Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.14 no.3 Lisboa set. 2018
CASOS CLÍNICOS
Endovascular management of life-threatening carotid blowout syndrome after osteoradionecrosis of the mandibula - a case report and literature review
Tratamento endovascular de síndrome de carotid blowout agudo após osteoradionecrose da mandíbula - a propósito de um caso clínico
Andreia Coelho1,2, Miguel Lobo1, Gustavo Coelho3, Marta Azevedo3, Jacinta Campos1,2, Rita Augusto1,2, Nuno Coelho1,2, Ana Carolina Semião1,2, João Pedro Ribeiro1, Horácio Costa3, Alexandra Canedo1,2
1 Angiology and Vascular Surgery Department; Centro Hospitalar Vila Nova de Gaia e Espinho;
2 Faculdade de Medicina da Universidade do Porto;
3 Plastic and Reconstructive Surgery Department; Centro Hospitalar Vila Nova de Gaia e Espinho
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Aim: Carotid blowout syndrome is a rare but devastating complication of head and neck malignancy, and is associated with a reported mortality and neurologic morbidity of 40% and 60% respectively. The aim of this case report is to present our experience with a single case of massive haemorrhage from the internal carotid artery (ICA) in a previously irradiated neck treated with a stentgraft, hence maintaining carotid artery patency.
Methods: Relevant medical data were collected and literature review was performed.
Results: The patient is a 61-year-old male with a previous history of head and neck cancer submitted to radical surgery and chemo and radiotherapy. Seven years later, the patient was diagnosed with osteoradionecrosis of the mandibula and submitted to surgery. Hospital stay was prolonged due to local infection and suture dehiscence with carotid artery exposure. No previous episodes of sentinel bleeding were registered. Life-threatening haemorrhage from the surgical wound started acutely. Under manual compression, the patient was rushed to the angiography suite and the diagnostic angiography ascertained active bleeding from the ICA. A stentgraft Atrium Advanta V12 (Maquet Getinge group, Hudson, NH, USA) was deployed maintaining ICA patency. The patient was subsequently submitted to surgical reconstruction and had an uneventful recovery.
Discussion: Management of acute carotid blow syndrome is critical, often requiring a multidisciplinary approach. Stentgraft placement is a highly feasible and effective approach with lower morbimortality rates when compared to surgical repair/ ligation or endovascular embolization. However long term results with patency rates are currently lacking.
Keywords: Carotid Blowout Sindrome; Endovascular Procedures; Carotid Artery Injuries
RESUMO
Objetivo: A síndrome de blowout carotídeo é uma complicação rara mas potencialmente catastrófica, da neoplasia de cabeça e pescoço, e está associada a uma mortalidade e morbidade neurológica reportadas de 40% e 60%, respetivamente. Pretende-se apresentar a nossa experiência com um caso de blowout carotídeo com hemorragia maciça com origem na artéria carótida interna (ACI) num doente com história prévia de radioterapia cervical e osteorradionecrose da mandíbula, tratado por via endovascular com colocação de um stent recoberto mantendo, assim, a permeabilidade carotídea.
Métodos: Realizou-se revisão dos dados clínicos relevantes bem como revisão da literatura existente.
Resultados: Trata-se de um doente do sexo masculino de 61 anos, com história prévia de neoplasia da cabeça e pescoço, submetido a cirurgia radical e quimio e radioterapia. Sete anos depois, o paciente foi diagnosticado com osteorradionecrose da mandíbula e submetido a cirurgia reconstrutiva. A estadia hospitalar pós-operatória foi prolongada por infeção local e deiscência da ferida cirúrgica com exposição carotídea. Não houve registo de episódios prévios de hemorragia sentinela, no entanto o doente apresentou inicio súbito de hemorragia major com origem na ferida cirúrgica. Sob compressão manual, o doente foi admitido na suite angiográfica tendo-se constatado hemorragia ativa da ACI. Posteriormente implantou-se um stent recoberto Atrium Advanta V12 (Maquet Getinge, Hudson, NH, EUA) mantendo-se a permeabilidade da ACI.
