Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Angiologia e Cirurgia Vascular
Print version ISSN 1646-706X
Angiol Cir Vasc vol.15 no.3 Lisboa Sept. 2019
ARTIGO DE REVISÃO
Obturator Hook Sign - When the common iliac vein disappearance eludes visual detection
Sinal do Gancho do Obturador - Quando a veia iliaca comum desaparece e não vemos
Andreia Coelho1,2, Gerard O'Sullivan3
1 Centro Hospitalar de Vila Nova de Gaia e Espinho
2 Faculdade de Medicina da Universidade do Porto
3 Galway University Hospitals
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Diagnosis of chronic iliac venous outflow obstruction is challenging, and no ideal imaging method has yet been defined. Even with imaging with superb detail, common iliac vein disappearance as occurs in Post-Thrombotic Syndrome (PTS) may be missed even by the most experienced radiologist. This scanning error occurs due to psychophysiological factors of human visual perception.
The purpose of this paper is to report on the “obturator hook sign”, evidencing obturator vein engorgement as a collateral pathway and hence a marker for hemodynamically significant chronic iliac venous outflow lesion, supporting this diagnosis.
Methods: Retrospective review of Indirect and Direct Computed Tomography Venography (CTV) and Magnetic Resonance Venography (MRV) imaging of the obturator hook sign and comprehensive literature review regarding iliac vein outflow obstruction diagnosis focusing on collateral vein development.
Results: The obturator hook sign is identified in Direct CTV, Indirect CTV and MRV of patients with chronic iliac venous outflow obstruction. The sign was never identified in imaging studies with no chronic iliac obstruction, suggesting high specificity.
Discussion: Venous collateralization is poorly understood, but it has been shown that when the main venous path is stenosed or occluded and the venous pressure rises, flow is side-tracked through alternative pathways. When the main venous path lesion is stented, flow once again takes the lower resistance pathway and the collaterals withdraw.
The obturator hook sign can be easily recognisable in CTV and MRV due to its peculiar anatomy and immediately points us towards hemodynamically significant chronic iliac venous outflow obstruction.
Keywords: Computed Tomography Angiography [MeSH]; Postthrombotic Syndrome [MeSH]; Diagnosis; Differential [MeSH]; May-Thurner Syndrome [MeSH]
RESUMO
Introdução: O diagnóstico de obstrução crónica do efluxo venoso ilíaco é desafiante e não existe nenhum método de imagem ideal. Mesmo com elevada qualidade de imagem a ausência súbita da veia ilíaca comum tal como ocorre na Síndrome Pós-Trombótico (SPT), pode ser subvalorizado mesmo por radiologistas experientes. Este erro de scanning ocorre devido a fatores psicofisiológicos da perceção visual humana.
O objetivo deste trabalho é relatar o “sinal do gancho do obturador”, demonstrando o aumento do calibre da veia obturadora como uma via colateral e, portanto, um marcador de lesão crónica hemodinamicamente significativa do efluxo venoso ilíaco.
Métodos: Estudo retrospetivo de imagens de venografia por tomografia computadorizada indireta e direta (VTC) e venografia por ressonância magnética (RMN) do sinal do obturador e revisão compreensiva da literatura relativa a diagnostico de obstrução do efluxo venoso ilíaco com enfâse nos mecanismos de desenvolvimento de colateralidade.
Resultados: O sinal do gancho do obturador é identificado em VTC e RMN de doentes com obstrução crónica do efluxo venoso ilíaco. O sinal não foi identificado em nenhum estudo imagiológico que não apresentasse concomitantemente obstrução do efluxo venoso, sugerindo tratar-se de um sinal com elevada especificidade.
Discussão: A colateralização venosa é um tema complexo, mas já foi demonstrado que, quando o trajeto venoso principal tem uma lesão hemodinamicamente significativa e a pressão venosa aumenta, o fluxo é desviado através de vias alternativas. Por outro lado, quando a lesão do trajeto venoso principal é tratada, o fluxo venoso regressa ao trajeto de menor resistência e as colaterais desaparecem.
