Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Angiologia e Cirurgia Vascular
versión impresa ISSN 1646-706X
Angiol Cir Vasc vol.16 no.1 Lisboa mar. 2020
ARTIGO ORIGINAL
Endovascular management and outcomes of visceral arterial aneurysms - single centre experience
Abordagem endovascular de aneurismas viscerais - experiência de um centro
Nuno Henriques Coelho1, Jacinta Campos1, Andreia Coelho1, Rita Augusto1, Carolina Semião1, Evelise Pinto1, João Ribeiro1, João Peixoto1, Victor Martins1, Daniel Brandão1, Ricardo Gouveia1, Alexandra Canedo1
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar Vila Nova de Gaia/Espinho
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Over the past decade, endovascular treatment (EVT) is taking over visceral arterial aneurysms treatment considering its effectiveness, safety and minimal invasiveness.
Methods: We retrospectively evaluated our department experience in visceral arterial aneurysms endovascular approach from 2009 to 2019.
Results: From 2009 to 2019, nineteen visceral artery aneurysms were submitted to EVT (mean age 62,5 years, 53% women). The addressed arterial segments were: the splenic artery (52%, n=10) followed by the renal artery (21%, n = 4), the hepatic artery (11%, n = 2), the superior mesenteric artery (11%, n = 2) and the celiac arrtery (5%, n = 1). Average diameter was 26,9 ± 5,4 mm [range 21-39 mm]. The majority were asymptomatic incidental findings (74%). Concomitant aneurysms were found in 3 patients (15,8%). EVT included: stent-graft exclusion (n = 9), aneurysm-sac coil embolization (n = 6), stent-assisted coil embolization (n=2) and segmental artery exclusion (n=2). Median radiological follow-up was 46,8 months [range 1,1-128 months]. Early SMA occlusion was reported in one case after stent-assisted coil embolization, however without ischemic symptoms. End-organ loss was reported in one case (renal artery coil embolization, without overall renal function worsening).
Conclusion: Nowadays, endovascular approach is the first-line intervention for most visceral arterial aneurysms. Although still limited, the reported results are favourable and are in line with the current literature.
Keywords: Visceral Artery Aneurysm; Visceral Artery Pseudoaneurysm; Endovascular Procedures; Embolization; Covered Stent; Outcome Analysis
RESUMO
Introdução: Ao longo da última década, a abordagem endovascular tem assumido um papel preponderante no tratamento dos aneurismas das artérias viscerais (AAVs). Esta mudança de paradigma tem em conta a eficácia, a segurança e o facto de o tratamento endovascular ser menos invasivo quando comparada com a cirurgia clássica. Reportamos a experiência do nosso centro no tratamento endovascular de AAVs.
Métodos: Revimos retrospectivamente os casos de AAVs tratados no nosso centro de 2009 a 2019.
Resultados: De 2009 a 2019, foram tratados dezanove aneurismas viscerais (idade média 62,5 anos, 53% do sexo feminino). Os segmentos arteriais afetados foram: a artéria esplénica (52%, n = 10), a artéria renal (21%, n = 4), a artéria hepática (11%, n = 2), a artéria mesentérica superior (11%, n = 2) e o tronco celíaco (5%, n = 1). O diâmetro aneurismático médio foi de 26,9 ± 5,4 mm [intervalo de 21 a 39 mm].
A maioria dos AAVs corresponderam a achados assintomáticos (74%). Foram encontrados aneurismas concomitantes em 15,8% dos casos. As técnicas endovasculares utilizadas foram as seguintes: exclusão do aneurisma com recurso a stent recoberto (n = 9), embolização do saco aneurismático com coils (n = 6), embolização assistida por stent (n = 2), exclusão segmentar da artéria (n = 2). O tempo médio de follow-up foi de 46,8 meses [intervalo 1,1-128 meses]. Foi constatada oclusão precoce da artéria mesentérica superior em um caso (após embolização assistida por stent), sem sintomatologia de isquemia intestinal. Foi também constatada uma trombose renal após embolização de aneurisma renal com coils, sem agravamento da função renal.
Conclusão: Atualmente, a abordagem endovascular é considerada como tratamento de primeira linha no contexto dos aneurismas viscerais. Ainda que limitada, esta série demonstra resultados favoráveis e em linha com o reportado na literatura.
