Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Angiologia e Cirurgia Vascular
versión impresa ISSN 1646-706X
Angiol Cir Vasc vol.16 no.1 Lisboa mar. 2020
ARTIGO ORIGINAL
Retrograde approach: going further in endovascular techniques dedicated to critical limb ischemia
Punção retrógrada: uma técnica endovascular alternativa dedicada à isquemia crítica
Rita Augusto1,2, Jacinta Campos1,2, Andreia Coelho1,2, Nuno Coelho1,2, Evelise Pinto1, Carolina Semião1,2, João Ribeiro1, João Peixoto1, Daniel Brandão1,2, Alexandra Canedo1,2
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
2 Unidade de Angiologia e Cirurgia Vascular da Faculdade de Medicina da Universidade do Porto, Porto, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Endovascular techniques have been revolutionizing the revascularization of patients with chronic limb threatening ischemia (CLTI), showing consistently high limb salvage rates. However, endovascular recanalization of infrapopliteal occlusive disease can be technically demanding and the failure rate for these types of lesions is about 20%. In that case, an alternative vascular access may be required. We report our experience concerning CLTI patients who underwent retrograde access and recanalization of chronic occlusions after failure of anterograde attempts.
Methods: Retrospective institutional review of consecutive patients requiring retrograde punctures to obtain endovascular revascularization (2013-2018) - 51 limbs in 50 patients. The primary outcome was to evaluate the technical success and the limb salvage - major-amputation free survival. The secondary outcomes were the rate of major and minor amputation, the global survival of this population and the characterization of the population and the endovascular procedures performed.
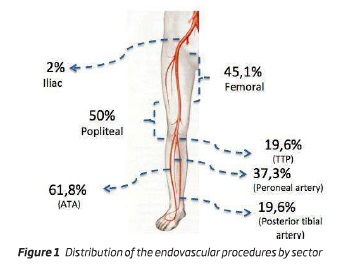
Results and conclusion: The technical success was achieved in 76,5% of the procedures. The major amputation free-survival rate was 81,4% at 6 months. The femoro-popliteal and distal territories were concomitantly treated in 63,3% of the procedures and isolated distal territory was treated in 32,7%. Femoral approach was always initially performed (90,2% anterograde). Direct revascularization according to the angiosome concept was obtained in 64,6% of the cases. Anterior tibial artery was punctured in 33,3% of cases followed by pedal artery (27,5%), peroneal artery (19,6%), common plantar artery (7,8%), posterial tibial artery above the ankle (3,9%), supra-articular popliteal artery (3,9%), lateral plantar artery (2%) and metatarsal artery (2%). Percutaneous transluminal angioplasty (PTA) was performed in 69,4% of the procedures (2% with Drug Elluting Balloons) and PTA and stenting in 28,6%. During follow-up 19,4% of patients were submitted to major amputation and 29,4% to minor amputation. The rate of healing at 6 months was 43,3%.
The results of the retrograde access and recanalization of chronic occlusions are comparable to data reported in the literature, confirming it as a valuable alternative. As so, the retrograde access approach for revascularization of CLTI patients appears to be a safe and effective alternative that expands revascularization options after the failure of a conventional endovascular anterograde approach, allowing the salvaging a greater number of limbs, particularly in patients with significant co-morbidities.
Keywords: Diabetic Foot; Endovascular procedures; Stent; Angioplasty; Limb salvage; Amputation
RESUMO
Introdução: A revascularização endovascular tem revolucionado a revascularização dos doentes com isquemia crónica ameaçadora de membro, demonstrando consistentemente maiores taxas de salvamento de membro. Contudo, a taxa de insucesso na repermeabilização endovascular anterógrada em oclusões infra-poplíteas ronda os 20%. Deste modo, as técnicas de abordagem retrógrada surgem como alternativa crescente na tentativa de revascularização eficaz do membro com o intuito de salvar o mesmo. Neste contexto, os autores propõem-se apresentar a série do respetivo serviço relativa a esta técnica, salientando, entre outros aspetos, a sua eficácia e segurança.
