Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Medicina Geral e Familiar
versão impressa ISSN 2182-5173
Rev Port Med Geral Fam vol.31 no.1 Lisboa fev. 2015
ESTUDOS ORIGINAIS
Anxiety and depression in Portuguese patients with chronic obstructive pulmonary disease: a multicentre cross-sectional study
Ansiedade e depressão em pacientes Portugueses com doença pulmonar obstrutiva crónica: um estudo multicêntrico, transversal
Cristina Jácome, MSc,* Alda Marques, PhD,** Raquel Gabriel, MSc,*** Joana Cruz, MSc,**** Daniela Figueiredo, PhD*****
*School of Health Sciences, University of Aveiro (ESSUA), Aveiro, Portugal
**School of Health Sciences, University of Aveiro (ESSUA), Aveiro, Portugal. Unidade de Investigação e Formação sobre Adultos e Idosos (UNIFAI), Porto, Portugal
***Department of Health Sciences, University of Aveiro (SACS), Aveiro, Portugal
****School of Health Sciences, University of Aveiro (ESSUA), Aveiro, Portugal. Department of Health Sciences, University of Aveiro (SACS), Aveiro, Portugal
*****School of Health Sciences, University of Aveiro (ESSUA), Aveiro, Portugal. Unidade de Investigação e Formação sobre Adultos e Idosos (UNIFAI), Porto, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Objectives: To assess symptoms of anxiety and depression among Portuguese patients with chronic obstructive pulmonary disease (COPD) and associated predictive factors.
Study design: A multicentre, cross-sectional study.
Setting: Three primary care centres and one district hospital in the central region of Portugal.
Participants: 302 Portuguese outpatients with COPD.
Methods: Symptoms of anxiety and depression were assessed with the Hospital Anxiety and Depression Scale (HADS). Scores ≥8 were considered clinically significant.
Results: This sample of patients had a mean age of 67±12 years and 41% were female. COPD was graded as mild in 106 (35.1%), moderate in 106 (35.1%) and severe-to-very-severe 90 patients (29.8%). Clinically significant anxiety was found in 53.3% of patients and symptoms of depression in 45.4%. Symptoms of anxiety were associated with limitation of activities (OR 1.39, 95% CI 1.04-1.84), age (0.97, 95% CI 0.94-0.99) and female gender (OR 0.37; 95% CI 0.20-0.66). Symptoms of depression were associated with functional mobility (OR 1.91, 95% CI 1.38-2.66) and limitation of activities (OR 1.12, 95% CI 1.04-1.21).
Conclusions: A high proportion of Portuguese patients with COPD experience symptoms of anxiety and depression. National pulmonary rehabilitation programmes might need to include collaborative self-management interventions to address patients emotional needs.
Keywords: Chronic Obstructive Pulmonary Disease; Anxiety; Depression.
RESUMO
Objetivos: Avaliar sintomas de ansiedade e depressão em pacientes Portugueses com doença pulmonar obstrutiva crónica (DPOC) e fatores preditores associados.
Tipo de estudo: Estudo multicêntrico, transversal.
Local: Três centros de saúde e um hospital distrital da região centro de Portugal.
População: 302 pacientes com DPOC.
Métodos: Os sintomas de ansiedade e depressão foram avaliados através da Escala de Ansiedade e Depressão (HADS). Pontuações ≥8 foram consideradas clinicamente significativas.
Resultados: Esta amostra de pacientes tinham em média de 67±12 anos de idade e 41,1% era do género feminino. A DPOC era de grau ligeiro em 106 (35,1%) pacientes, moderado em 106 (35,1%) e grave-a-muito-grave em 90 (29,8%). Sintomas de ansiedade clinicamente significativos estavam presentes em 53,3% dos pacientes e sintomas de depressão em 45,4%. Os sintomas de ansiedade estavam associados a limitação nas atividades (OR 1,39, 95% CI 1,04-1,84), idade (0,97, 95% CI 0,94-0,99) e género feminino (OR 0,37; 95% CI 0,20-0,66). Os sintomas de depressão estavam associados à mobilidade funcional (OR 1,91, 95% CI 1,38-2,66) e a limitação nas atividades (OR 1,12, 95% CI 1,04-1,21).
