Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.22 no.1 Lisboa fev. 2015
https://doi.org/10.1016/j.jpge.2014.09.002
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
A Case of Obstructive Jaundice
Um Caso de Icterícia Obstrutiva
Nuno Veloso∗, Sara Pires, Rogério Godinho
Gastroenterology Department, Hospital Espírito Santo, Évora, Portugal
* Corresponding author.
An 84-year-old woman presented with a 2-day history of jaundice, fever and abdominal pain. Physical examination showed scleral icterus and right upper quadrant tenderness without inspiratory arrest at palpation (absent Murphys sign). Laboratory workup revealed leukocytosis (12.4×103 aL), elevated C-reactive protein (8.3 mg/dL) and cholestasis (bilirubin 5.4 mg/dL, alkaline phosphatise 893 U/L, gamma-glutamyl transferase 1143 U/L) with elevated liver enzymes (aspartate aminotransferase 231 U/L, alanine aminotransferase 178 U/L). Abdominal ultrasound demonstrated a scleroatrophic gallbladder with cholelithiasis and an impacted large gallstone in the common bile duct with dilated common and intrahepatic bile ducts.
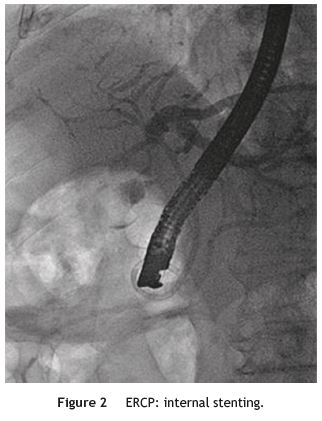
We performed an endoscopic retrograde cholangiopancreatography (ERCP) that clearly showed common hepatic duct compression by a large gallstone (20 mm) impacted in the cystic duct (Fig. 1), compatible with the diagnosis of Mirizzi syndrome. Successful biliary decompression was performed by internal stenting (Fig. 2) with subsequent patient referral to surgery (cholecystectomy plus closure of the fistula).
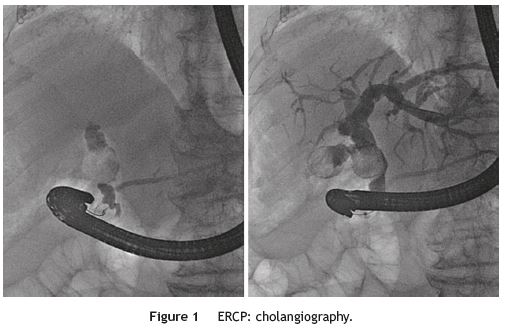
The Mirizzi syndrome refers to common hepatic duct obstruction caused by an extrinsic compression from an impacted stone in the cystic duct or Hartmanns pouch of the gallbladder.1 The majority of the patients present the clinical triad of jaundice, fever, and right upper quadrant pain, showing in the laboratory evaluation elevations in the serum concentrations of alkaline phosphatase and bilirubin.2
The Mirizzi syndrome is part of the differential diagnosis of obstructive jaundice and therefore the diagnostic approach usually begins with ultrasonography complemented by ERCP or magnetic resonance cholangiography.
A useful classification system takes into account the presence and extent of a cholecystobiliary fistula, due to erosion of the anterior or lateral wall of the common bile duct by impacted stones.3
Surgery is the mainstay of therapy for Mirizzi syndrome.4 ERCP treatment can be effective as a temporizing measure before surgery and can be definitive treatment for unsuitable surgical candidates.
References
1. Alberti-Flor JJ, Iskandarani M, Jeffers L, Schiff ER. Mirizzi syndrome. Am J Gastroenterol. 1985;80:822. [ Links ]
2. Binmoeller KF, Thonke F, Soehendra N. Endoscopic treatment of Mirizzis syndrome. Gastrointest Endosc. 1993;39:532. [ Links ]
3. Csendes A, Díaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989;76:1139. [ Links ]
4. Kwon AH, Inui H. Preoperative diagnosis and efficacy of laparoscopic procedures in the treatment of Mirizzi syndrome. J Am Coll Surg. 2007;204:409. [ Links ]
*Corresponding author
E-mail address: nuno_veloso@hotmail.com (N. Veloso).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Received 13 September 2013; accepted 24 September 2014