Numa segunda fase, após estabilização do doente em unidade de cuidados intensivos, o doente foi submetido a reconstrução cirúrgica, sem intercorrências.
Discussão: O tratamento da síndrome de blowout carotídeo agudo é emergente, exigindo muitas vezes uma abordagem multidisciplinar. A colocação de um stent recoberto é uma abordagem exequível e eficaz em contexto agudo, com menores taxas de morbimortalidade associadas, quando comparado ao tratamento/laqueação cirúrgica ou embolização endovascular. No entanto, desconhece-se os resultados a longo prazo, em particular taxas de permeabilidade.
Palavras-chave: Síndrome de Carotid Blowout; Tratamento endovascular; Lesão da artéria carótida
Aim: Carotid blowout syndrome (CBS) is defined as the rupture of the carotid artery associated with haemorrhage or exposure of part of the carotid artery in a patient who has undergone aggressive management for head and neck cancer. It is associated with a reported mortality and neurologic morbidity of 40% and 60% respectively.(1) It is a true surgical emergency, and the classical life-saving approach is carotid artery ligation, due to the technical difficulty associated with repairing a previously irradiated and/or infected artery.(2,3) The aim of this case report was to present our experience with a single case of massive haemorrhage from the internal carotid artery in a previously irradiated neck treated with a covered stent, hence maintaining carotid artery patency.
Methods: Relevant medical data were collected and review of the literature was performed. A Medline database search was performed with the following query: Carotid blowout syndrome AND Endovascular procedures [MeSH].
Results: The patient is a 61-year-old male with a previous history of head and neck cancer diagnosed in 2010 and submitted to radical surgery and chemo and radiotherapy. Seven years later, the patient was diagnosed with osteoradionecrosis of the mandible and submitted to surgery. However, hospital stay was prolonged due to local infection and suture dehiscence with carotid artery exposure. No previous episodes of sentinel bleeding were registered. Life-threatening haemorrhage from the surgical wound started acutely. (Figure 1) Initially, an attempt to surgically ligate the artery was entertained, but the neck was impenetrable due to fibrosis. Also, the haemorrhage was above the mandible angle, with difficult surgical access.
Under manual compression, the patient was rushed to the angiography suite and manual compression was needed throughout the whole procedure.
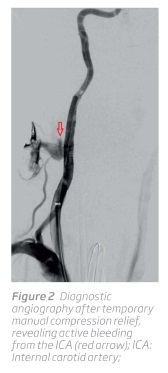
Access was obtained in the left common femoral artery, and after selective catheterization of the right common carotid artery, a diagnostic angiography was performed. Temporary relief of manual compression was necessary in order to identify the active bleeding site from the internal carotid artery approximately 2cm above the mandible angle. (Figure 2)
A Check Flo sheath (Cook Medical, Bloomington, Indiana) was positioned and afterwards a stentgraft Atrium Advanta V12, (Maquet Getinge group, Hudson, NH, USA) was deployed maintaining ICA patency. (Figure 3)
Intravenous cefoxitin and vancomycin were administered before the procedure and maintained for 24h.
During the interventional procedure, a heparin bolus of 50 IU/kg body weight was administered before stent graft deployment. No pre-medication with antiplatelet therapy was given before stent insertion, but he was started on daily intake of aspirin (100 mg/day) immediately after stent placement and maintained lifelong.
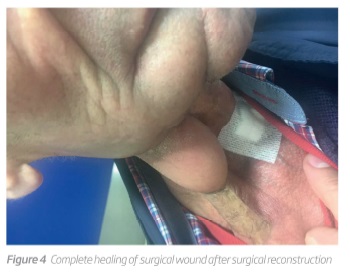
Following the procedure, the patient was asymptomatic with no haemorrhagic recurrence. He was subsequently submitted to surgical reconstruction with latissimus dorsi muscle and had an uneventful recovery.
On follow-up visit 3 months post-procedure the patient was asymptomatic and the carotid artery was effectively covered with muscle and skin with complete healing of the surgical wound. (Figure 4) Ultrasound Doppler evaluation revealed a patent stentgraft.