Conclusão: Uma elevada proporção de pacientes com DPOC experiencia sintomas de ansiedade e depressão. Os programas nacionais de reabilitação respiratória deveriam incluir intervenções colaborativas de autogestão que respondam a estas necessidades emocionais.
Palavras-chave: Doença Pulmonar Obstrutiva Crónica; Ansiedade; Depressão.
Introduction
Chronic obstructive pulmonary disease (COPD) affects 210 million people worldwide. It is projected to be the seventh leading cause of years lived with disability by 2030.1-2 In Portugal, the prevalence of COPD is 14.2% in the population above 45 years of age. It is estimated that 800,000 citizens live with COPD.3 COPD is characterised by persistent limitation of airflow that is usually progressive. Exacerbations and comorbidities can cause a highly incapacitating disease.4
Anxiety and depression are common symptoms in patients with COPD. This may have a detrimental effect on quality of life and well-being as these symptoms can affect emotional, social and physical functioning.5 There is a complex interaction between anxiety and breathlessness that often exists as a vicious cycle of worsening symptoms.6
In studies conducted in the United Kingdom, Denmark, Canada and New Zealand, 50% to 74% of patients with COPD presented symptoms of anxiety and 28% to 80% symptoms of depression.7-10 In recent systematic reviews, lower prevalences have been reported, with 10-55%11 of patients showing symptoms of anxiety and 7-46%12 depression. In Portugal, the prevalence of symptoms of anxiety and depression in patients with COPD is unknown. One retrospective study, of the impact of comorbidities in outcomes of respiratory rehabilitation, reported that 21.1% (n=24) of patients with COPD had anxiety or depression.13
The current study aimed to assess symptoms of anxiety and depression among Portuguese patients with COPD and to identify associated factors.
Methods
Study design
A multicentre, cross-sectional study of Portuguese outpatients with COPD was conducted in the central region of Portugal between December 2010 and December 2012. The study received Institutional Ethics Committee approval. The reporting of this study conforms to the STROBE statement.14
Participants
The sample was recruited from three primary care centres and one district hospital. The clinicians of these institutions identified patients for the study. They ensured that patients met the criteria for eligibility. Inclusion criteria included a diagnosis of COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria,4 age ≥ 18 years old, the ability to understand the purpose of the study and to give vo-luntarily consent to participate. Exclusion criteria were the presence of severe psychiatric conditions or the inability to understand and co-operate.
Eligible patients were contacted by telephone. The researchers explained the purpose of the study and asked about their willingness to participate. If they agreed to participate, an appointment was scheduled at the patients primary care clinic or hospital. Before data collection, more detailed information about the study was provided to the patient and written informed consent was obtained.
Data collection procedures
Socio-demographic data (age, gender, educational level, marital status and occupation) and clinical data (body mass index (BMI), comorbidities, medication) were recorded first. Lung function and functional mobility were then assessed. Lastly, limitation of activities resulting from breathlessness and symptoms of anxiety and depression were assessed.
Measures
Lung function
Spirometry, using a portable spirometer (MicroLab 3500, CareFusion, Kent, UK), was performed according to the American Thoracic Society/European Respiratory Society Task Force standards for lung function tes-ting.15 The classification of the severity COPD was made in accordance with the GOLD criteria.4
Functional mobility
The Timed Up and Go (TUG) test was used as a test of functional mobility. This test is often used in patients with COPD.16-17 It requires the patient to rise from a standard chair, walk 3 meters, turn around, walk back to the chair, and sit down, after the command go.18 Patients were instructed to walk quickly, but as safely as possible. Two TUG tests were performed and the best performance was considered.
Limitation of activities resulting from breathlessness
The Modified British Medical Research Council questionnaire (mMRC) was used to assess symptoms in patients with COPD, as recommended by GOLD.4 Patients reported their limitation of activities resulting from breathlessness by selecting the statement that best described their limitation.19 The questionnaire comprises five grades (statements) on a scale from 0 to 4, with higher grades indicating greater perceived respiratory limitation.
