◦ ao 85◦ mês de tempo pós-operatório (p < 0.0001). Além disso, 78% reportaram tendo apresentado comorbidades pré-operatórias, especialmente hipertensão (44%), reumatismo (34%), dislipidemia (24%) e diabetes (20%). Entretanto, após a cirurgia, as taxas de resolução foram de 77, 24, 100 e 100%, respectivamente, para essas mesmas condições clínicas. Em termos de QDV, alguns pacientes relataram se sentir melhor (8%) ou muito melhor (92%) após a DGYB. O resultado do método BAROS para esses pacientes foi classificado como insuficiente (2%), bom (8%), muito bom (24%) e excelente (66%).
Conclusões: Resultados preliminares indicaram que a DGYB pode ser um procedimento cirúrgico para promover com sucesso a redução satisfatória e sustentada nas medidas corporais de pacientes com obesidade mórbida provenientes de Goiás, Brasil. Além disso, a pontuação final do BAROS mostrou melhorias das comorbidades associadas e também na QDV desses pacientes.
Palavras-Chave: Brasil; Cirurgia Bariátrica; Obesidade Mórbida; Qualidade de Vida
1. Introduction
Obesity which is responsible for comorbidities such as diabetes, ischemic heart disease, hypertension and atherosclerosis, is currently a major public health problem of great prevalence. Furthermore, overall mortality due to this clinical condition has increased over the years.1,2
Consequently, dietary and pharmacotherapeutic treatments are undertaken for weight loss and maintenance. However, studies have shown that clinical and nutritional treatment present no significant result in the long term. Hence, bariatric surgery has been widely indicated due to the difficulties involved in the clinical management of severely obese adults.3-7
The main benefits accruing from this surgery are the resolution of comorbidities, weight loss and maintenance, all of which lead to an improvement in the quality-of-life.8,9 Furthermore, expenditure involving medicines, health professionals and tests progressively decrease after the operation. This is more evident in patients with more comorbidity. Therefore, this surgery produces substantial economic benefits for health systems and/or patients, which, in turn, compensate for the considerable expenses involved in undergoing bariatric surgery.10-12
Resolution 1.942/2010 of Brazils Federal Council of Medicines13 presents the accepted procedures for this surgical practice, in which the Roux-en-Y Gastric Bypass (RYGB) is widely recommended (40%).14
RYGB provides proper and long-lasting weight loss in conjunction with low failure rates and few long-term complications. Nutritional and metabolic accompaniment of the patient is easy and the surgery is reversible, although this involves certain technical difficulties. In addition, it presents excellent results in terms of improved quality-of-life and treatment of related diseases.13
However, the literature highlights certain postoperative complications such as dumping syndrome (nausea, vomiting, flushing, abdominal pain and symptoms of hypoglycemia), gastric obstruction, rupture of the staple line and some specific micronutrient deficiencies, which demand adequate nutritional intervention.15 In addition, such patients are classified with lower quality-of-life. Thus, efficient approaches are needed to ensure weight reduction and also to improve quality-of-life of patients who have undergone RYGB.
Assessment of the effectiveness of surgical treatment requires specific and appropriate evaluation methods given all the variables which influence the outcome of bariatric surgery.16 Hence, it is important to use standardized and reliable methods, such as the Bariatric Analysis and Reporting Outcome System (BAROS) proposed by Oria and Moorehead.17
Given this scenario, this preliminary study evaluated the effectiveness and impact of RYGB bariatric surgery on the quality-of-life of patients in two locations in the State of Goiás, Brazil, using the BAROS method.
2. Materials and methods
A retrospective study was carried out, in Goiânia and Rio Verde, Goiás, Brazil, with 50 over 18-year-old patients of both genders, who had undergone RYGB and had at least three months of postoperative time. These towns represent, respectively, the Central and Southern mesoregions of Goiás, a state where to date, no studies have been published on the quality-of-life of patients who have undergone bariatric surgery.
After approval by the Research Ethics Committee of the Federal University of Goiás, Brazil (FUG no. 048/2012), periodic visits to public and private health facilities were conducted to invite patients who had undergone RYGB to participate in this study. The invitation was realized by chance for patients that we found in the health facilities during the days visited. When it was not possible to interview a patient while waiting for their consultation, they were interviewed later and were also asked if they knew other patients who had RYGB. A total of 55 patients were invited to participate in this study, two of whom refused for unexplained reasons.