O sinal do gancho do obturador pode ser facilmente reconhecido em VTC e RMN devido à sua anatomia particular e aponta imediatamente para a obstrução do fluxo venoso ilíaco hemodinamicamente significativo.
Palavras-chave: Angiotomografia Computorizada; Síndrome Pós-Trombótico; Diagnóstico Diferencial; Síndrome de May-Thurner
Introduction
Diagnosis of chronic iliac venous outflow obstruction is challenging, and no ideal imaging method has yet been defined. Phlebography is no longer used for routine examination of the venous network of the lower limbs, due to its invasiveness, but remains classified as the ‘‘gold standard’’(1)
Computed Tomography Venography (CTV) and Magnetic Ressonance Venography (MRV) have been increasingly used in this setting. However, even with imaging with superb detail common iliac vein disappearance as occurs in Post-Thrombotic Syndrome (PTS) may be missed by the most experienced radiologist. This scanning error occurs due to psychophysiological factors of human visual perception(2). It is easier to see something that is there, rather than noticing that something is suddenly not there.
The “obturator hook sign” (OHS) appears when the obturator vein becomes engorged, being a collateral pathway for chronic iliac venous outflow obstruction and hence a marker for hemodynamically significant iliac venous outflow lesion. In fact, obstructions of the ilio-cava sector reveal the functional importance of the pelvic veins and abdominal wall veins as cross-roads for shunting blood circulation. There are several anatomical factors that facilitate shunting: large number of anastomoses in the pelvis; absence of valvula in the pelvic veins and the abdominal pressure(3).
The purpose of this paper is to report on the “obturator hook sign” as a marker for hemodynamically significant chronic iliac venous outflow lesion in CTV and MRV.
Methods
Retrospective review of Indirect and Direct Computed Tomography Venography (CTV) and Magnetic Resonance Venography (MRV) imaging of the obturator hook sign and comprehensive literature review regarding iliac vein outflow obstruction diagnosis focusing on collateral vein development.
Ascending Venography
In the setting of chronic iliac vein outflow obstruction, ascending phlebography is still considered gold standard for assessment of chronic venous obstruction before treatment(5).
Indirect CTV
Indirect CTV is performed as a standard, nonoral, post-intravenous contrast-enhanced CT at approximately 120 to 150 seconds after injection of contrast, which is considerably later than portal venous phase(1).
ICTV is dependent on cardiac output, size of the intravenous line, rate of injection, and degree of hydration(1). Therefore, it can provide suboptimal or non-diagnostic CTV studies in 3.1% to 15.2% of cases(6,7).
Direct CTV
Direct CTV is performed as follows: First, a thigh-high compression stocking is placed on the affected limb, and a 21-gauge needle is inserted into any vein in the foot. Then, 100 mL of iodinated contrast is injected at 3 mL/second with a 30-mL saline chaser, and scans are acquired from mid-calf up to the diaphragm.
Direct CTV is an easy to reproduce technique and provides outstanding detail, when compared to indirect CTV. It is very useful for planning endovascular reconstruction, especially in postthrombotic patients.
MRV
MRV can be performed with or without contrast. In the latter, imaging of the venous system is suboptimal. Contrast-enhanced MR techniques allow for more detailed images with a specifically high signal intensity in blood. Similarly, to CTV, contrast can be administered in an upper arm vein or in a pedal vein with direct visualization of the lower extremity veins. However, as opposed to CTV, direct MRV has not been proven beneficial compared to indirect techniques(4).
Several studies have shown high-quality imaging of the venous system, from the calf up to the IVC, feasible and reproducible with several different imaging protocols. However, MRV remains an expensive, time-consuming and scarcely available exam that requires a level of expertise most centres have yet to reach(10).