Symptoms of anxiety and depression
The Portuguese version of the Hospital Anxiety and Depression Scale (HADS) was used to assess symptoms of anxiety and depression.20 This scale has been widely used in patients with COPD and has been reported internationally as a valid and reliable instrument.21 The HADS contains 14 items. Seven items measure symptoms of anxiety (HADS-A) and 7 symptoms of depression (HADS-D).22 The presence of clinically significant symptoms of anxiety or depression was defined by a HADS-A/HADS-D score of ≥ 8.21 The severity of symptoms of anxiety or depression was categorised as mild (score 8-10), moderate (score 11-14) or severe (score 15-21).20 Coefficients of Cronbachs alpha found in the present study (0.78 for anxiety and 0.74 for depression) were similar to those reported by Pais-Ribeiro et al (0.76 and 0.81, respectively).20
Statistical analysis
Descriptive statistics were used to describe the socio-demographic variables, clinical characteristics, and the HADS-A/HADS-D scores. As most of the previous stu-dies of symptoms of anxiety and depression in COPD used point prevalence, the frequency of symptoms of anxiety and depression (HADS-A/HADS-D≥8) was computed based on this estimation. This facilitated the discussion of results. Frequencies were presented together with the 95% confidence intervals. The severity of symptoms of anxiety and depression was categorised as mild (HADS-A/HADS-D ≥8 and ≤10), moderate (HADS-A/HADS-D ≥11 and ≤14) or severe (HADS-A/HADS-D ≥15 and ≤21).20 To explore associations between variables related to the presence of clinically significant symptoms of anxiety and depression, variables of patients with and without symptoms of anxiety and depression (HADS-A/HADS-D≥8 compared to HADS-A/HADS-D<8) were compared using independent t-tests for normally distributed data, Mann-Whitney U-tests for non-normally distributed data and ordinal data, and Chi-square tests for categorical data. In the case of chi-square tests, when a statistically significant difference was found for a categorical variable with more than two categories, chi-square multiple comparison tests with Bonferroni correction were performed to explore which categories differed from each other. The variables that were statistically different (p<0.05) between the two groups were used to further explore their relationship with the severity of anxiety and depression and to perform two multivariate logistic regressions (Enter method). The dependent variable in each multivariate logistic regression was the presence of clinically significant symptoms of anxiety symptoms or depression (0 = absent, 1 = present). Multiple logistic regression analysis was used for predictive purposes and to adjust for possible confounders.23 The level of significance considered was 0.05. Statistical analyses were performed using IBM SPSS Statistics version 20.0 (IBM Corporation, Armonk, NY, USA).
Results
Characteristics of participants
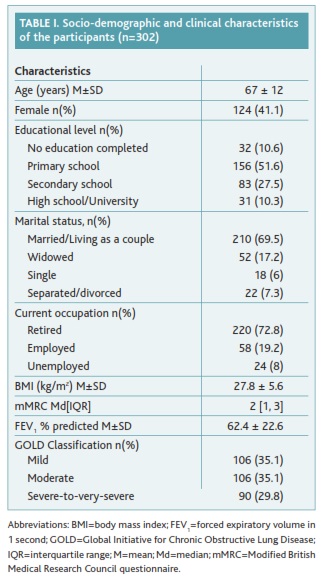
The total number of patients initially screened at the participating institutions was not possible to obtain due to the recruitment strategy. A total of 340 patients with COPD were approached by the research team for inclusion in the study, however 32 refused to participate due to personal reasons and 6 failed to attend the arranged meeting. The final sample comprised 302 patients with COPD (mean age 67±12 years old; 41.1% female). The majority of participants had completed primary school (n=156; 51.6%) and were retired (n=220; 72.8%). The mean BMI was 27.8±5.6kg/m2 and the median mMRC grade was 2 (I walk slower than people of the same age on the level because of the breathlessness, or I have to stop for breath when walking on my own pace on the level). According to the GOLD criteria, 106 (35.1%) patients had mild, 106 (35.1%) mode-rate and 90 (29.8%) had severe-to-very-severe COPD. Table I shows the socio-demographic and clinical cha-racteristics of the study participants.