Interviews were conducted between July and August 2012, after each respondent had completed the Free and Clarified Consent Term, using the BAROS questionnaire (Appendix). All information used in the research was provided by the patients, thus clinical charts were not assessed. The hospitals involved are accredited for bariatric surgery.
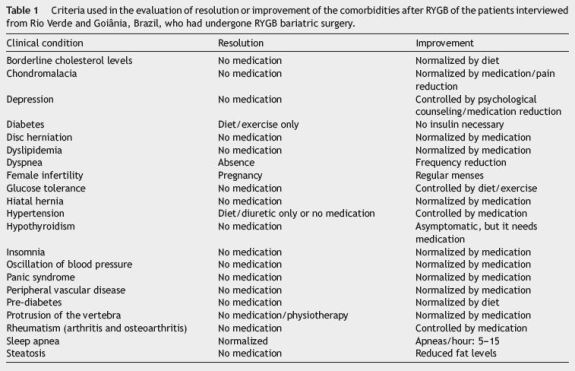
The BAROS questionnaire17 quantitatively evaluates the quality-of-life of patients who have undergone bariatric surgery for the long term treatment of obesity in three main areas: percentage of excess weight loss (%EWL), changes in medical conditions (comorbidities) and quality-of-life. It considers self-esteem, physical activities, social relationships, willingness to work and sexual interest. The system defines five outcome groups (failure, fair, good, very good, and excellent), based on a scoring table which adds or subtracts points in accordance with the existence of complications and/or reoperation while evaluating the three main areas described above. As adapted from Oria and Moorehead,17 Table 1 shows the criteria used in the evaluation of resolution or improvement of the comorbidities after RYGB of the patients interviewed in this study.
Of the 53 patients interviewed, 50 met the inclusion criteria for the study: over 18 female or male patients, who had undergone RYGB at least three months previously. The exclusion criteria meant that patients under 18, who had undergone bariatric surgery less than three months previously (n = 1) and individuals operated with other types of bariatric surgery such as sleeve gastrectomy (n = 2) were not included.
The distribution data of patients was performed using descriptive statistics: mean, standard deviation, minimum and maximum values, absolute and relative data, numeric and percentile values. The inter group variation was measured by the one-way analysis of variance (ANOVA) or two-way ANOVA followed by the Bonferroni test. Statistical significance was set at p < 0.05.
3. Results
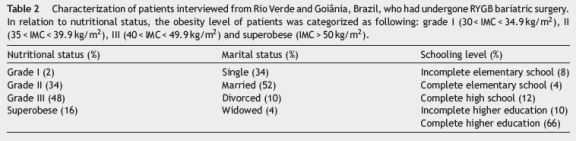
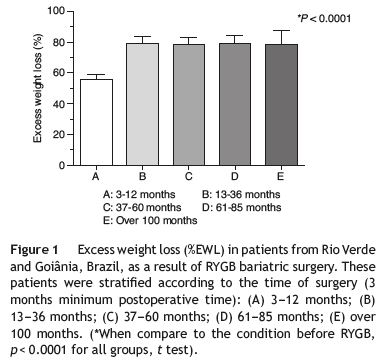
Of the patients interviewed after RYGB bariatric surgery, 13 (26%) were from Rio Verde and 37 (74%) from Goiânia. In the former group, 15 and 85% were male and female, respectively, while in the latter this frequency was 22 and 78%, in the same order. These patients were stratified according to the time of surgery (3 months minimum of postoperative time): (A) 3-12 months (n = 14); (B) 13-36 months (n = 13); (C) 37-60 months (n = 12); (D) 61-85 months (n = 8); (E) over 100 months (n = 3). Age ranged from 22 to 59, with a mean of 39.6 years. Education level, nutritional condition and marital status are presented in Table 2.