Palavras-chave: Aneurisma de Artéria Visceral; Pseudoaneurisma de Artéria Visceral; Procedimentos Endovasculares; Embolização; Stents-Recobertos; Resultados; Follow-Up
Introduction
Visceral arterial aneurysms are a rare but clinically important vascular pathology. Of all intra-abdominal aneurysms, only 5% address the visceral vasculature.(1,2) It includes splanchnic territory aneurysms (celiac artery, superior mesenteric artery (SMA), inferior mesenteric artery (IMA) and their branches) and also renal artery aneurysms.(3,4)
Nowadays, visceral arterial aneurysms are more frequently found due to easier access to cross-sectional imaging, increase in surgical and percutaneous interventions and also due to population aging.(1,2,4,5,6) Rupture, reported in H10-20%, is the most devastating complication with mortality ranging from 20 to 100%, depending on aneurysm location (with SMA, gastroduodenal and pancreaticoduodenal being the most lethal).(4) Visceral arterial aneurysms include both true (VATAs) and pseudoaneurysms (VAPSAs) having different underling etiologies. Atherosclerotic degeneration is the most common cause of VATAs. However, multiparity, portal hypertension, connective tissue disorders, vasculitis and rare congenital disorders (such as von Recklinghausens's disease, Ehlers-Danlos type IV, Marfan's syndrome) can also be listed. VAPSAs can be related to abdominal trauma (blunt, penetrating or iatrogenic - abdominal surgery or hepatobiliary instrumentation), intrabdominal inflammatory processes (pancreatitis), infection or vasculitis and have a higher rupture-risk.(1,5) Most non-ruptured VATAs are asymptomatic or present with mild nonspecific symptoms, related aneurysm size and location (with SMA and celiac aneurysms being more symptomatic).(1) Splenic artery is the most common affected (60%), followed by the hepatic (20%), renal (10%), SMA (6%) and celiac arteries (4%).(2,5)
VAPSA treatment is mandatory because of the high risk of rupture.(4) However, the incidental finding of an asymptomatic VATA leaves clinicians with a dilemma. Discriminating which are harmless from those who are high-risk is not always possible.(5) Small clinical series suggest that the risk of rupture depends not only of aneurysm diameter, but also upon VATA's localization, underlining etiology and growth-rate.(2)
With the improvement and refined endovascular armamentarium (smooth detachable micro-coils, flexible sheaths, low-profile flexible stent-grafts, flow-diverting stents), endovascular treatment (EVT) is taking over visceral arterial aneurysms approach, considering its effectiveness, safety and minimal invasiveness.(4)
The objective if this retrospective study was to review the applicability and outcome of different endovascular techniques applied for the treatment of visceral arterial aneurysms.
Materials & methods
Retrospective analysis of all visceral arterial aneurysms submitted to EVT in our Institution from 2009 to 2019. Age, sex, comorbidities, risk factors and aneurysms characteristics (location, VATAs vs VAPSAs, diameter, presentation and etiology) were considered. Furthermore, we evaluated all the interventions with respect to technical success, embolic/occlusive agents used, procedure-related complications and clinical and radiologic follow-up.
Results
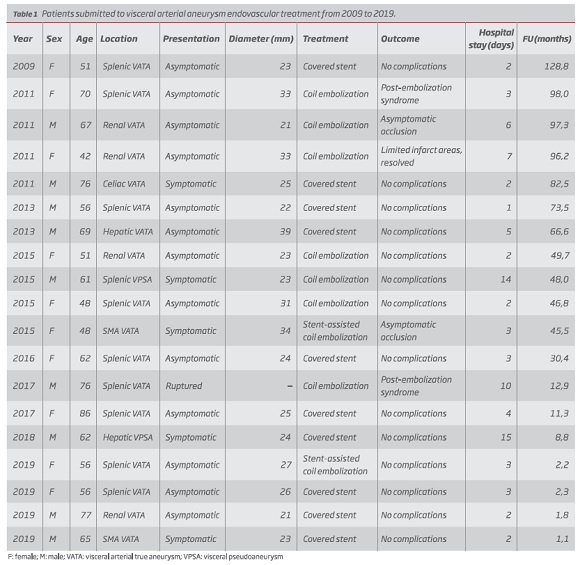
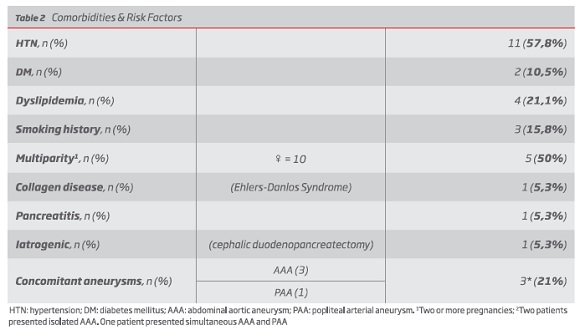
Nineteen patients (17 VATAs and 2 VAPSAs) were submitted to EVT during the reported period (age 62,5 years [range 42-86 years], 52,6% women) (table 1). Comorbidities and possible risk factors can be consulted in table 2. The presumed etiology was degenerative in the majority of patients (n = 16), iatrogenic after surgical procedure (n = 1), connective tissue disease (n = 1) and inflammatory due to adjacent pancreatitis (n = 1). All aneurysms were diagnosed through angioCT. Average aneurysm diameter was 26,9 ± 5,4 mm [range 21-39 mm]. More than a half cases involved the splenic artery (52%, n = 10), followed by the renal arteries (21%, n = 4), the hepatic artery (11%, n = 2), the SMA (11%, n = 2) and the celiac artery (5%, n = 1). The majority of VATAs were asymptomatic (n = 14; 88,4%) with only two patients reporting vague sporadic abdominal pain. Concomitant aneurysms were found in 3 patients (two patients with isolated abdominal aortic aneurysm (AAA) and one patient with concomitant AAA and unilateral popliteal arterial aneurysm).