Material e métodos: Estudo retrospetivo dos doentes com isquemia crónica ameaçadora de membro submetidos a punção retrógrada para repermeabilização de eixos arteriais (2013-2018) - 51 membros em 50 doentes, O objetivo primário é avaliar o sucesso técnico e a taxa de sobrevida livre de amputação-major. Como objetivos secundários os autores pretendem descrever as taxas de amputação major e amputação minor, a sobrevida global e os tratamentos endovasculares efetuados.
Resultados e conclusão: O sucesso técnico foi alcançado em 76,5% dos procedimentos. A sobrevida livre de amputação major aos 6 meses foi de 81,4% . O setor femoro-poplíteo e distal foi tratado concomitantemente em 63,3% dos casos e somente o sector distal em 32,7%. A punção femoral foi sempre efetuada inicialmente (anterógrada em 90,2% dos casos). A revascularização angiossómica foi obtida em 64,6% dos casos. A artéria tibial anterior foi a artéria maioritariamente puncionada (33,3%), seguida pela artéria pediosa (27,5%), artéria peroneal (19,6%), artéria plantar comum (7,8%), artéria tibial posterior (3,9%), artéria popliteal supra-articular (3,9%), artéria plantar lateral (2%) e artéria metatársica (2%). Angioplastia transluminal percutânea (ATP) foi efetuada em 69,4% dos casos (2% com Drug Elluting Balloons) e ATP com stenting em 28,6%. Durante o follow-up, 19,4% dos doentes foram submetidos a amputação major e 29,4% a amputação minor. A taxa de cicatrização aos 6 meses foi de 43,3%.
Os resultados da abordagem endovascular por punção retrógrada com recanalização de oclusões crónicas assumem uma tendência semelhante aos dados reportados na literatura, assumindo-se esta técnica como uma alternativa eficaz e segura quando a via anterógrada não é tecnicamente exequível, aumentando o sucesso na revascularização de doentes com isquemia crítica possibilitando, assim, a preservação de um maior número de membros.
Palavras-chave: Pé Diabético; Revascularização endovascular; Stent; Angioplastia; Salvamento de membro; Amputação
Introduction
Limb revascularization in chronic limb threatening ischemia (CLTI) is a main topic concerning the Vascular Surgery community. However, there is still a lack of high-level evidence regarding the optimal treatment strategy. The UK National Institute of Health Research, Health Technology Assessment funded Bypass versus Angioplasty for Severe Ischaemia of the Limb (BASIL) trial remains the only randomised controlled trial (RCT) to have compared a "bypass surgery first" with a "plain balloon angioplasty (PBA) first" strategy for CLTI resulting from infra-inguinal disease.(1) In patients who were likely to survive for 2 years and had a suitable vein, primary bypass (PB) was associated with better clinical outcomes. Furthermore, PBA was associated with a high technical and clinical failure rate. Still, the endovascular treatment of patients with CLTI has progressed dramatically in recent years as a result of advances in endovascular techniques and equipment.(2) As a result, vein bypass is increasingly being viewed as a secondary, salvage procedure to be performed when all endovascular revascularization options have been exhausted. (Joels, C.S, Goodney, P.P).(3,4)
The ongoing randomized BEST-CLI and BASIL-2 trials will provide high-quality evidence about the treatment of limb-threatening ischemia, but their results will only be applicable in a minority of patients, namely in those who are candidates for both endovascular and surgical revascularization.
A key step for a successful endovascular intervention is arterial access. The standard approach to an endovascular revascularization is an antegrade approach, defined as accessing preferably ipsilateral or contralateral femoral artery, and crossing the lesion(s) in an antegrade way. Once it is crossed, a variety of modalities are available for treatment including balloon angioplasty, stent placement and/or atherectomy. However, in up to 20% of cases tibial lesions cannot be crossed in an antegrade direction.(5)
There are several reasons for failure of the antegrade approach such as: the absence of an arterial "stump" at the beginning of the chronic total occlusion (CTO); failure to create a subintimal channel due to extreme calcification; inability to re-enter the true lumen after subintimal recanalization; the presence of arterial bifurcations/important collaterals near the occlusion; complications such as perforation.(6,7)
When the antegrade approach fails, an alternative endovascular strategy can be used: access the vessel distal to the lesion and cross the obstruction in a retrograde fashion. The retrograde approach uses a distal arterial access site that ranges from the distal superficial femoral artery to the very distal arteries of the foot. The first description of a retrograde approach for crossing a tibial lesion was in a 1990 report by Iyer et al.(8) A percutaneous technique with a combined antegrade-retrograde approach to establish through-and-through wire access (i.e. the SAFARI technique - Subintimal Arterial Flossing with Antegrade-Retrograde Intervention) was later described in detail by Spinosa et al(9), with good results - technical success rates of recanalization improved to > 90%. In recent years, the retrograde tibiopedal approach is increasingly being used for revascularization of complex CTOs of infrainguinal arteries. Manzi and Palena have expanded the utility of tibiopedal access and interventions with the description of retrograde transmetatarsal or transplantar arch access.(10,11)
Accordingly, the authors intend to describe the experience of their Vascular Surgery Department on retrograde endovascular revascularization for the treatment of CLTI patients.