Discussion
CBS is a serious complication of head and neck malignancy, which can be divided into 3 main categories: impending, in which the carotid artery is exposed with no previous episodes of bleeding. Threatened in which sentinel transoral or transcervical bleeding episodes occur, but are managed with conservative treatment. Finally, acute CBS, in which life-threatening haemorrhage or carotid artery rupture occur.(4-6)
Prevention of the syndrome is paramount and is primarily accomplished by prophylactic coverage of the major vasculature with well-vascularized tissue, especially in an irradiated field. Modern reconstructive techniques have therefore significantly decreased its occurrence especially in a subset of patients with multiple risk factors who are at particularly high risk for this syndrome, as follows: prior radiotherapy; prior radical neck dissection; mucocutaneous fistula; flap necrosis; wound infection; poor nutrition or compromised wound healing; recurrent tumor;(4,7)
There are several possible approaches. Open surgery is associated with high morbi-mortality, due to the technical difficulty of dealing with anatomy altered by prior surgery and radiation with resulting fragile tissues that heal poorly.(5) Open approach includes surgical bypass or surgical ligation, with the latter being the only alternative in most patients.(8)
The development of endovascular techniques has significantly altered CBS management, with an associated decrease in short-term morbidity and mortality. However, the long-term mortality of patients experiencing this complication remains essentially unchanged because it usually occurs in the setting of recurrent and/or uncontrolled tumors in the head and neck region.(4)
Endovascular options include coil embolization or detachable balloon occlusion of the carotid artery. This approach is associated with a risk of 15-20% for neurologic morbidity. Pre-occlusion tests are possible with the exception of acute haemorrhagic episodes.(9)
Stentgraft placement is a highly feasible and effective approach with the potential advantage of maintaining carotid artery patency, reducing morbi-mortality rates when compared to surgical repair/ ligation or endovascular coil embolization. However, it may be associated with a technical challenge due to large luminal calibre discrepancy between ICA and CCA.(10-12)
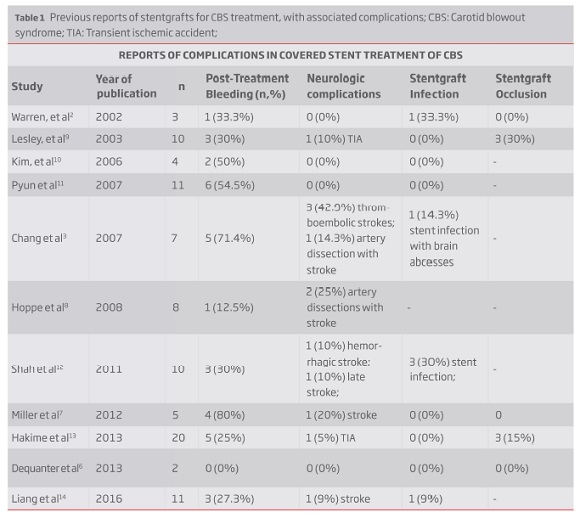
Long term results with patency rates are currently lacking. Literature review also reveals lack of data concerning risk for thromboembolic or other complications.(10) Only a few series have been published, with the biggest having 20 patients. They reveal an unneglectable risk for stentgraft occlusion, neurological events (due to thromboembolic events, artery dissection or stent occlusion) and stentgraft infection with possible brain abscesses. (Table 1) In fact, necrotic tumour represents an unsterile field and endovascular implantation of prosthetic material in an infected environment is a concern, but unfortunately there are no guidelines for antibiotherapy in this setting.(13) Close follow-up should be maintained due to the risk of recurrent bleeding.(14)
In conclusion, CBS may be a marker of poor prognosis due to advanced disease rather than the mortal event and should be managed aggressively.(14) Management of acute CBS is critical, often requiring a multidisciplinary approach. Stentgraft placement is a highly feasible and effective approach with lower morbimortality rates when compared to surgical repair/ ligation or endovascular embolization;
REFERENCES
1. Dong F, Li Q, Wu J, Zhang M, Zhang G, Li B, et al. Carotid blowout syndrome after nasopharyngeal carcinoma radiotherapy: successful treatment by internal carotid artery occlusion after stent implantation failure. Springerplus. 2016;5(1):1553. https://acvjournal.com/index.php/acv/article/view/146
2. Warren FM, Cohen JI, Nesbit GM, Barnwell SL, Wax MK, Andersen PE. Management of carotid 'blowout' with endovascular stent grafts. Laryngoscope. 2002;112(3):428-33. DOI: 10.1097/00005537-200203000-00004.