All procedures were performed under local anesthesia/conscient sedation. EVT included: exclusion with covered stent (n = 9; 5 splenic, 1 renal, 1 celiac and 2 hepatic aneurysms), aneurysm-sac coil embolization (n = 6; 3 splenic and 3 renal aneurysms), stent-assisted coil embolization (n = 2; 1 SMA and 1 splenic aneurysm) and segmental artery exclusion with coils (total n = 2; 1 ruptured splenic VATA and 1 splenic VPSA, emergency setting).
No access-related complications were identified. Immediate technical success was achieved in 100% patients. Two patients had auto-limited post-embolization Syndrome. Mean hospital stay was 3,1 days [range 1-7 days] for elective VATAs and 13 days [range 10-15 days] for urgent cases (2 VAPSAs and one ruptured VATA).
Clinical and radiological follow-up was 46,8 months [range 1,1-128 months]. Early asymptomatic SMA occlusion (day 4) was reported in one case, after stent-assisted coil embolization. End-organ loss during follow-up was reported in one case (renal artery coil embolization, without overall renal function worsening). No mortality or re-interventions were identified.
Discussion
Considering its rarity (estimated prevalence of 0,1 to 2%), visceral arterial aneurysms natural history is still poorly defined.(2) Nowadays, EVT is considered the first-line treatment. Nevertheless, there is a lack of literature that document both EVT effectiveness and long-term outcomes. Therefore, this report encompassing nineteen cases with a considerable follow-up (up to ten years, with a mean of four years) adds an important contribution.
In line with literature, the most frequent suspected etiology was degenerative/atherosclerotic accounting for more than 80% cases. Aneurysms distribution was also in accordance with other reports with splenic artery aneurysms being the more common (53%). Female predominance (70%), as well as multiparity (5 out of 10 women had two or more pregnancies) were particular significant in the splenic territory. Although most of VATAs were asymptomatic, two patients (celiac and SMA aneurysms) reported sporadic vague abdominal discomfort, this being explained by their adjacent neurological structures.(2)
Although it is life-saving to treat a rupture, urgent to treat a pseudoaneurysm and relatively straightforward to intervene on a symptomatic or rapid-growing visceral aneurysm, asymptomatic incidental true VATAs remain a dilemma. Hindered by the lack of prospective studies that evaluate their natural history, diameter criteria for intervention remain unclear. The European Society for Vascular and Endovascular Surgery propose that intervention should be considered for asymptomatic splanchnic aneurysms of e 25 mm diameter (Class IIb, level C evidence).(7) On the other hand, a recent draft (not yet published) from the Society for Vascular Surgery, suggests 20 mm as cut-off for the majority of asymptomatic VATAs.(3) The decision to treat or not to treat an asymptomatic VATA should lead clinicians to consider not only the size but also its location, suspected etiology, patient's comorbidities and preferences, local expertise, anticipated difficulties and eventual procedure-related complications. In this study, all patients had VATAs with e 20 mm size. We included one ruptured splenic aneurysm. However, as no previous image was available, and once is difficult to retrospectively estimate a ruptured aneurysm diameter, we decided not to include it in the diameter report.