A total of 78% reported having presented comorbidities prior to bariatric surgery. As shown in Table 3, the most prevalent comorbidities presented prior to the surgical procedure were hypertension (44%), rheumatism (arthritis and osteoarthritis) (34%), dyslipidemia (24%) and diabetes (20%). On the other hand, all respondents who had diabetes before the bariatric surgery reported not using diabetes medications due to resolution of this condition by RYGB. Similar findings were observed in patients who had dyslipidemia. Regarding hypertension, patients showed 77% of resolution. Moreover, 90% of patients reported resolution of sleep apnea, while 76% showed improvement of rheumatism. Additionally, other clinical conditions were also improved or resolved by surgery.
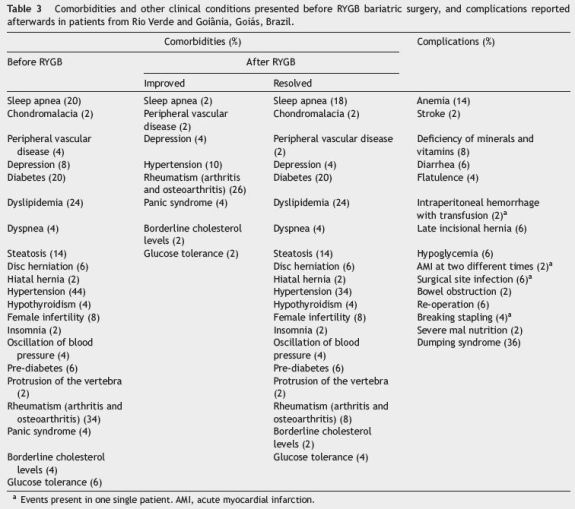
However, 60% of respondents said they experienced certain complications. There was a higher prevalence of minor complications, such as dumping syndrome (36%) and anemia (14%), than of severe complications. In addition, a reduced reoperation rate (6%) was found, but only in the case of female patients.
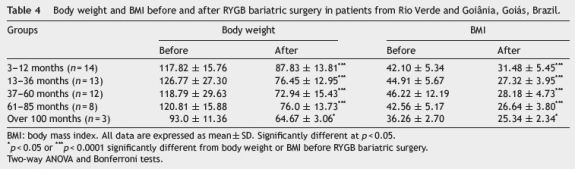
With regard to weight and body mass index (BMI), there was a significant reduction in both parameters after the RYGB bariatric surgery, mainly from the 3rd to 85th month of postoperative time (groups A-D) (p < 0.0001) (Table 4). In addition, the EWL percentage was significantly higher (p < 0.0001), greater than 50% in group A and 80% in groups B-E (Fig. 1).
In terms of quality-of-life aspects, some patients reported feeling better (8%) or much better (92%) after surgery. In addition, 8% stated that their physical activities had decreased, 28% said that they remained stable, while the remaining 64% said that they had increased. Furthermore, 2% reported that they were attending less social and family gatherings. Others stated that nothing had changed in this respect (32%), while a larger number said that their social activities had increased (66%). A small number of interviewees reported that their working capacity had reduced (2%) or remained unchanged (12%), while, on the other hand, 86% said theirs had improved. On the question of sexual activity, several patients declared that their interest was the same (28%) or higher (68%), while a minority (4%) reported a decrease.
So in terms of the BAROS method, the outcome for those patients who had undergone RYGB bariatric surgery was classified as fair (2%), good (8%), very good (24%) and excellent (66%) (Fig. 2).
4. Discussion
In recent years, the popularity of bariatric surgery has increased and RYGB had been classified as the most common weight loss procedure.18 In view of that, a retrospective study of quality-of-life was carried out with 50 patients who underwent RYGB in Goiânia and Rio Verde, Goiás, Brazil, a region where no studies had previously been published on the quality-of-life of patients who had undergone bariatric surgery.
It was obtained preliminary results using the BAROS, a standardized methodology. Despite the availability of other specific questionnaires to assess the quality-of-life of patients undergoing bariatric surgery, the literature has shown that the BAROS method is suitable for this evaluation.19-21 However, some limitations were pointed out in this study such as the self-declaration of occurrence or absence of comorbidities and other data, reduced sample size and no evaluation of patients in different periods of time. On the other hand, the results obtained here were similar to other relevant studies22-28 and these data support other larger studies.