Methods
Retrospective institutional review of consecutive patients with CLTI requiring retrograde punctures to obtain endovascular revascularization (January 2013-December 2018). The authors evaluated demographics and co-morbidities data. The primary outcome was to evaluate the technical success and the limb salvage. The secondary outcomes were the rate of major and minor amputation, the global survival of this population and the characterization of the population and the endovascular procedures performed. Major amputation was defined as amputation proximal to the ankle joint whilst minor amputation was defined as amputation distal to the ankle joint. Operative reports were also reviewed to analyze the endovascular procedures and techniques.
Procedure
The retrograde distal approach was made when the anterograde revascularization failed to cross the occlusion and, if it was possible, performed according to the angiosome. Using a 20-gauge needle, under fluoroscopy guidance with proximal injection of contrast medium the arterial access was gained, being an 0.018-inch guide wire then carefully advanced to avoid inadvertent retraction resulting in loss of access. After snaring the guidewire into the catheter placed anterogradely (when necessary with the assistance of the rendez-vous technique), a through-and-through wire access was achieved, and the lesion was treated in an anterograde direction. The hemostasis was achieved at the distal puncture by manual compression and, if needed, with balloon inflation at a low pressure.
Statistical analysis
Categorical variables are presented as frequencies and percentages and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distribution. Analyses were performed with the use of SPSS software, version 22.
Results
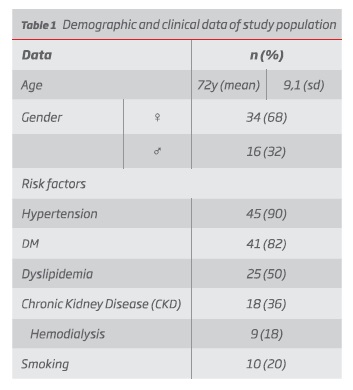
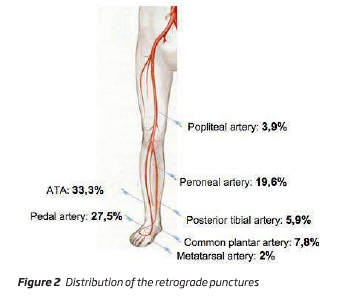
A total of 513 consecutive limbs with CLTI who underwent endovascular revascularization were identified, 51 of whom (10%) were treated using retrograde approach. Demographic data are presented in Table 1.
Isolated rest pain with no ulcer was present in only 3,9% of the patients.
Femoral antegrade approach was always obtained - 90,2% ipsilateral.
The technical success - crossing the lesion, recanalizing the vessel and reaching adequate foot run-off at least in one artery - was achieved in 76,5% of the procedures. Direct angiossomic revascularization was obtained in 64,6% of the cases.
The femoro-popliteal and tibial arteries were revascularized in 63,3% of cases, tibial arteries alone were treated in 32,7% of cases, isolated femoro-popliteal territory was treated in only 2% of the procedures, as well as iliac territory (2%). Figure 1 presents the distribution of the endovascular procedures according to the revascularized territory. Anterior tibial artery (ATA) was punctured in 33,3% of cases followed by pedal artery (27,5%), peroneal artery (19,6%), common plantar artery (7,8%), posterior tibial artery above the ankle (3,9%), supra-articular popliteal artery (3,9%), lateral plantar artery (2%) and metatarsal artery (2%) - Figure 2.