3. Chang FC, Lirng JF, Luo CB, Guo WY, Teng MM, Tai SK, et al. Carotid blowout syndrome in patients with head-and-neck cancers: reconstructive management by self-expandable stent-grafts. AJNR Am J Neuroradiol. 2007;28(1):181-8. [ Links ]
4. Gleysteen J, Clayburgh D, Cohen J. Management of Carotid Blowout from Radiation Necrosis. Otolaryngol Clin North Am. 2016;49(3):829-39. [ Links ]
5. Haas RA, Ahn SH. Interventional management of head and neck emergencies: carotid blowout. Semin Intervent Radiol. 2013;30(3):245-8. [ Links ]
6. Dequanter D, Shahla M, Paulus P, Aubert C, Lothaire P. Transarterial endovascular treatment in the management of life-threatening carotid blowout syndrome in head and neck cancer patients: review of the literature. J Mal Vasc. 2013;38(6):341-4. [ Links ]
7. Miller T, Burns J, Farinhas J, Pasquale D, Haboosheh A, Bello JA, et al. Covered stents safely utilized to prevent catastrophic hemorrhage in patients with advanced head and neck malignancy. Journal of neurointerventional surgery. 2012;4(6):426-34. [ Links ]
8. Hoppe H, Barnwell SL, Nesbit GM, Petersen BD. Stent-grafts in the treatment of emergent or urgent carotid artery disease: review of 25 cases. J Vasc Interv Radiol. 2008;19(1):31-41. DOI: 10.1016/j.jvir.2007.08.024. [ Links ]
9. Lesley WS, Chaloupka JC, Weigele JB, Mangla S, Dogar MA. Preliminary experience with endovascular reconstruction for the management of carotid blowout syndrome. AJNR American journal of neuroradiology. 2003;24(5):975-81. [ Links ]
10. Kim HS, Lee DH, Kim HJ, Kim SJ, Kim W, Kim SY, et al. Life-threatening common carotid artery blowout: rescue treatment with a newly designed self-expanding covered nitinol stent. The British journal of radiology. 2006;79(939):226-31. [ Links ]
11. Pyun HW, Lee DH, Yoo HM, Lee JH, Choi CG, Kim SJ, et al. Placement of covered stents for carotid blowout in patients with head and neck cancer: follow-up results after rescue treatments. AJNR American journal of neuroradiology. 2007;28(8):1594-8. [ Links ]
12. Shah H, Gemmete JJ, Chaudhary N, Pandey AS, Ansari SA. Acute life-threatening hemorrhage in patients with head and neck cancer presenting with carotid blowout syndrome: follow-up results after initial hemostasis with covered-stent placement. AJNR American journal of neuroradiology. 2011;32(4):743-7. [ Links ]
13. Hakime A, Khoury E, Hameg A, Liberge R, Deschamps F, Farouil G, et al. Polytetrafluoroethylene-covered nitinol stent graft for treatment of carotid artery blowout syndrome in head and neck cancer patients. Laryngoscope. 2013;123(7):1670-5. [ Links ]
14. Liang NL, Guedes BD, Duvvuri U, Singh MJ, Chaer RA, Makaroun MS, et al. Outcomes of interventions for carotid blowout syndrome in patients with head and neck cancer. Journal of vascular surgery. 2016;63(6):1525-30. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: andreiasmpcoelho@gmail.com (A. Coelho).
Ethical Responsabilities
Protection of patients and animals: The authors state that for this investigation no experiments were performed on humans and / or animals.
Confidentiality of the data: The authors state that they have followed the centre´s established protocols on the publication of patient data.
Right to privacy and informed consent: The authors declare that no patient data is available in this article.
Conflict of interest: The authors declare no potential confict of interest.
Recebido a 27 de maio de 2018
Aceite a 12 de agosto de 2018