The majority of obese patients interviewed showed satisfactory results after RYGB since excess weight loss was significantly higher and was associated with high rates of resolution of comorbidities due to obesity, minor post-surgical complications and improved quality-of-life, according to the Oria and Moorehead criteria.17
In relation to preoperative comorbidities, the prevalence was high (78%), similar to that observed in the literature.26,27 However, Faria et al22 and Vázquez et al29 found still higher rates, 93 and 88.1%, respectively. Hypertension was the most prevalent comorbidity (44%) presented. It was also found by Vázquez et al29 and Costa et al30 (47.7 and 63.49%, respectively). However, in the Faria et al22 study, sleep apnea and dyslipidemia were most prevalent. This relatively high number of comorbidities points to the need for effective weight loss treatment for obese patients. In this context, bariatric surgery has been shown to be a useful clinical approach, since all patients interviewed in the studies presented considerable improvement or resolution of their medical conditions.
Toledo et al31 pointed out the benefits as 63.9% of patients presented reduced hypertension and lipid levels. Higa et al32 demonstrated improvement and/or resolution in 87, 67, and 76% of patients with hypertension, dyslipidemia, and sleep apnea, respectively. Díaz and Folgueras25 noted resolution of the following comorbidities: diabetes (68.7%), hypertension (47.2%), dyslipidemia (43.7%) and sleep apnea (36.3%). Our study showed resolution rates of 100, 77, 100 and 90%, respectively, for these same clinical conditions. In addition, other health problems related by patients were also improved or resolved after RYGB. This surgical procedure has been associated with high rates of long lasting medical resolution especially in metabolic diseases such as diabetes.33 In this regard, recent studies revealed laboratory remission of diabetes in morbidly and non-severely obese patients operated with RYGB.34,35
Although bariatric surgery has been performed since the 1950s, this surgical practice has only become safe and successful in the last two decades. With the increase in the number of surgeries, several complications have arisen. Hence, it is crucial that the predictive risk factors in relation to morbidity and mortality involving bariatric surgery be identified and defined.36 Furthermore, it is worth noting that laparoscopy instead of open surgery has greatly decreased the occurrence of severe surgical complications.32
In our study, 60% of respondents experienced postsurgical complications. Of these the dumping syndrome was most prevalent (36%), similar to another study with 50 patients who underwent RYGB that found an incidence of 42%.18 This finding emphasizes the need for nutritional monitoring during the postoperative follow-up.18,37 In another study, hair loss (73.3%) was most prevalent, followed by dumping syndrome (66.6%).27 These studies highlight the presence of minor complications after bariatric surgery, but do not take from the benefits derived from a reduction in body measurements.10
The weight loss parameter is one of the crucial endpoints in quality-of-life assessment. The patients mean preoperative weight and BMI were 119.37±18.44 kg and 43.54±5.33 kg/m2, respectively, with a prevalence of morbid obesity (48%), in consonance with other studies.27,31 By contrast, after the RYGB bariatric surgery these same parameters decreased significantly to 78.01±11.06 kg and 28.46±3.61 kg/m2, respectively. Weight loss associated with RYGB is multifactorial and well-understood, occurring due to changes in the entero-endocrine axis and restriction of food intake by virtue of a smaller gastric pouch and malabsorptive effects resulting from the distortion of the gastrointestinal anatomy.18
The excess weight loss percentage (%EWL), after 13 months postoperative time was similar to that of other studies, which found 60% EWL after 6 months as compared to 75%, 12 months after surgery.38,39 Weight loss after RYGB bariatric surgery can reach 65-80% within 12-18 months after surgery. However, some weight gain usually occurs within three to five years afterwards. A 5-year follow-up after surgery showed an average EWL oscillating between 50 and 60%.4 According to Suter et al,28 after the same period, 74.9% of patients had an EWL of at least 50% while Harakeh et al19 found an average EWL of 75.3%, 18 months after bariatric surgery.