Obturator Hook Sign
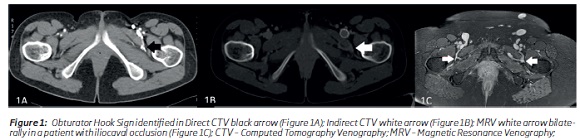
The obturator vein begins in the adductor region of the thigh and enters the pelvis through the obturator foramen, in the obturator canal. It runs backward and upward on the lateral wall of the pelvis to end in the hypogastric vein(16). When the obturator vein becomes engorged, a hook contouring the adductor muscle is identifiable in cross-sectional imaging (Figure 1).
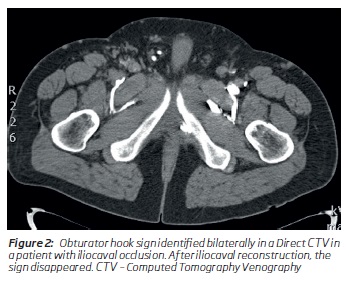
The obturator hook sign is identified in Direct CTV, Indirect CTV and MRV (Figure 1) as a sign of collateral pathway engorgement, all in patients with chronic iliac outflow occlusion.
Discussion
Collateral pathway development is poorly understood, but 2 major mechanisms have been entertained: The first and main mechanism is development of collateral channels as a result of venous obstruction or stenosis. The second is increased blood flow through collateral vessels due to an hyperdynamic status such as neoplasm or vascular lesion. Recognition of abnormal hemodynamic facilitates understanding of the physiology of such conditions and the identification of the level of narrowing(11).
In cases of common iliac vein obstruction, blood flow can be diverted by the internal iliac vein through the presacral and parametrial plexuses, ipsilateral ascending lumbar vein, ovarian veins, or paravertebral plexuses. When obstruction also involves the external iliac vein or common femoral vein, the deep circumflex iliac vein, obturator vein, or deep external pudendal vein can be activated too. In addition, blood flow can be diverted through the superficial external pudendal, pubic, and superficial epigastric veins, which leads to the visible collateral veins on the abdominal wall or across the pubic bone. Involvement of the IVC likely results in a more extensive collateral network, involving the paravertebral plexus and epigastric veins, draining into the azygos system and the superior vena cava. The latter veins can lead to wide-ranging externally visible collateral formation(3,12,13).
Another interesting finding concerning collateral pathways is that when the main stenosis is treated, flow once again takes the lower resistance pathway and the collaterals “disappear”(14,15).
The obturator hook sign is one of the many possible collateral pathways for iliac vein obstruction that is easily identified due to its peculiar anatomy, even when iliac vein obstruction identification is initially missed.
However, assessing the true value of the sign as a marker for iliac vein obstruction requires multicentric high volume evaluation of the sign in CTV comparing it with a gold standard for iliac vein lesions (possibly a venography).
Other possible collateral pathways include the development of clinically visible abdominal wall veins, described by Kurstjens et al as a sign with high specificity (86%; 95% CI 79-91) and high positive predictive value (93%; 95% CI 90-96) and relatively low sensitivity (53%; 95% CI 48-57) and negative predictive value (32%; 95% CI 19-36) for iliac vein obstruction diagnosis(17).
In conclusion, the obturator hook sign can be easily identified in direct CTV, indirect CTV and MRV and it is easily recognisable and immediately points us towards hemodynamically significant chronic iliac venous outflow obstruction, even when the iliac vein lesion is initially missed.
