Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.15 no.4 Lisboa dez. 2019
CASOS CLÍNICOS
Type B aortic intramural hematoma - when a sheep becomes a wolf
Hematoma intramural da aorta tipo B - vigilância clínica e imagiológica na identificação precoce de complicações
Nuno Henriques Coelho1, Clara Nogueira1, Victor Martins1, Jacinta Campos1, Andreia Coelho1, Rita Augusto1, Carolina Semião1, Evelise Pinto1, João Ribeiro1, João Peixoto1, Alexandra Canedo1
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar Vila Nova de Gaia/Espinho
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Type B aortic intramural hematoma (B-IMH) has a complex and variable natural history: it can remain stable and resolve spontaneously or progress to dissection, aneurysm, ulcer or even rupture. The possibility of disease progression, frequently with mild or no symptomatology, poses a significant treatment dilemma.
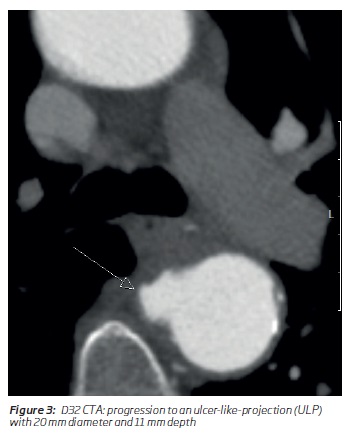
Clinical Case: We report a case of a 60 year-old-female diagnosed with an acute B-IMH, initially treated medically. However, 1-month control CTA revealed disease progression (increased B-IMH thickness and evolution to an ulcer-like-projection with 20 mm diameter and 11 mm depth). She was submitted to a left carotid-subclavian bypass followed by TEVAR and left-subclavian ostial embolization. During follow-up (5 months) patient remain asymptomatic, demonstrating favorable aortic remodeling.
Conclusion: Type B-IMH is a dynamic pathology. From presentation to late follow-up, patients remain at high risk for abrupt catastrophic complications. As reported, TEVAR seems to be a safe and effective approach in the event of unfavorable evolution.
Keywords: Acute aortic syndromes; Intramural hematoma; Penetrating aortic ulcer; TEVAR
RESUMO
Introdução: O hematoma intramural da aorta tipo B (HIM-B) tem uma história natural complexa e variável: pode permanecer estável e resolver espontaneamente ou evoluir para disseção aórtica, degenerescência aneurismática, úlcera penetrante ou mesmo rotura. Esta possibilidade de progressão da doença, frequentemente associada a sintomatologia frustre, torna a abordagem e tratamento do HIM-B complexos.
Caso clínico: Doente de 60 anos, do sexo feminino, com diagnóstico de HIM-B após recorrer ao serviço de urgência por dor torácica, inicialmente sujeita a tratamento médico. No angioTC de controlo, ao 1º mês, foi identificada uma ulceração da parede da aorta (20 mm de diâmetro e 11 de profundidade). Foi então submetida a um bypass carótido-subclávio esquerdo seguido de TEVAR e embolização ostial da artéria subclávia esquerda. Durante o follow-up (5 meses) a doente permanece assintomática verificando-se remodeling aórtico favorável.
Conclusion: O HIM-B é uma patologia dinâmica. Desde a apresentação inicial até uma fase avançada do follow-up pode cursar com complicações catastróficas. O tratamento endovascular parece ser uma opção segura e com bons resultados em caso de evolução desfavorável, tal como reportado neste caso.
Palavras-chave: Síndromes aórticas agudas; Hematoma intramural da aorta; Úlcera penetrante da aorta; TEVAR
Introduction
Acute aortic syndromes (AAS) comprehend a triad of life-threatening conditions that share identical risk factors (namely hypertension, atherosclerosis and increasing age), similar clinical presentations and overlapping imaging features(1). Aortic dissection (AD) (65-75% of all AAS), intramural hematoma (IMH) and penetrating aortic ulcer (PAU) (<10%) are dynamic and interchangeable pathologies. Both acute and long-term behavior can be highly unpredictable(2). IMH accounts for approximately 5-20% of AAS and typically addresses the descending thoracic aorta (60 to 70%)(3). Although several hypotheses have been proposed - vasa vasorum spontaneous rupture or presence of focal “microtears” - the true pathogenesis remain unclear(4,5). Typical computed angio-tomography (CTA) finding is the presence of a circular or crescentic-shaped thickening of the aortic wall (>5 mm), with absence of dissecting membrane or false lumen flow(6-8). For B-IMH best medical therapy (BMT) should always be part of the treatment. Medical management is based on blood pressure reduction to limit aortic wall stress. Antihypertensive agents should be immediately initiated to achieve a systolic blood pressure of less than 110-120 mmHg and heart rate bellow 60 beats/min. ß-blockers have been associated with improved long term survival being the first line treatment(1). Pain control and close surveillance are also part of medical management. Notwithstanding, B-IMH's natural course is quite unpredictable: it can remain stable and resolve spontaneously (32-40%) or progress to classic dissection (28-47%), aneurysm (20-45%) or even rupture (<5%)(2,9,10,11). Disease progression is reported in up to 44% BMT patients, frequently with mild symptomatology, turning the decision-making process challenging for the caring team(7,11,12). Thoracic endovascular aortic repair (TEVAR) for descending thoracic aorta pathologies (AD, PAU and aneurysms) is gaining its place and may also have a role in B-IMH management(13).