For this group of patients, especially the morbidly obese, their health-related quality-of-life is poor and expectations of improving it are a reason why patients frequently seek help through bariatric surgery.40 In relation to quality-of-life, the patients interviewed in this study presented very good (24%) or excellent (66%) outcomes in the final BAROS score. Harakeh et al19, Faria et al22 and González et al23 also found a high percentage of patients with excellent outcomes (approximately 60%), while the final scores of Dadan et al24 and Díaz and Folgueras25 rated as very good (57 and 54%, respectively). Recently, another study using SF-36 and Obesity-related Problems scale (OP) instruments showed patients operated with RGYB have better scores in most aspects of quality-of-life compared to non-operated obese individuals, although they did not achieve the levels of the general population.40 As seen here, this study showed that improving obesity-related comorbidity is a prerequisite for good quality-of-life. While improved QOL is triggered by weight loss, patients are also instructed to implement diet and lifestyle changes after gastric bypass surgery.41 Thus, they gain quality-of-life through healthier behavior and this may even be assimilated by their partners.41,42
In addition, psychosocial relations improved for several patients interviewed, since this surgery enhances selfesteem and promotes healthier living in society. Although obesity is a health problem in current society, it is also an esthetic problem, which can affect the obese both emotionally and socially, and thus interfere in their quality-of-life.43
On considering the characteristics of the population in this study, in addition to great body mass, there was a considerable prevalence of women, also observed by other authors.30,44 In their studies, approximately 80% of patients were female, justified by the greater demand for treatment among women. Prevedello et al1 argue that this prevalence may be related to the fact that obese women are more motivated to lose weight than obese men, perhaps as a result of esthetic pressures. In addition, the average age of respondents in this study was about 40 years, which is also similar to that of other studies.25,29,44 Approximately 65% were married, and presented the same profile as the group of patients studied by Guimarães et al26 And most of the respondents were university graduates (66%), with a higher education level, similar to that found in the literature.1
Although this is a preliminary study as a basis for further studies with larger numbers of patients and/or a long-term follow-up, results obtained indicated that the RYGB could be a successful surgical procedure to promote a satisfactory and sustained reduction in the body measurements of morbidly obese patients from Goiás, Brazil. Furthermore, the final BAROS scores showed improvements in associated comorbidity and also in the quality-of-life of these patients.
References
1. Prevedello CF, Colpo E, Mayer ET, Copetti H. Análise do impacto da cirurgia bariátrica em uma população do centro do estado do Rio Grande do Sul utilizando o método BAROS. Arq Gastroenterol. 2009;46:199-203. [ Links ]
2. Santos RS, Pereferrer FS, Fernandez SE, Dejardin DC, Villarrasa N, Bernal DF. Is the morbid obesity surgery profitable in times of crisis? A cost-benefit analysis of bariatric surgery. Cir Espan. 2013;91:474-84. [ Links ]
3. Brolin REMD. Bariatric surgery and long-term control of morbid obesity. JAMA Surg. 2002;288:2793-6. [ Links ]
4. Ravelli MN, Merhi VAL, Mônaco DV, Aranha N. Obesidade, cirurgia bariátrica e implicações nutricionais. Rev Bras Prom Saúde. 2007;20:259-66. [ Links ]
5. Tavares TB, Nunes SM, Santos MO. Obesidade e qualidade de vida: revisão da literatura. Rev Med Minas Gerais. 2010;20:359-66. [ Links ]
6. Ilias EJ. Síndrome metabólica após cirurgia bariátrica. Resultado dependente da técnica realizada. Rev Assoc Med Bras. 2011;57:6. [ Links ]