Percutaneous Transluminal Angioplasty (PTA) was performed in 69,4% of the procedures (2% with drug eluting balloon - DEB) and recanalization, PTA and stenting in 28,6%. Tibial arteries stenting was performed in 5,9% of procedures as a bail-out technique.
The median follow-up (FU) time was 7 months (mo), with an interquartile range of 12 mo. During FU, 19,4% of patients were submitted to major amputation and 29,4% to minor amputation.
The major amputation free-survival (AFS) rate at 6 mo was 81,4% and at 12 mo was 76,6% and the rate of healing at 6 mo was 43,3% and at 12 mo was 56,3%. The 6 mo global survival was 66,2%. The median procedure and fluoroscopy times were 146 (IQR 85) and 50 (IQR 21) min, respectively.
The endovascular reintervention rate was 17,6% and the median time was 156 days after the first procedure. Balloon angioplasty was the most common modality used for reintervention - 66,7% of cases.
Discussion
Several strategies have been developed to improve the success rate of recanalizing CTOs, such as subintimal angioplasty, CTO crossing devices and re-entry devices. However, even these techniques may not be successful or feasible. One adjunctive technique to achieve effective recanalization is to obtain a retrograde access, improving the overall technical success rate.(12)
Concerning this technique, Rutger’s systematic review(13) included 19 articles, counting with 3 prospective studies (1905 interventions in 1395 patients). The bellow-the-knee vessels were punctured in 61.3% of cases, being 86.0% of all lesions successfully crossed using a retrograde access with 84.0% technical success.
Spinosa et al(9) were able to demonstrate a 100% technical success rate in crossing the lesion and establishing in-line flow to the foot through retrograde approach. Other series have also shown promising results from a combined retrograde-antegrade strategy, with procedural success rates of 69-86%.(5,14,15)
Kaushal et al(16) describe a cohort of 52 limbs with a 63.5% technical success rate. The limb salvage rate at a mean follow-up of 5.4 months was 78.8%. In their serie, Taha et al(17), described a retrograde approach technique after a failed antegrade recanalization in 47 patients (85% presenting with critical limb ischemia). They achieved an overall technical success in 57% of cases.
Goltz et al(18) recently reported their results of 16 patients with CLTI who underwent retrograde transpedal access after an unsuccessful antegrade approach. Procedural success was 75% and limb salvage rate at 1 year was 73%.
Therefore, the data presented in this study show a similar trend to the literature.
These studies report a satisfactory safety profile for the retrograde access of the popliteal, tibial, or pedal vessels and this is also demonstrated in the present study, where the authors just had local complications such as hematoma, which were minor and self-limited. Other complications that may be related to this technique, described in literature, are arterial perforation or arteriovenous fistula formation, dissection or thrombosis of the vessel.
In their serie, Kaushal et al(16) described 5 complications: 4 hematomas managed conservatively and 1 major retroperitoneal bleed resulting in patient death.
In the Rutger’s systematic review(13) distal access site complications were reported in 4,1% of cases and a prospective trial that looked at tibial and pedal artery access in 197 patients, showed high access and intervention success rates with few minor access site complications (5.6%) and no major complications related to access.(19)
In this study, the authors performed ultradistal punctures - below the ankle - in 19 cases (37,2%). Such distal punctures should be reserved for extreme cases in which other revascularization options are unfeasible or contraindicated.