Visceral territory presents several singularities: tortuous and spasm/dissection-prone vessels; bowel and diaphragmatic movements; difficult trackability, pushability, crossability and steerability; difficult and unfavorable approach angles; need for side branches preservation. However, with a flexible sheath, an angled catheter, a hydrophilic microcatheter (triaxial technique) frequently it is not only possible to exclude the aneurysm but also to preserve afferent arteries, with favorable long-term outcomes.(4)
In the first reports, coil embolization was the mainstay of treatment, considering the numerous feeding collaterals that assure the splanchnic circulation. Nevertheless, up to 40% of patients submitted to coil embolization can have ischemic complications.(4) Therefore, flexible and low profile stent grafts have gained its momentum in the visceral territory(9). They have the advantage of aneurysms exclusion while maintaining direct antegrade arterial flow. We used stent-grafts in nine cases. During follow-up (50,3 months [range 1,1-128,8 months] no complications were reported, even in those having almost a decade of follow-up. After treatment, 6-months dual antiplatelet therapy (acetylsalicylic acid and clopidogrel) was prescribed for all the patients treated with covered-stents. Although we did not used any flow diverter stent, they are more and more used to treat aneurysms with very large neck or those with insufficient landing-zone(4). Flow diverters keep the side branches patent and may allow treatment of renal or superior mesenteric artery aneurysms that once were considered unsuitable for EVT.
Following endovascular intervention, periodic surveillance with appropriate imaging studies is advisable to identify endoleaks or continued aneurysm perfusion. In our Institution we perform 1 month and 6 months control CTA. Without negative clinical or imagiological evolution the interval between CTA control can be extended to 2-3 years. When visceral arterial axis can be accurately accessed, we use duplex-ultrasound (DUS), thus decreasing patient radiation and contrast exposure. DUS or magnetic resonance are also alternatives when coils artifact is a limitation. The identification of synchronous or metachronous aneurysms addressing other arterial territories should also be focused. We found a 15,7% prevalence of synchronous aneurysms, in line with other series.
Conclusion
Although limited this retrospective review show good long-term outcomes after endovascular treatment of visceral arterial aneurysm. EVT represents a safe and effective option, associated with less burden of morbidity and shorter hospital stay, when compared to open surgery. However, there is still a lack of clinical evidence and consensus in both timing and technique, especially for asymptomatic VATAs treatment.
REFERENCES
1. Hosn, M. A. et al. Visceral Artery Aneurysms : Decision Making and Treatment Options in the New Era of Minimally Invasive and Endovascular Surgery. [ Links ]
2. Pitton, M. B. et al. Visceral artery aneurysms : Incidence , management , and outcome analysis in a tertiary care center over one decade. (2015). DOI: 10.1007/s00330-015-3599-1 [ Links ]
3. Rabih A. Chaer, MD, Christopher J. Abularrage, MD, Dawn M. Coleman, MD, Mohammad H. Eslami, MD, Vikram S. Kashyap, MD, Caron Rockman, MD, M. Hassan Murad, M. The Society for Vascular Surgery Clinical Practice Guidelines on the Management of Visceral Aneurysms (DRAFT). (2019).
4. Loffroy, R. et al. World Journal of Radiology © 2015. 7, (2015). [ Links ]
5. Wojtaszek, B. M. Managing Visceral Artery Aneurysms. (2013). [ Links ]
6. Regus, S. & Lang, W. Rupture Risk and Etiology of Visceral Artery Aneurysms and Pseudoaneurysms : A Single-Center Experience. 50, 10-15 (2016). [ Links ]
7. Committee, W. et al. Editor ’ s Choice e Management of the Diseases of Mesenteric Arteries and Veins Clinical Practice Guidelines of the European Society of Vascular Surgery ( ESVS ). 460-510 (2017). DOI: 10.1016/j.ejvs.2017.01.010
8. Song, C., Dong, J., Yu, G., Zhou, J. & Xiang, F. Comparison of open surgery and endovascular procedures as a therapeutic choice for visceral artery aneurysms. (2017). DOI: 10.1177/1708538117744102 [ Links ]
9. Venturini, M. et al. Endovascular Repair of 40 Visceral Artery Aneurysms and Pseudoaneurysms with the Viabahn Stent-Graft : Technical Aspects , Clinical Outcome and Mid-Term Patency. 385-397 (2018). DOI: 10.1007/s00270-017-1844-5 [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: nunoc.90@gmail.com (N. Coelho).
Recebido a 14 de junho de 2019
Aceite a 14 de março de 2020