Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.14 no.3 Lisboa set. 2018
CASOS CLÍNICOS
May-Thurner Syndrome: a case report after two years of endovascular treatment
Síndrome de May-Thurner: um caso clínico dois anos após tratamento endovascular
Tony R. Soares1,2, José Tiago3, Viviana Manuel1,2, Pedro Amorim1,2,4, João Leitão4,5, Carlos Martins1,2, Luís Mendes Pedro1,2,4
1 Department of Vascular Surgery, Hospital Santa Maria, Lisbon, Portugal
2 Lisbon Academic Medical Centre, Lisbon, Portugal
3 Vascular Surgery Department, Hospital Beatriz Ângelo, Loures, Portugal
4 University of Lisbon, Lisbon, Portugal
5 Department of Radiology, Hospital Santa Maria, Lisbon, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Previously considered a rare clinical condition, the development of more sophisticated imaging methods and endovascular intervention for deep venous thrombosis (DVT) led to a more frequent identification of May-Thurner Syndrome.
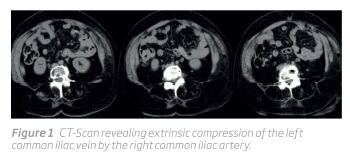
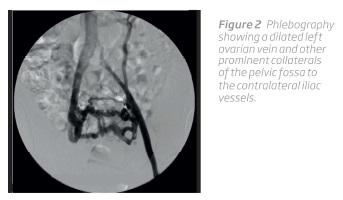
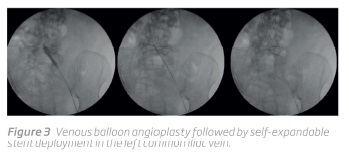
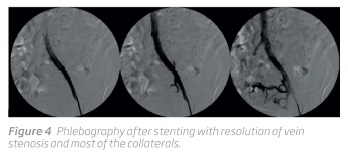
We present a 68 years-old woman with history of chronic pain and edema in the left lower limb and a CT-scan finding of left common iliac vein compression. Phlebography confirmed a stenosis in the confluence of the left common iliac vein with the inferior vena cava and a dilated left ovarian vein as well as voluminous collaterals in the pelvic fossa to the contralateral iliac vessels. These aspects are suggestive of May-Thurner Syndrome. The lesion was treated by venous angioplasty and stenting of the left common iliac vein. The recovery was uneventful, the patient remained on antiplatelet therapy and anticoagulation and had a notorious clinical improvement.
May-Thurner Syndrome should be suspected in patients with chronic symptoms of venous insufficiency or as an underlying cause of acute proximal DVT in the left lower limb.
Keywords: Deep vein thrombosis, DVT, iliac veins, May-Thurner syndrome, Cockett syndrome, iliac vein compression syndrome, venous stenting.
RESUMO
Previamente considerada como uma entidade clínica rara, o desenvolvimento de métodos de imagem cada vez mais sofisticados e a proliferação do tratamento endovascular da TVP, tornou a Síndrome de May-Thurner um diagnóstico cada vez mais frequente na nossa prática clínica.
Apresentamos o caso de uma doente de 68 anos de idade com queixas crónicas de dor e edema do membro inferior esquerdo e um achado em angio-TC de compressão da veia ilíaca primitiva. A flebografia confirmou a presença de uma estenose na confluência entre a veia ilíaca primitiva esquerda com a veia cava inferior, a dilatação da veia ovárica esquerda e uma volumosa rede de colaterais da fossa pélvica com comunicação com os vasos ilíacos contralaterais - aspetos sugestivos da Síndrome de May-Thurner. A lesão foi tratada com angioplastia transluminal percutânea com implantação de stent na veia ilíaca primitiva esquerda. O periodo pós-operatório decorreu sem intercorrências. A doente teve alta sob antiagregação e anticoagulação com uma notória melhoria clínica.