Symptoms of anxiety and depression
The mean anxiety score was 8.1±4.4 and the mean depression score was 7.3±4. A total of 161 (53.3%; 95% CI 48-58.9) patients had clinically significant symptoms of anxiety. Symptoms of anxiety were experienced mainly as mild (n=74; 46%, 95% CI 38.5-53.4) or moderate (n=59; 36.6%, 95% CI 29.2-44.7) with few severe cases (n=28; 17.4%, 95% CI 11.8-23.6). Clinically significant symptoms of depression were present in 45.4% (95% CI 40.1-50.7, n=137) of patients. These symptoms were experienced as mild in the majority of the sample (n=74; 54%, 95% CI 46-62.8), but also moderate (n=48; 35%, 95% CI 27-43.1) and a few severe cases were found (n=15; 11%, 95% CI 5.8-16.1). A total of 99 (32.8%, 95% CI 27.5-38.1) patients had both symptoms of anxiety and depression.
Associations between anxiety and depression and socio-demographic characteristics
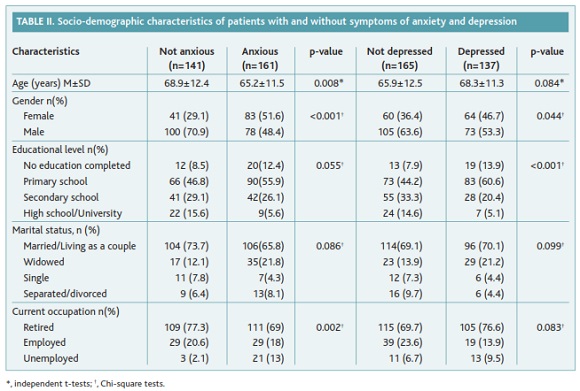
Symptoms of anxiety and depression were more frequent in female patients (p<0.001 and p=0.044) (table II). Symptoms of anxiety were also more frequent in younger patients (p=0.008) and unemployed patients (p=0.002). Symptoms of depression were more frequent in those with lower educational levels (no education completed, primary school and secondary school; p<0.001) (table II). Regarding the association of gender and severity of anxiety, it was found that the frequency of females with moderate and severe anxiety (66.1% and 67.9%, respectively) was significantly higher than females with mild anxiety (33.8%, p<0.001). No other statistically significant differences were found.
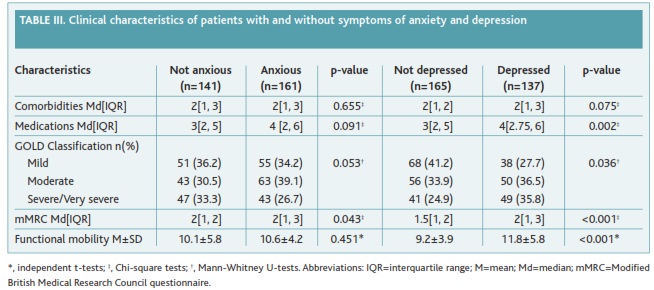
Relationship between symptoms of anxiety and depression and clinical characteristics
The frequency of symptoms of anxiety and depression was higher in patients with greater limitation of activities resulting from breathlessness (mMRC, p=0.043 and p<0.001) (table III). The frequency of symptoms of depression was also higher in patients with higher medication intake (p=0.002), advanced COPD (p=0.036) and lower functional mobility (p<0.001) (table III). Limitation of activities resulting from breathlessness was higher in patients with moderate or severe anxiety (Median 2, Interquartile range (1,3); 2(2,3)) and depression (3(2,3); 3(1.5,3)) than in those with mild anxiety (2(1,2), p=0.026) and depression (2(1,3), p=0.016). No other statistically significant differences were observed regar-ding the severity of symptoms.
Predictors of anxiety and depression
Two multivariate logistic regressions were performed to identify the predictors of symptoms of anxiety and depression. Symptoms of anxiety were predicted by limitation of activities resulting from breathlessness (OR 1.39, 95% CI 1.04-1.84), age (0.97, 95% CI 0.94-0.99), and female gender (OR 0.37; 95% CI 0.20-0.66). Symptoms of depression were predicted by functional mobility (OR 1.91, 95% CI 1.38-2.66) and limitation of activities (OR 1.12, 95% CI 1.04-1.21). These logistic regression models predicted 13% of the total variance of anxiety and 22.4% of the total variance of symptoms of depression.