7. Padwal R, Klarenbach S, Wiebe N, Hazel M, Birch D, Karmali S. Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med. 2011;26:1183-94. [ Links ]
8. Buchuwald H. Consensus Conference Statement Bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005:371-81. [ Links ]
9. Islam N. Obesity: a epidemic of the 21st century. J Pak Med Assoc. 2005;55:166-72. [ Links ]
10. Arcila D, Velázquez D, Gamino R, Sierra M, Salin-Pascual R, González-Barranco J. Quality of life in bariatric surgery. Obes Surg. 2002;12:661-5. [ Links ]
11. Craig BM, Tseng DS. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491-8. [ Links ]
12. Sussenbach SP, Padoin AV, Silva EN, Benzano D, Pufal MA, Barhouch AS. Economic benefits of bariatric surgery. Obes Surg. 2012;22:266-70. [ Links ]
13. Conselho Federal de Medicina. Resolução CFM n◦. 1.942/2010, de 12 de fevereiro de 2010. Diário Oficial da União, Seção I, p. 72, Brasília, DF, 5 February 2010. [ Links ]
14. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605-11. [ Links ]
15. Cruz MRR, Morimoto IMI. Intervenção nutricional no tratamento cirúrgico da obesidade mórbida: resultados de um protocolo diferenciado. Rev Nutr. 2004;17:263-72. [ Links ]
16. Victorzon M, Tolonen P. Bariatric Analysis and Reporting Outcome System (BAROS) following laparoscopic adjustable gastric banding in Finland. Obes Surg. 2001;11:740-3. [ Links ]
17. Oria HE, Moorehead MK. Bariatric Analysis and Reporting Outcome System (BAROS). Obes Surg. 1998;8:487-99. [ Links ]
18. Banerjee A, Ding Y, Mikami DJ, Needleman BJ. The role of dumping syndrome in weight loss after gastric bypass surgery. Surg Endosc. 2013;27:1573-8. [ Links ]
19. Harakeh AB, Larson CJ, Mathiason MA, Kallies KJ, Kothari SN. BAROS results in 700 patients after laparoscopic Roux-en-Y gastric bypass with subset analysis of age, gender, and initial body mass index. Surg Obes Relat Dis. 2011;7:94-8. [ Links ]
20. Guedes AC, Virgens AA, Nascimento CE, Vieira MPB. Qualidade de vida em pacientes submetidos à cirurgia bariátrica do tipo derivação biliopancreática com preservação gástrica (DBPPG). Rev Inst Cienc Saude. 2009;27:209-13. [ Links ]
21. Bobowicz M, Lehmann A, Orlowisk M, Lech P, Michalik M. Preliminary outcomes 1 year after laparoscopic sleeve gastrectomy based on bariatric analysis and reporting outcome system (BAROS). Obes Surg. 2011;21:1843-8. [ Links ]
22. Faria OP, Pereira VA, Gangoni CMC, Lins RD, Leite S, Rassi V. Obesos mórbidos tratados com gastroplastia redutora com bypass gástrico em Y de Roux: análise de 160 pacientes. Bras Méd. 2002;39:26-34. [ Links ]
23. González JF, Gómez G, Arraigada G. Evaluación mediante score BAROS de los resultados del bypass gástrico en el tratamiento de la obesidad mórbida. Rev Chil Cir. 2006;58:365-70. [ Links ]
24. Dadan J, Iwacewicz P, Hady HR. Original paper. Quality of life evaluation after selected bariatric procedures using the Bariatric Analysis and Reporting Outcome System. Videosurg Miniinv. 2010;5:93-9. [ Links ]
25. Días GE, Folgueras MT. Preoperative determinants of outcomes of laparoscopic gastric bypass in the treatment of morbid obesity. Nutr Hosp. 2011;26:851-5. [ Links ]
26. Guimarães J, Rodrigues D, Campos MV, Melo M, Bastos M, Milheiro A. Factores preditivos da perda de peso após cirurgia bariátrica. Revista Portuguesa de Endocrinologia, Diabetes e Metabolismo. 2006;2:7-11. [ Links ]
27. Bregion NO, Silva SA, Salvo VLMA. Estado Nutricional e condição de saúde de pacientes nos períodos pré e pós-operatório de cirurgia bariátrica. Rev Bras Ciênc Saúde. 2007:33-42, ano III (14). [ Links ]
28. Suter M, Donadini A, Romy S, Demartines N, Giusti V. Laparoscopic Roux-En-Y Gastric Bypass: significant long-term weight loss, improvement of obesity-related comorbidities and quality of life. Ann Surg. 2011;254:267-73. [ Links ]
29. Vásquez PA, Orón M, Ríspoli T. Valoración de la evolución de las comorbilidades de la obesidad mórbida tras tratamiento quirúrgico mediante la técnica del cruce duodenal. Nutr Hosp. 2007;22:596-601. [ Links ]