To assist in gaining access to the distal artery either fluoroscopy or ultrasound can be used. Whereas many surgeons have been using fluoroscopy, according to the literature, a shift to ultrasound-guidance is noticed. Nevertheless fluoroscopy remains a fast and reliable way to guide access.(7) The only multicenter prospective trial on the effectiveness of retrograde tibiopedal access including 197 patients used angiography to guide access in 33.5%, ultrasound in 36.0% and a combination in 29.4% of the cases.(19) The disadvantages of ultrasound-guided puncture in the distal approach might be the edema (that reduces visibility of the small tibiopedal arteries), the heavy calcification (which may cause extensive shadowing) and the depth of the leg arteries (especially anterior tibial and peroneal arteries) that may be difficult to visualize. Additionally, ultrasound-guidance requires a device with high definition as the arteries to be punctured have a diameter that varies between 1,5 and 3 mm. However, ultrasound has advantages over fluoroscopy-guided puncture in chronic kidney disease (which is not too infrequent in patients with CLTI), reducing the contrast medium dosage. Additionally, with an adequate technique, the risks of hematoma or dissection are minimized. Moreover, radiation-exposure to the surgeon and the patient can be reduced.(7) While calcifications are to be avoided in ultrasound-guided access, they can be targeted for fluoroscopy-guided access. Very important for this kind of access is a stable positioning of the foot to avoid movements and to allow for an optimal adjustment of the C-arm to the course of the access arteries.(7)
According to the learning curve of the group, nowadays, the authors perform retrograde recanalization based preferably in an 0,018 inch guide wire (to obtain support to cross the distal cap of the occlusion), without any sheath, low profile catheter or balloon catheter, in order to avoid any trauma that the material may cause inside the distal artery.
There are some limitations to this technique: occlusion or severe luminal disease of the distal artery, complications at the distal artery (dissection, perforation or thrombosis) caused by antegrade revascularization attempts or necrosis/ulcer at the puncture site.
It should also be considered that the results of this technique (patency and AFS) are to be interpreted in light of the context of an aggressive strategy of revascularization in a high-risk cohort of patients: those that failed an attempt of endovascular anterograde recanalization and were not suitable for a surgical bypass.
One further aspect that needs to be considered is the patient’s general condition - that might justify the results of this study concerning the mortality. The most important of the many factors to consider are life expectancy and the presence of co-morbidities, such as DM and CKD. Those are patients with more severe and progresses vascular damage - poor prognosis.(20,21)
In the authors’ department, the follow-up of the revascularized patients is done by clinical observation of the lesions and evaluation of quality of Doppler signal. If there is a deterioration or stagnation of the ulcer healing with worsening of the vascular status, the patient is considered to a secondary endovascular procedure. However, the author’s opinion is that the vessel patency is related to the stage of the disease in the vessel and not to the vessel used for access.
Concerning the optimal medical treatment, all patients of the present study were put under dual antiplatelet therapy for a minimum period of 6 months.
Conclusion
The increasing overall life expectancy combined with the global diabetes epidemic has culminated in a progressively increasing prevalence of CLTI.(15)
Pedal/tibial access should be part of the routine armamentarium of any vascular surgeon for the treatment of peripheral arterial disease, especially when open surgical revascularization is not an option, due to systemic co-morbidities, lack of a suitable venous conduit or adequate run-off.
The results of the retrograde access and recanalization of chronic occlusions show a similar trend to the data reported in the literature, confirming it as a useful alternative. As so, the retrograde access approach for revascularization of CLTI patients appears to be a viable, safe and effective alternative that expands revascularization options after the failure of a more conventional endovascular anterograde approach, offering the possibility of salvaging a greater number of limbs.
REFERENCES