Discussion
This study showed that a large proportion of Portuguese patients with COPD present symptoms of anxiety and depression. Limitation of activities resulting from breathlessness, female gender, age and functional mobility were predictors of these distressing symptoms.
More than half of patients had symptoms of anxiety (53.3%) and 45.4% had symptoms of depression. This is higher than the value reported by Carreiro (21.1%).13 The proportions found in the present study fall within the range of estimates found among patients with COPD in other countries.7-12 Comparisons need to be interpreted with caution as different instruments were used in other studies.
The presence of symptoms of both anxiety and depression was predicted by limitation of activities resulting from breathlessness. The severity of anxiety and depression was also related to the severity of breathlessness. Respiratory symptoms have been associated with patients anxiety and depression.8 The frequency of symptoms of anxiety was similar in early and advanced COPD. The results strengthen previous findings stating that even at earlier stages of the disease, the uncertain and unpredictable nature of the symptoms and acute exacerbations have an impact of on patients emotional well-being.24
Anxiety was also predicted by female gender and age. Female gender was related to higher emotional distress, consistent with previously published results.25-26 This may reflect the gender differences already found in the general population.27 A higher frequency of symptoms of anxiety was found in younger and unemployed patients, which has been found previously.25-26,28 These findings are relevant for clinical practice. It can be hypothesised that older patients interpret the occurrence of an illness as an expected late-life stressor.28-29 Low educational levels were associated with a higher frequency of depression. This was expected since having a high educational level has been shown to be an important contributor to enhanced personal internal resources.30
Regarding symptoms of depression, the severity of COPD had a different role. More advanced disease was associated with a higher frequency of symptoms of depression. This might be explained by the role of physical functioning on symptoms of depression.31-32 Patients with advanced COPD experience more physical disa-bility. This was confirmed by the logistic regression analysis, which identified patients functional mobility as a predictor of clinically significant symptoms of depression.
These findings suggest that many patients with COPD suffer from symptoms of anxiety and depression and thus interventions are needed to promote a healthy adjustment to the disease. Pulmonary rehabilitation programmes are recommended to improve the physical and psychological condition of patients with COPD.33-34 According to recent international guidelines, these programmes should include exercise training, education and behavioural change through collaborative self-management interventions.33 In COPD and other chronic diseases, there is evidence that these interventions have a significant positive effect on patients emotional function.35-38 In Portugal, pulmonary rehabilitation programmes are scarce and typically combine exercise training with education.39-40 Patients emotional needs are not often directly addressed. It would be logical to complement national programmes with collaborative self-management interventions, since they may increase instrumental and emotional coping abilities to allow patients to manage the demands of the disease. Collaborative self-management interventions place patients and health professionals in partnership to enhance patients self-efficacy and self-management abilities.33 It remains to be determined if involving the family caregiver in this partnership brings additional benefits to patients.
This study has some limitations. Possible sources of bias were the recruitment strategy using clinicians in the institutions involved and the fact that the sample was recruited from only the central region of Portugal. Future studies containing a larger sample and inclu-ding patients with COPD from other regions of the country would be more representative of the Portuguese population with COPD. A control group of healthy individuals with similar socio-demographic characteristics should also be included in further research to increase the validity of these findings. The use of HADS to assess symptoms of anxiety and depression may have introduced a bias in the study since some authors have recently emphasised that the assumed bi-dimensionality of the HADS may not be appropriate.41-42 However, this instrument was used as a screening tool for symptoms of anxiety and depression and not as an instrument for diagnosis of clinical anxiety or depression. The HADS has shown to be a reliable instrument internationally for measuring emotional distress of patients with COPD. This study focused on the presence of clinically significant symptoms of anxiety and depression (i.e., HADS-A/HADS-D≥8). It may be interes-ting to explore the absolute scores of HADS-A and HADS-D and derive predictive equations. Another limitation of the present study is related to its cross-sectional nature. The frequency of distressing symptoms and the relationships with associated factors could not be established along the progression of the disease. Longitudinal studies following a cohort of patients with COPD would address this issue and identify other predictors of symptoms of anxiety and depression. For ins-tance, the predictive value of alexithymia could be investigated. Recent research found a strong association between this condition and distressing symptoms in patients with COPD.43
Conclusion
A large proportion of Portuguese patients with COPD experience symptoms of anxiety and depression. Limi-tation of activities resulting from breathlessness, female gender, age, and functional mobility were predictors of these distressing symptoms. To address patients emotional needs, national pulmonary rehabilitation programmes should include a collaborative self-management component. Future research could explore the effects of involving family caregivers in these interventions on beneficial outcomes for patients.