Clinical case
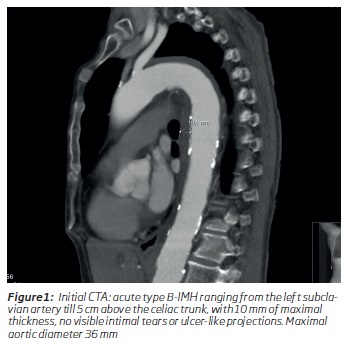
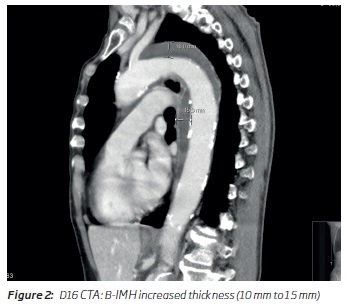
60 years-old-female, admitted due to a 4-hour evolution, acute onset, severe interscapular pain, without any other symptoms. She was a current smoker (60 pack-years) and had history of dyslipidemia. All vital signs and clinical exam were unremarkable, except for a blood pressure (BP) of 160/70 mmHg (similar in both arms). CTA revealed an acute aortic type B-IMH ranging from the left subclavian artery (LSA) till 5 cm above the celiac trunk, with maximal aortic diameter (MAD) of 36 mm, 10 mm of maximal thickness, without intimal tears or ulcer-like projections (figure 1). BMT strategy as defined by guidelines(1) was initiated and close surveillance was followed. With BP control (using intravenous ß-blockers and calcium channel antagonists), symptoms rapidly disappeared. Control CTA (day 7) revealed no imagiological progression and she was discharged with oral anti-hypertensive medication (consisting of ß-blockers and calcium channel antagonists, initiated at day 3 and with controlled BP). Notwithstanding being compliant with medication, at day 16, an intermittent mild thoracic discomfort made the patient seek medical attention. CTA was repeated revealing increased IMH thickness (from 10 to 15 mm) (figure 2). However, after pain control, she was discharged home without vascular surgery evaluation. Despite reporting only very sporadic mild thoracic discomfort, 1-month control CTA revealed not only increased IMH thickness but also progression to an ulcer-like-projection (ULP) with 20 mm diameter and 11 mm depth at proximal third of descending thoracic aorta (figure 3).
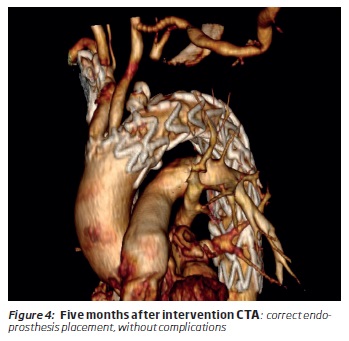
Patient was submitted to left carotid-subclavian bypass followed by TEVAR (Medtronic Valiant® 32×28×150 mm and 28×28×100 mm - oversize less than 10%) and LSA ostial occlusion (Abbot AVP II® 12×9 mm). After endovascular treatment she maintained oral ß-blockers and calcium channel antagonists, as well as acetylsalicylic acid and statin medication. During follow-up (5 months), patient reported no symptoms and control CTA showed favorable aortic remodeling (figure 4).
Discussion
B-IMH is still a mysterious entity, generating a lot of interest and discussion among vascular specialists. The prognosis and natural history of non-complicated B-HIM is unclear and dire complications can appear during follow-up, with minimal or no warning signs, even in complaint BMT patients. Morphological changes in IMH are very dynamic, particularly in the first 90 days, as shown in the present case(1). Therefore, increasing investigation regarding the identification of radiological findings predictable of progression to an unstable state is being performed. Unfortunately, most series are retrospective, heterogeneous, small, with short-term follow-up, precluding the definition of reliable therapeutic thresholds. Notwithstanding, persistent pain, refractory hypertension, acute-phase maximum aortic diameter (MAD) of > 45mm, wall thickness > 10 mm (range 10-15 mm) or chronic-phase MAD > 50 mm or > 0.5 cm/year increase, as well as the appearance of ULP along follow-up, are considered high-risk markers for progression and complications(11). Despite sporadic, patient referred a mild thoracic pain. In the presented case, symptoms, along with the radiological findings (progressive increased aortic wall thickness and de novo >20 mm in diameter and >10 mm depth ULP) led to endovascular treatment decision. Evolution to ULP during B-IMH follow-up is a frequent manifestation of aortic pathology progression (20 to 60% of cases)(11). It can have a delayed appearance and the estimated mean time between IMH onset and the appearance of an ULP is reported to be around 2.4 months (in this case, H 1 month)(14). Despite the scant data over TEVAR application in IMH, some recent series show encouraging results reporting favorable aortic remodeling, along with low aortic-related adverse events(8). Nevertheless, there are some concerns when performing TEVAR in B-IMH. First, frequently there is no focal intimal defect or a false lumen to be thrombosed and even when a ULP is visible, is difficult to define the “healthy” landing-zone. Consequently, longer aortic coverage is frequently required, caring a higher risk for neurological complications. As we anticipated a thoracic aorta coverage of > 200 mm with coverage of LSA (in order to achieve proximal and distal “healthy” landing-zones) we decided to perform LSA revascularization prior to this non-emergent TEVAR. Additionally, during and in the early period after intervention we also maintained mean arterial pressures > 90 mmHg. In our Centre we adopt a selective perioperative cerebrospinal fluid drainage policy. As we anticipated a relatively fast procedure, in a patient with no prior aortic intervention and with a previously revascularized LSA we decided not to do it. Considering the reported higher aortic wall frailty of IMH when compared to other AAS, a compromise between stent-graft fixation and risk of iatrogenic complications (dissection or rupture) is the key. In this case, we used the recommended < 10% oversize. On the same line, balloon angioplasty was performed only in the stent-graft overlap, avoiding the proximal or distal landing zones. Even after treatment, the patient should undergo a strict clinical and radiological surveillance. The follow-up protocol in our Center is 1 month, 6 months,1-year CTA and yearly thereafter. If the patient remains asymptomatic and without negative imagiological evolution, the interval can be extended to 2-3 years.