A Síndrome de May-Thurner é uma entidade clínica que deve ser suspeitada em doentes com sintomatologia crónica de insuficiência venosa ou eventos de trombose venosa profunda no membro inferior esquerdo.
Palavras-chave: Trombose venosa profunda, TVP, veias ilíacas, Síndrome de May-Thurner, Síndrome de Cockett, Síndrome de compressão da veia ilíaca, stenting venoso.
Introduction
May-Thurner Syndrome, also known as Cockett syndrome or iliac vein compression syndrome, is the symptomatic presentation caused by chronic pulsatile extrinsic compression of the left common iliac vein by the right common iliac artery against the lumbar vertebral body(1,2). May-Thurner Syndrome frequently presents as chronic venous insufficiency or deep venous thrombosis(1). We present herein a woman with chronic history of a prominent edema in the left lower limb.
Case Report
A 68 years-old woman complaining of chronic edema and a gradually increase of pain in the left lower limb was referred to Vascular Surgery Department with a CT-scan revealing left common iliac vein compression (Figure 1).
The patient had history of hypertension, poliomyelitis at 8 months of age, hepatitis C acquired after blood transfusion at 41 years-old, treated with Interferon that resulted in thyroiditis with hypothyroidism, and knee replacement surgery at 48 years-old. She denied history of deep venous thrombosis (DVT) or known pulmonary embolism. At physical examination, we observed a significant edema of the entire left lower limb, with Godets sign, and no alterations in the color skin or temperature. The contralateral lower limb presented with no alterations. Both lower limbs have femoral, popliteal and distal pulses. She was submitted to a phlebographic examination which confirmed a stenosis in the confluence of the left common iliac vein with the inferior vena cava. A dilated left ovarian vein and other prominent collaterals of the pelvic fossa to the contralateral iliac vessels were also observed (Figure 2).
Compression of the left renal vein between the abdominal aorta and superior mesenteric artery - nutcracker syndrome - was excluded by CT scan and phlebography.
Before a symptomatic left common iliac vein stenosis compatible with May-Thurner Syndrome, we proposed an endovascular procedure.
The patient was submitted to left femoral vein catheterization with a 5Fr sheath, the lesion was easily crossed with a hydrophilic guide wire and a venous balloon angioplasty was performed (balloons 10x40mm and 14x40mm) followed by self-expandable stent deployment (Zilver Vena CookMedical® 14x100 mm) in the left common iliac vein (Figure 3 and 4).
The recovery was uneventful and the patient was discharged in the next day under antiplatelet (acetylsalicylic acid) and anticoagulation (tinzaparin for the first two weeks, followed by rivaroxaban) therapy. She had a notorious resolution of the limb edema, achieving a comparable diameter with the contralateral leg. After more than two years of follow up, the patient remains stable despite some lymphedema secondary to 2 events of erysipelas.
Discussion
May-Thurner Syndrome usually refers to the clinical impact of an extrinsic compression of the left common iliac vein between the right common iliac artery and lumbar vertebral body. Previously considered a rare clinical finding, recent imaging techniques revealed that this condition may be more common. Additionally, the increasing use of endoluminal approach to treat DVT have augmented the suspicion index to this syndrome(3).
The anatomical variation behind this pathology is estimated to have a prevalence of about 22-24% in an asymptomatic population and 37-61% in symptomatic left lower limbs(2,4-6).The underlying lesion to this syndrome seems to be iliac vein spurs, which corresponds to a form of collagen scar typically observed in patients with extrinsic venous compression, identified in roughly half of the patients with acute left iliac venous thrombosis(6,7).
May-Thurner Syndrome is more common in young female patients in the third to fifth decades of life(1). The suspicion of the syndrome should be raised mainly in two settings(8,9): (1) a potential underlying condition for proximal DVTs; (2) a cause of left lower limb chronic venous insufficiency (presenting, for example, with edema, pain, varicose veins, lipodermatosclerosis or ulcerative lesions)(1).