REFERENCES
1. World Health Organization. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. Geneva: WHO; 2007. ISBN 9789241563468 [ Links ]
2. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):2011-30. [ Links ]
3. Observatório Nacional das Doenças Respiratórias. Prevenir a doença, acompanhar e reabilitar o doente: relatório de 2013. Lisboa: ONDR; 2013. [ Links ]
4. Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(4):347-65. [ Links ]
5. Wouters EF, Celis MP, Breyer MK, Rutten EP, Graat-Verboom L, Spruit MA. Co-morbid manifestations in COPD. Respir Med: COPD Update. 2007;3(4):135-51. [ Links ]
6. Willgoss TG, Yohannes AM, Goldbart J, Fatoye F. Everything was spiraling out of control: experiences of anxiety in people with chronic obstructive pulmonary disease. Heart Lung. 2012;41(6):562-71. [ Links ]
7. Stage KB, Middelboe T, Pisinger C. Measurement of depression in patients with chronic obstructive pulmonary disease (COPD). Nord J Psychiatry. 2003;57(4):297-301. [ Links ]
8. Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25(12):1209-21. [ Links ]
9. Lacasse Y, Rousseau L, Maltais F. Prevalence of depressive symptoms and depression in patients with severe oxygen-dependent chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2001;21(2):80-6. [ Links ]
10. Dowson C, Laing R, Barraclough R, Town I, Mulder R, Norris K, et al. The use of the Hospital Anxiety and Depression Scale (HADS) in patients with chronic obstructive pulmonary disease: a pilot study. N Z Med J. 2001;114(1141):447-9. [ Links ]
11. Willgoss TG, Yohannes AM. Anxiety disorders in patients with COPD: a systematic review. Respir Care. 2013;58(5):858-66. [ Links ]
12. Zhang MW, Ho RC, Cheung MW, Fu E, Mak A. Prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease: a systematic review, meta-analysis and meta-regression. Gen Hosp Psychiatry. 2011;33(3):217-23. [ Links ]
13. Carreiro A, Santos J, Rodrigues F. Impacto das comorbilidades num programa de reabilitação respiratória em doentes com doença pulmonar obstrutiva crónica (Impact of comorbidities in pulmonary rehabilitation outcomes in patients with COPD). Rev Port Pneumol. 2013;19(3):106-13. [ Links ] Portuguese
14. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-9. [ Links ]
15. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-38. [ Links ]
16. Beauchamp MK, OHoski S, Goldstein RS, Brooks D. Effect of pulmonary rehabilitation on balance in persons with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(9):1460-5. [ Links ]
17. Jácome C, Cruz J, Gabriel R, Figueiredo D, Marques A. Functional balance in older adults with COPD. J Aging Phys Act. 2014;22(3):357-63. [ Links ]
18. Podsiadlo D, Richardson S. The timed Up & Go: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-8. [ Links ]
19. Doherty DE, Belfer MH, Brunton SA, Fromer L, Morris CM, Snader TC. Chronic obstructive pulmonary disease: consensus recommendations for early diagnosis and treatment. J Fam Pract. 2006;55 Suppl 1:S1-8. [ Links ]
20. Pais-Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, Baltar M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol Health Med. 2007;12(2):225-35. [ Links ]
21. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52(2):69-77. [ Links ]
22. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361-70. [ Links ]
23. McIlroy SP, Dynan KB, Lawson JT, Patterson CC, Passmore AP. Moderately elevated plasma homocysteine, methylenetetrahydrofolate reductase genotype, and risk for stroke, vascular dementia, and Alzheimer disease in Northern Ireland. Stroke. 2002;33(10):2351-6. [ Links ]
24. Boyle AH. An integrative review of the impact of COPD on families. South Online J Nurs Res. 2009;9(3):1-12. [ Links ]