REFERENCES
1. Abdalla G, Fawzi Matuk R, Venugopal V, Verde F, Magnuson TH, Schweitzer MA, et al. The diagnostic accuracy of magnetic resonance venography in the detection of deep venous thrombosis: a systematic review and meta-analysis. Clin Radiol. 2015;70(8):858-71. [ Links ]
2. Pinto A, Brunese L. Spectrum of diagnostic errors in radiology. World J Radiol. 2010;2(10):377-83. [ Links ]
3. Kurstjens RL, van Vuuren TM, de Wolf MA, de Graaf R, Arnoldussen CW, Wittens CH. Abdominal and pubic collateral veins as indicators of deep venous obstruction. J Vasc Surg Venous Lymphat Disord. 2016;4(4):426-33. [ Links ]
4. Fraser DG, Moody AR, Morgan PS, Martel A. Iliac compression syndrome and recanalization of femoropopliteal and iliac venous thrombosis: a prospective study with magnetic resonance venography. Journal of vascular surgery. 2004;40(4):612-9. [ Links ]
5. Mahnken AH, Thomson K, de Haan M, O'Sullivan GJ. CIRSE standards of practice guidelines on iliocaval stenting. Cardiovascular and interventional radiology. 2014;37(4):889-97. [ Links ]
6. Reichert M, Henzler T, Krissak R, Apfaltrer P, Huck K, Buesing K, et al. Venous thromboembolism: additional diagnostic value and radiation dose of pelvic CT venography in patients with suspected pulmonary embolism. European journal of radiology. 2011;80(1):50-3. [ Links ]
7. Shi WY, Wang LW, Wang SJ, Yin XD, Gu JP. Combined Direct and Indirect CT Venography (Combined CTV) in Detecting Lower Extremity Deep Vein Thrombosis. Medicine (Baltimore). 2016;95(11):e3010. [ Links ]
8. Min SK, Kim SY, Park YJ, Lee W, Jung IM, Lee T, et al. Role of three-dimensional computed tomography venography as a powerful navigator for varicose vein surgery. Journal of vascular surgery. 2010;51(4):893-9. [ Links ]
9. Gagne PJ, Tahara RW, Fastabend CP, Dzieciuchowicz L, Marston W, Vedantham S, et al. Venography versus intravascular ultrasound for diagnosing and treating iliofemoral vein obstruction. J Vasc Surg Venous Lymphat Disord. 2017;5(5):678-87. [ Links ]
10. Arnoldussen CW, de Graaf R, Wittens CH, de Haan MW. Value of magnetic resonance venography and computed tomographic venography in lower extremity chronic venous disease. Phlebology. 2013;28 Suppl 1:169-75. [ Links ]
11. Umeoka S, Koyama T, Togashi K, Kobayashi H, Akuta K. Vascular dilatation in the pelvis: identification with CT and MR imaging. Radiographics. 2004;24(1):193-208. [ Links ]
12. Heijmen RH, Bollen TL, Duyndam DA, Overtoom TT, Van Den Berg JC, Moll FL. Endovascular venous stenting in May-Thurner syndrome. The Journal of cardiovascular surgery. 2001;42(1):83-7. [ Links ]
13. Ferris EJ, Lim WN, Smith PL, Casali R. May-Thurner syndrome. Radiology. 1983;147(1):29-31. [ Links ]
14. Raju S, Neglen P. High prevalence of nonthrombotic iliac vein lesions in chronic venous disease: a permissive role in pathogenicity. Journal of vascular surgery. 2006;44(1):136-43; discussion 44. [ Links ]
15. Neglen P, Raju S. Intravascular ultrasound scan evaluation of the obstructed vein. Journal of vascular surgery. 2002;35(4):694-700. [ Links ]
16. Brown SC, Gewillig M. Ever heard of the obturator vein? Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2010;75(3):416-9. [ Links ]
17. Kurstjens RL, van Vuuren TM, de Wolf MA, de Graaf R, Arnoldussen CW, Wittens CH. Abdominal and pubic collateral veins as indicators of deep venous obstruction. J Vasc Surg Venous Lymphat Disord. 2016;4(4):426-33. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: andreiasmpcoelho@gmail.com (A. Coelho).
Recebido a 07 de julho de 2019
Aceite a 13 de outubro de 2019