1. Bradbury, AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: an intention-to-treat analysis of amputation-free and overall survival in patients randomized to a bypass surgery-first or a balloon angioplasty-first revascularization strategyJ Vasc Surg, 51 (Suppl 10) (2010), pp. 5S-17S. [ Links ]
2. Bisdas T, Borowski M, Stavroulakis K, et al. Endovascular therapy versus bypass surgery as first-line treatment strategies for critical limb ischemia: results of the interim analysis of the CRITISCH registry. JACC Cardiovasc Interv 2016; 9:2557-2565 [ Links ]
3. Joels, CS, York, JW, Kalbaugh, CA, Cull, DL, Langan, EM, Taylor, SM. Surgical implications of early failed endovascular intervention of the superficial femoral artery. J Vasc Surg. 2008; 47: 562-565 [ Links ]
4. Goodney, PP, Beck, AW, Nagle, J, Welch, HG, Zwolak, RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009; 50: 54-60 [ Links ]
5. Montero-Baker M, Schmidt A, Braunlich S, et al. Retrograde approach for complex popliteal and tibioperoneal occlusions. J Endovasc Ther. 2008;15(5):594-604 [ Links ]
6. Scheinert D, Braunlich S, Scheinert S, Ulrich M, Biamino G, Schmidt A. Initial clinical experience with an ivus-guided transmembrane puncture device to facilitate recanalization of total femoral artery occlusions. Eurointervention 2005;1:115-9 [ Links ]
7. Schmidt A, Bakker OJ, Bausback Y, Scheinert D.The tibiopedal retrograde vascular access for challenging popliteal and below-the-knee chronic total occlusions: literature review and description of the technique. J Cardiovasc Surg (Torino). 2017 Jun;58(3):371-382 [ Links ]
8. Iyer SS, Dorros G, Zaitoun R, Lewin RF. Retrograde recanalization of an occluded posterior tibial artery by using a posterior tibial cutdown: Two case reports. Cathet Cardiovasc Diagn. 1990;20(4):251-253 [ Links ]
9. Spinosa DJ, Harthun NL, Bissonette EA, et al. Subintimal arterial flossing with antegraderetrograde intervention (SAFARI) for subintimal recanalization to treat chronic critical limb ischemia. J Vasc Interv Radiol. 2005;16(1):37-44 [ Links ]
10. Palena LM, Manzi M. Extreme below-the-knee interventions: retrograde transmetatarsal or transplantar arch access for foot salvage in challenging cases of critical limb ischemia. J Endovasc Ther. 2012;19(6):805-11 [ Links ]
11. Manzi M, Palena LM. Retrograde percutaneous transmetatarsal artery access: new approach for extreme revascularization in challenging cases of critical limb ischemia. Cardiovasc Intervent Radiol. 2013;36(2):554-7
12. Raskin D, Khaitovich B, Silverberg D, Halak M, Balan S, Rimon U. Primary Retrograde Dorsalis Pedis Artery Single Access for Revascularization of Chronic Total Occlusion in Patients with Critical Limb Ischemia. J Vasc Interv Radiol. 2019;30(4):554-559 [ Links ]
13. Welling RHA, Bakker OL, Scheinert D, Moll FL, Hazenberg CE, Mustapha JA, Borst GJ, Schmidt A. Below-the-Knee Retrograde Access for Peripheral Interventions: A Systematic Review. J Endovasc Ther. 2018 Jun;25(3):345-352 [ Links ]
14. Rogers RK, Dattilo PB, Garcia JA, Tsai T, Casserly IP. Retrograde approach to recanalization of complex tibial disease. Catheter Cardiovasc Interv. 2011;77(6):915-925 [ Links ]
15. Bazan HA, Le L, Donovan M, Sidhom T, Smith TA, Sternbergh WC,3rd. Retrograde pedal access for patients with critical limb ischemia. J Vasc Surg. 2014;60(2):375-381 [ Links ]
16. Kaushal A, Roche-Nagle G, Tan KT, Liao E, Eisenberg N, Oreopoulos GD, Rajan DK. Outcomes at a single center after subintimal arterial flossing with antegrade-retrograde intervention for critical limb ischemia. J Vasc Surg. 2018 May;67(5):1448-1454 [ Links ]
17. Taha AG, Abou Ali AN, Al-Khoury G, Singh MJ, Makaroun MS, Avgerinos ED, Chaer RA. Outcomes of infrageniculate retrograde versus transfemoral access for endovascular intervention for chronic lower extremity ischemia. J Vasc Surg. 2018 Oct;68(4):1088-1095. [ Links ]
18. Goltz JP, Planert M, Horn M, et al. Retrograde transpedal access for revascularization of below-the-knee arteries in patients with critical limb ischemia after an unsuccessful antegrade transfemoral approach. Rofo. 2016;188(10):940-948 [ Links ]
19. Walker CM, Mustapha J, Zeller T, schmidt a, Montero-Baker M, Nanjundappa a, et al. Tibiopedal access for crossing of infrainguinal artery occlusions: a prospective multicenter observational study. J endovasc Ther 2016;23:839-46 [ Links ]
20. Ndip A, Lavery LA, Boulton AJ. Diabetic foot disease in people with advanced nephropathy and those on renal dialysis. Curr Diab Rep 2010;10:283e90. [ Links ]
21. Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. EURODIALE Study Diabetologia 2008;51:747e55. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: rita.augusto1988@gmail.com (R. Augusto).
Recebido a 11 de junho de 2019
Aceite a 21 de fevereiro de 2020