25. Karakurt P, Ünsal A. Fatigue, anxiety and depression levels, activities of daily living of patients with chronic obstructive pulmonary disease. Int J Nurs Pract. 2013;19(2):221-31. [ Links ]
26. Lee H, Yoon JY, Kim I, Jeong YH. The effects of personal resources and coping strategies on depression and anxiety in patients with chronic obstructive pulmonary disease. Heart Lung. 2013;42(6):473-9. [ Links ]
27. Altemus M. Sex differences in depression and anxiety disorders: potential biological determinants. Horm Behav. 2006;50(4):534-8. [ Links ]
28. Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24(3):217-23. [ Links ]
29. Balcells E, Gea J, Ferrer J, Serra I, Orozco-Levi M, de Batlle J, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010;8(1):108. [ Links ]
30. Drageset S, Lindström TC. Coping with a possible breast cancer diagnosis: demographic factors and social support. J Adv Nurs. 2005;51(3):217-26. [ Links ]
31. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. ISBN 9780826141927 [ Links ]
32. Ng TP, Niti M, Fones C, Yap KB, Tan WC. Co-morbid association of depression and COPD: a population-based study. Respir Med. 2009;103(6):895-901. [ Links ]
33. Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13-e64. [ Links ]
34. Paz-Díaz H, Montes de Oca M, López JM, Celli BR. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. Am J Phys Med Rehabil. 2007;86(1):30-6. [ Links ]
35. Coventry PA, Bower P, Keyworth C, Kenning C, Knopp J, Garrett C, et al. The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS ONE. 2013;8(4):e60532. [ Links ]
36. Adams SG, Smith PK, Allan PF, Anzueto A, Pugh JA, Cornell JE. Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167(6):551-61. [ Links ]
37. Okamura H, Fukui S, Nagasaka Y, Koike M, Uchitomi Y. Psychoeducational intervention for patients with primary breast cancer and patient satisfaction with information: an exploratory analysis. Breast Cancer Res Treat. 2003;80(3):331-8. [ Links ]
38. Sharif F, Mohebbi S, Tabatabaee HR, Saberi-Firoozi M, Gholamzadeh S. Effects of psycho-educational intervention on health-related quality of life (QOL) of patients with chronic liver disease referring to Shiraz University of Medical Sciences. Health Qual Life Outcomes. 2005;3(1):81. [ Links ]
39. Simão P, Almeida P. Reabilitação respiratória: uma estratégia para a sua implementação. Rev Port Pneumol. 2009;XV Suppl 1:S93-S118. [ Links ]
40. Direcção-Geral da Saúde. Orientações técnicas sobre reabilitação respiratória na doença pulmonar obstrutiva crónica (DPOC): circular informativa nº 40/DSPCD, de 27/10/09. Lisboa: DGS; 2009. [ Links ]
41. Cosco TD, Doyle F, Ward M, McGee H. Latent structure of the Hospital Anxiety and Depression Scale: a 10-year systematic review. J Psychosom Res. 2012;72(3):180-4. [ Links ]
42. Herrmann C. International experiences with the Hospital Anxiety and Depression Scale: a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17-41. [ Links ]
43. Tselebis A, Kosmas E, Bratis D, Moussas G, Karkanias A, Ilias I, et al. Prevalence of alexithymia and its association with anxiety and depression in a sample of Greek chronic obstructive pulmonary disease (COPD) outpatients. Ann Gen Psychiatry. 2010;9:16. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Alda Marques
School of Health Sciences, University of Aveiro
Campus Universitário de Santiago - Agras do Crasto, Edifício 30
3810-193 Aveiro, Portugal
E-mail: amarques@ua.pt
Acknowledgements
The authors would like to acknowledge all institutions and patients involved for their participation in this research.
Declaration of Interest
This work was supported by Portuguese National Funds through FCT - Foundation for Science and Technology (grant number RIPD/CIF/109502/2009). The authors report no conflict of interest.
Recebido em 11-08-2014
Aceite para publicação em 10-12-2014