Invasive phlebography is still considered by many the gold standard diagnostic method(1,5,10-12), however, it is complemented and even replaced by other modalities, such as computed tomography venography (CTV)(13), magnetic resonance venography (MRV)(14) and intravascular ultrasound (IVUS)(15). CTV is a useful tool to identify left common iliac vein compression with high sensitivity and specificity and a great tool for differential diagnosis of left lower extremity swelling(12,14). MRV is an expensive technology that offers comparable imaging with CTV and is capable to estimate pelvic collaterals flow. Intravascular ultrasound (IVUS) imaging is evolving as an important methodology, mainly intra-operatively to confirm the diagnosis and to assess the efficacy of stenting (sizing and correct apposition)(12,14,16,17). It is also important for the evaluation of residual venous narrowing determined by vessel recoil or by webs, spurs or wall thickening areas. In a small series of 16 patients, IVUS influenced 50% of endovascular management(17). Nevertheless, further studies are necessary to evaluate the best applications of all these imaging tools in May-Thurner syndrome.
Before the advent of the endovascular approach, treatment options of iliac vein compression syndrome was anticoagulation and surgery(8). Several surgical techniques were described, such as ilio-iliac vein crossover bypass, left femoral vein-to-right femoral vein bypass with the greater saphenous vein and a temporary arteriovenous fistula (Palma procedure) or a patch venoplasty with distal division of the right common iliac artery and positioning the artery behind the left common iliac vein(7,18). However, only a few long-term studies with modest results were achieved, with the best outcomes obtained by the most invasive procedures(7).
In the last years, the development of endovascular devices suitable for venous territory, expanded its indication to treat venous iliac pathologies(8). The advantage of a minimally invasive, fastest and easier techniques, with better short-term results, made endovascular approach as a first-choice treatment for occlusive lesions. However, with the exponential acceptance of this less invasive options, there are just a few comparative studies between conventional and endoluminal therapies(7,8).
An important number of studies discussing the endovascular treatment of iliac vein lesions reported high technical success (87-100%) and high primary patency rates (79-98.7%)(3,8,19-26). Ye et al obtained outstanding results with primary and secondary patency rates of 98.7% and 100% for a median follow-up of 4 years in 205 symptomatic patients with nonthrombotic iliac vein compression lesions(24). A new self-expanding hybrid nitinol venous stent was developed with a proximal closed-cell segment that provides higher radial force at the compression site and an oblique design at the proximal end, preventing to extend the stent into the inferior vena cava(27). This new technology appears to provide good early patency and clinical outcomes(27).
Evidence-based clinical practice guidelines from Society for Vascular Surgery and American Venous Forum recommend self-expanding metallic stents for chronic iliocaval underlying compressive syndromes persisting after endovascular thrombus-removal techniques, in patients with proximal DVT(28). Although the feasibility and good early and mid-term results of iliocaval venous stenting, long-term results are unclear.
General recommendations advise postprocedure anticoagulation for at least 6 months, despite lacking in evidence-based studies(8,9,20,21,24). Some authors also recommend antiplatelet drugs from 6 months to lifetime(9,24).
Conclusion
May-Thurner Syndrome is more common than previously assumed. Frequently presenting as chronic venous insufficiency or deep venous thrombosis, it is important to keep a high index of suspicion. Invasive phlebography is considered the gold standard to identify iliac vein compression but CT scan is growing as a first-choice diagnostic method. Endovascular approach is well established and the first line treatment, achieving good short-term results. However, the long-term behavior of venous stents is not well known.