30. Costa AC, Ivo ML, Cantero WB, Tognini JRF. Obesidade em pacientes candidatos a cirurgia bariátrica. Acta Paul Enferm. 2009;22:55-9. [ Links ]
31. Toledo CC, Camilo GB, Guimarães RL, Moraes FR, Júnior CS. Qualidade de vida no pós-operatório tardio de pacientes submetidos à cirurgia bariátrica. Rev APS. 2010;13:202-9. [ Links ]
32. Higa K, Ho T, Tercero F, Yunus T, Boone KB. Laparoscopic Rouxen-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7:516-25. [ Links ]
33. Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP, Sledge I. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248-56. [ Links ]
34. Li Q, Chen L, Yang Z, Ye Z, Huang Y, He M, Zhang S, Feng X, Gong W, Zhang Z, Zhao W, Liu C, Qu S, Hu R. Metabolic effects of bariatric surgery in type 2 diabetic patients with body mass index <35 kg/m2. Diabetes Obes Metab. 2012;14:262-70. [ Links ]
35. Kaska Ł, Proczko M, Kobiela J, Stefaniak TJ, Śledziński Z. Dynamics of type 2 diabetes mellitus laboratory remission after Roux-en-Y gastric bypass in patients with body mass index lower than 35 kg/m2 and higher than 35 kg/m2 in a 3-year observation period. Videosurg Miniinv. 2014;9:523-30. [ Links ]
36. Hintze LJ, Bevilaqua CA, Pimentel EB, Nardo N Jr. Cirurgia bariátrica no Brasil. Rev Cien Med. 2011;20:87-98. [ Links ]
37. Heber D, Greenway FL, Kaplan LM, Livingston E. Endocrine and nutritional management of the post-bariatric surgery patient: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:4823-43. [ Links ]
38. Carrasco F, Ruz M, Rojas P, Csendes A, Rebolledo A, Codoceo J. Changes in bone mineral density, body composition and a adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg. 2006;19:41-6. [ Links ]
39. Wolf AM, Beisiegel U. The effect of loss of excess weight on the metabolic risk factor after bariatric surgery in morbidly and super-obese patients. Obes Surg. 2007;17:910-9. [ Links ]
40. Raoof M, Näslund I, Rask E, Karlsson J, Sundbom M, Edholm D, Karlsson FA, Svensson F, Szabo E. Health-related quality-of-life (HRQoL) on an average of 12 years after gastric bypass surgery. Obes Surg. 2015, http://dx.doi.org/10.1007/s11695-014-1513-6 (in press). [ Links ]
41. Woodard GA, Encarnacion B, Peraza J, Hernandez-Bousard T, Morton J. Halo effect for bariatric surgery: collateral weight loss in patients family members. Arch Surg. 2011;146:1185-90. [ Links ]
42. Aarts F, Radhakishun NN, van Vliet M, Geenen R, von Rosenstiel IA, Hinnen C, Beijnen JH, Brandjes DP, Diamant M, Gerdes VE. Gastric bypass may promote weight loss in overweight partners. J Am Board Fam Med. 2015;28:90-6. [ Links ]
43. Martínez Y, Ruiz-López MD, Giménez R, Pérez de la Cruz AJ, Orduña R. Does bariatric surgery improve the patients quality of life? Nutr Hosp. 2010;25:925-30. [ Links ]
44. Branson R, Potoczna N, Brunotte R, Piec G, Ricklin T, Steffen R, et al. Impact of age, sex and body mass index on outcomes at four years after gastric banding. Obes Surg. 2005;15:834-42. [ Links ]
* Corresponding author.
E-mail addresses: peritaemmeline@gmail.com (E.F. Ribeiro), avila.ri@hotmail.com (R.I. de Ávila).
1 These authors equally contributed for this study and are the corresponding authors.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
All authors declare no conflict of interest regarding all sections of this research, considering project elaboration, research execution and results expression.
Contributors
E. F. Ribeiro and R.I. Ávila equally participated in the project elaboration; research execution; data collection; analysis and expression of results; literature review; and writing of the manuscript. R. R. S. Santos participated in the project elaboration; data collection; literature review; and writing of the manuscript. C. F. D. Garrote oriented the study and contributed to the final draft.
Received 7 November 2014; accepted 13 March 2015
Appendix 1