Conclusion
B-IMH is a treacherous pathology and changes on its evolution can appear abruptly. From presentation to late follow-up, patients remain at high risk for catastrophic complications. Close clinical and radiological follow-up is the keystone for preventing a sheep to become a wolf. Current studies privilege an endovascular approach for complicated IMH.
REFERENCES
1. Committee, W. et al. Editor ' s Choice e Management of Descending Thoracic Aorta Diseases Clinical Practice Guidelines of the European Society for Vascular Surgery ( ESVS ). 4-52 (2017). doi: 10.1016/j.ejvs.2016.06.005.
2. Maslow, A., Atalay, M. K. & Sodha, N. Intramural Hematoma. J. Cardiothorac. Vasc. Anesth. 1-22 (2018). doi: 10.1053/j.jvca.2018.01.025. [ Links ]
3. Moral, S., Avegliano, G., Ballesteros, E., Salcedo, M. T. & Evangelista, A. Clinical Implications of Focal Intimal Disruption in Patients With Type B Intramural Hematoma. J Am Coll Cardiol. 69, 28-39 (2017). [ Links ]
4. Ferrera, C. et al. Evolution and prognosis of intramural aortic hematoma. Insights from a midterm cohort study. Int. J. Cardiol. 249, 410-413 (2017). [ Links ]
5. Ferrera, C. et al. Evolution and prognosis of intramural aortic hematoma . Insights from a midterm cohort study. Int. J. Cardiol. 1-4 (2017). doi: 10.1016/j.ijcard.2017.09.170. [ Links ]
6. Muntanyà, X. et al. Predictive value of small ulcers in the evolution of acute type B intramural hematoma. Eur. J. Radiol. 81, 1569-1574 (2011). [ Links ]
7. Elefteriades, J. A. et al. Long-term behavior of aortic intramural hematomas and penetrating ulcers. J. Thorac. Cardiovasc. Surg. 151, 361-373.e1 (2015). [ Links ]
8. Piffaretti, G. et al. Best Medical Treatment and Selective Stent-GraftRepair for Acute Type B Aortic Intramural Hematoma. Semin. Thorac. Cardiovasc. Surg. 30, 279-287 (2018). [ Links ]
9. Tenorio, E. R. & Sandri, G. A. Penetrating Aortic Ulcer and Intramural Hematoma. Cardiovasc Interv. Radiol. 42(3), 321-334 (2019). [ Links ]
10. Nauta, Foeke; Kamman, Arnoud; Trimarchi, S. Penetrating Aortic Ulcer and Intramural Hematoma. Endovasc. Today 87-91 (2014). [ Links ]
11. Evangelista, A., Czerny, M., Nienaber, C., Schepens, M. & Rousseau, H. Interdisciplinary expert consensus on management of type B intramural haematoma and penetrating aortic ulcer. Eur J Cardiothorac Surg 47, 209-217 (2015). [ Links ]
12. Schlatter, T. et al. Type B intramural hematoma of the aorta: Evolution and prognostic value of intimal erosion. J. Vasc. Interv. Radiol. 22, 533-541 (2011). [ Links ]
13. Goldberg, J. B., Kim, J. B. & Sundt, T. M. Current understandings and approach to the management of aortic intramural hematomas. Semin. Thorac. Cardiovasc. Surg. 26, 123-131 (2014). [ Links ]
14. Bosma, M. S. et al. Ulcer-like Projections Developing in Noncommunicating Aortic Dissections: CT Findings and Natural History. AJR Am J Roentgenol. 895-905 (2009). [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: nunoc.90@gmail.com (N. Coelho).
Recebido a 14 de junho de 2019
Aceite a 03 de dezembro de 2019