REFERENCES
1. Fazel R, Froehlich JB, Williams DM, Saint S, Nallamothu BK. A Sinister Development. N Engl J Med. 2007;357(1):53-59. DOI: 10.1056/NEJMcps061337. [ Links ]
2. Kibbe MR, Ujiki M, Goodwin a. L, et al. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39(5):937-943. DOI: 10.1016/j.jvs.2003.12.032. [ Links ]
3. Bozkaya H, Cinar C, Ertugay S, et al. Endovascular Treatment of Iliac Vein Compression (May-Thurner) Syndrome: Angioplasty and Stenting with or without Manual Aspiration Thrombectomy and Catheter-Directed Thrombolysis. Ann Vasc Dis. 2015;8(1):21-28. DOI: 10.3400/avd.oa.14-00110. [ Links ]
4. May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8(5):419-427. DOI: 10.1177/000331975700800505. [ Links ]
5. Wolpert LM, Rahmani O, Stein B, Gallagher JJ, Drezner a D. Magnetic resonance venography in the diagnosis and management of May-Thurner syndrome. Vasc Endovascular Surg. 2002;36(1):51-57. DOI: 10.1177/153857440203600109. [ Links ]
6. Chung JW, Yoon CJ, Jung S Il, et al. Acute Iliofemoral Deep Vein Thrombosis: Evaluation of Underlying Anatomic Abnormalities by Spiral CT Venography. J Vasc Interv Radiol. 2004;15(3):249-256. DOI: 10.1097/01.RVI.0000109402.52762.8D. [ Links ]
7. Mickley V, Schwagierek R, Rilinger N, Gorich J, Sunder-Plassmann L. Left iliac venous thrombosis caused by venous spur: Treatment with thrombectomy and stent implantation. J Vasc Surg. 1998;28(3):492-497. DOI: 10.1016/S0741-5214(98)70135-1. [ Links ]
8. OSullivan GJ, Semba CP, Bittner C a, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000;11(7):823-836. DOI: 10.1016/S1051-0443(07)61796-5. [ Links ]
9. Mousa AY, AbuRahma AF. May-Thurner Syndrome: Update and Review. Ann Vasc Surg. 2013;27(7):984-995. DOI: 10.1016/j.avsg.2013.05.001. [ Links ]
10. Taheri S a, Williams J, Powell S, et al. Iliocaval compression syndrome. Am J Surg. 1987;154(2):169-172. DOI: 10.1177/153100359200500211. [ Links ]
11. Chamarthy MR, Sutphin P, Anderson M, Reddick M, Kalva SP. Evolving Concepts in the Diagnosis and Management of May-Thurner Syndrome. J Clin Interv Radiol. 2016;1:23-30. DOI: 10.1055/s-0036-1597954. [ Links ]
12. Brinegar KN. Iliac vein compression syndrome: Clinical, imaging and pathologic findings. World J Radiol. 2015;7(11):375. DOI: 10.4329/wjr.v7.i11.375. [ Links ]
13. Kuo Y-S, Chen C-J, Chen J-J, et al. May-Thurner syndrome: Correlation between digital subtraction and computed tomography venography. J Formos Med Assoc. 2015;114(4):363-368. DOI: 10.1016/j.jfma.2012.12.004. [ Links ]
14. Knuttinen M-G, Naidu S, Oklu R, et al. May-Thurner: diagnosis and endovascular management. Cardiovasc Diagn Ther. 2017;7(S3):S159-S164. DOI: 10.21037/cdt.2017.10.14. [ Links ]
15. Gagne PJ, Tahara RW, Fastabend CP, et al. Venography versus intravascular ultrasound for diagnosing and treating iliofemoral vein obstruction. J Vasc Surg Venous Lymphat Disord. 2017;5(5):678-687. DOI: 10.1016/j.jvsv.2017.04.007. [ Links ]
16. Birn J, Vedantham S. May-Thurner syndrome and other obstructive iliac vein lesions: Meaning, myth, and mystery. Vasc Med. 2015;20(1):74-83. DOI: 10.1177/1358863X14560429. [ Links ]
17. Forauer AR, Gemmete JJ, Dasika NL, Cho KJ, Williams DM. Intravascular ultrasound in the diagnosis and treatment of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2002;13(5):523-527. DOI: 10.1016/S1051-0443(07)61535-8. [ Links ]
