Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.21 no.5 Lisboa out. 2014
https://doi.org/10.1016/j.jpg.2014.03.002
ENDOSCOPIC SPOT
Ileocecal neoformation in a Human Immunodeficiency Virus positive patient
Neoformação ileocecal em doente Vírus da Imunodeficiência Humana positivo
Ricardo Küttner Magalhãesa,∗, Fernanda Reisb, Isabel Pedrotoa
a Department of Gastroenterology, Hospital Santo António, Centro Hospitalar do Porto, Portugal
b Department of Radiology, Hospital Santo António, Centro Hospitalar do Porto, Portugal
*Corresponding author
Patients infected with the Human Immunodeficiency Virus (HIV) have an increased risk of developing cancer, of which 10% are Non-Hodgkin Lymphomas (NHL).1,2
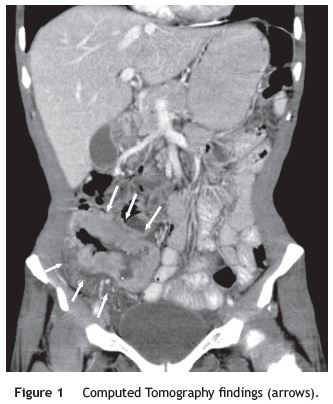
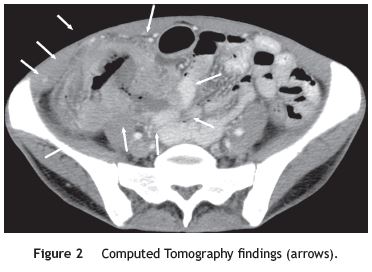
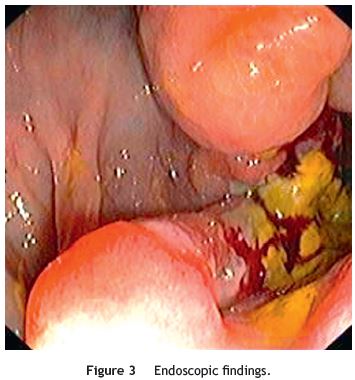
We report a case of a 46-year-old female with pulmonary tuberculosis three years before, currently with stage C3 AIDS with a CD4+ lymphocytes count of 122. She attended the Hospital because of abdominal pain in the right lower abdominal quadrant, 4-5 liquid stools/day with dark blood, weight loss (7 kg), asthenia and anorexia in the last 3 months. Evening fever was reported in the previous 5 days. She was hemodynamically stable. There was no palpable adenopathy, but the presence of a tender mass in the right lower abdominal quadrant was noted. She had relative neutrophilia and CRP elevation (133 mg/L). CMV and EBV IgG antibodies were positive and IgM antibodies were negative. Abdomen ultrasound and Computed Tomography showed thickening of the terminal ileum and part of the ascending colon, with abnormal parietal enhancement, fat densification, a small area of focal wall necrosis and an adjacent adenopathy (Figs. 1 and 2). Both exams suggested tuberculosis and less probably lymphoma as possible diagnosis. Colonoscopy showed an ileocecal ulcerated neoformation (Figs. 3 and 4). Histology revealed diffuse B large cells NHL. It was an IIE/B stage with normal LDH and chemotherapy with cyclophosphamide, adriamycin, vincristine and prednisolone was started.

The gastrointestinal tract is the most common location of extra nodal NHL, associated with HIV. Lymphomas are late events during HIV infection, with the following associated risk factors: low CD4 + lymphocytes count, high viral load, advanced age, EBV infection and presence of AIDS-defining conditions.2-4 It is important to equate this diagnosis in HIV positive patients with these features.
References
1. Bonnet F, Chêne G. Evolving epidemiology of malignancies in HIV. Curr Opin Oncol. 2008;20:534-40. [ Links ]
2. Heise W. GI-lymphomas in immunosuppressed patients (organ transplantation; HIV). Best Pract Res Clin Gastroenterol. 2010;24:57-69. [ Links ]
3. Ho-Yen C, Chang F, van der Walt J, Lucas S. Gastrointestinal malignancies in HIV-infected or immunosuppressed patients. Adv Anat Pathol. 2007;14(6):431-43. [ Links ]
4. Srinivasan S, Takeshita K, Holkova B, Czuczman MS, Miller K, Bernstein ZP, et al. Clinical characteristics of gastrointestinal lymphomas associated with AIDS (GI-ARL) and the impact of HAART. HIV Clin Trials. 2004;5:140-5. [ Links ]
*Corresponding author
E-mail address: rkuttner@gmail.com (R.K. Magalhães).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 13 January 2014; accepted 29 March 2014