18. Akers DL, Creado B, Hewitt RL. Iliac vein compression syndrome: case report and review of the literature. J Vasc Surg. 1996;24(3):477-481. [ Links ]
19. Hurst DR, Forauer AR, Bloom JR, Greenfield LJ, Wakefield TW, Williams DM. Diagnosis and endovascular treatment of iliocaval compression syndrome. J Vasc Surg. 2001;34(1):106-113. DOI: 10.1067/mva.2001.114213. [ Links ]
20. Kwak H-S, Han Y-M, Lee Y-S, Jin G-Y, Chung G-H. Stents in common iliac vein obstruction with acute ipsilateral deep venous thrombosis: early and late results. J Vasc Interv Radiol. 2005;16(6):815-822. DOI: 10.1097/01.RVI.0000157690.91690.38. [ Links ]
21. Lamont JP, Pearl GJ, Patetsios P, et al. Prospective evaluation of endoluminal venous stents in the treatment of the May-Thurner syndrome. Ann Vasc Surg. 2002;16(1):61-64. DOI: 10.1007/s10016-001-0143-3. [ Links ]
22. Liu Z, Gao N, Shen L, et al. Endovascular treatment for symptomatic iliac vein compression syndrome: a prospective consecutive series of 48 patients. Ann Vasc Surg. 2014;28(3):695-704. DOI: 10.1016/j.avsg.2013.05.019. [ Links ]
23.Lee K, Sung J-A, Kim J-S, Park T-J. The roles of obesity and gender on the relationship between metabolic risk factors and non-alcoholic fatty liver disease in Koreans. Diabetes Metab Res Rev. 2009;25(2):150-155. DOI: 10.1002/dmrr.924. [ Links ]
24. Ye K, Lu X, Li W, et al. Long-Term Outcomes of Stent Placement for Symptomatic Nonthrombotic Iliac Vein Compression Lesions in Chronic Venous Disease. J Vasc Interv Radiol. 2012;23(4):497-502. DOI: 10.1016/j.jvir.2011.12.021. [ Links ]
25. Oguzkurt L, Tercan F, Ozkan U, Gulcan O. Iliac vein compression syndrome: outcome of endovascular treatment with long-term follow-up. Eur J Radiol. 2008;68(3):487-492. DOI: 10.1016/j.ejrad.2007.08.019. [ Links ]
26. van Vuuren TMAJ, de Wolf MAF, Arnoldussen CWKP, et al. Editors Choice - Reconstruction of the femoro-ilio-caval outflow by percutaneous and hybrid interventions in symptomatic deep venous obstruction. Eur J Vasc Endovasc Surg. 2017;54(4):495-503. DOI: 10.1016/j.ejvs.2017.06.023. [ Links ]
27. Stuck AK, Kunz S, Baumgartner I, Kucher N. Patency and Clinical Outcomes of a Dedicated, Self-Expanding, Hybrid Oblique Stent Used in the Treatment of Common Iliac Vein Compression. J Endovasc Ther. 2017;24(1):159-166. DOI: 10.1177/1526602816676803. [ Links ]
28. Meissner MH, Gloviczki P, Comerota AJ, et al. Early thrombus removal strategies for acute deep venous thrombosis: Clinical Practice Guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2012;55(5):1449-1462. DOI: 10.1016/j.jvs.2011.12.081. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: tony.ramos.soares@gmail.com (T. Soares).
Ethical Issues
Conflicts of interest: The authors declare that there is no conflict of interest regarding the publication of this article.
Protection of people and animals: The authors declare that for this investigation no experiments were carried out on humans or animals.
Confidentiality of the data: The authors state that they have followed the protocols of their institution respecting to patient data.
Right to privacy and informed consent: The authors declare that no patient data appears in this article.
Recebido a 30 de dezembro de 2017
Aceite a 21 de agosto de 2018