Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.14 no.3 Lisboa set. 2018
CASOS CLÍNICOS
Entrapment syndrome in a non-athletic patient
Síndrome do Entrapment Popliteu em doente não atleta
Tony R. Soares1,3, José Tiago1,3, Viviana Manuel1,3, Carlos Martins1,3, Pedro Amorim1,2,3, Luís Mendes Pedro1,2,3
1. Department of Vascular Surgery, Hospital Santa Maria, Lisbon, Portugal
2. University of Lisbon, Lisbon, Portugal
3. Lisbon Academic Medical Centre, Lisbon, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
The popliteal artery entrapment syndrome (PAES) is a major cause of claudication and acute ischemia of lower limb in young athletes without risk factors for atherosclerosis.
We present a 39 years-old female patient with no relevant past history and no sport activity, admitted to our emergency department with acute disabling claudication in the right lower limb caused by retrogeniculate popliteal artery occlusion. Computed tomography scan confirmed a type II popliteal entrapment syndrome with popliteal artery occlusion. The patient was submitted to surgery that consisted in myotomy of the medial head of the gastrocnemius muscle, division of the anomalous fibrous band, resection of the diseased popliteal artery and interposition of a reverse ipsilateral saphenous vein graft. The patient recovered distal pulse on the right foot.
Previously considered as a rare disease, the growing number of publications about PAES in the medical literature show the opposite. However, little is known about the prevalence of this syndrome and some studies report a prevalence of 0.165-3.5%. PAES is more common in males and in almost 60% is bilateral. The best treatment results are obtained with replacement of the popliteal artery with graft interposition, preferably venous. Currently, this approach is advocated in all patients with entrapment with the exception of early stages with arterial disease confined to the adventitia.
PAES is not as rare as previously admitted and therefore it is important to maintain a high index of suspicion in these age group.
Keywords: Entrapment; popliteu; poplíteo; isquemia do membro inferior; PAES;
RESUMO
A síndrome do entrapment da artéria popliteia (PAES) é uma causa importante de claudicação e isquemia aguda do membro inferior em jovens atletas sem fatores de risco para aterosclerose.
Apresentamos o caso de uma doente de 39 anos de idade, sem antecedentes pessoais relevantes e sem hábitos para a prática desportiva, que recorre ao serviço de urgência com queixas de claudicação incapacitante no membro inferior direito que se revelou consequente a uma oclusão da artéria popliteia. A análise da angio-TC confirma a suspeita diagnóstica da síndrome do entrapment popliteu do tipo II. A doente é submetida a miotomia da cabeça medial do gémeo, secção de uma banda fibrosa anómala, ressecção do segmento de artéria doente e interposição de veia safena interna ipsilateral e invertida. A doente recuperou pulsos distais no membro inferior direito.
A PAES é uma entidade patológica mais frequente do que previamente descrito, contudo, com uma taxa de prevalência ainda não bem definida. Alguns estudos reportam uma prevalência entre os 0.165% e 3.5%, sendo mais comum no sexo masculino e bilateral em quase 60% dos casos. O tratamento de escolha passa pela substituição da artéria popliteia com interposição de enxerto venoso. Atualmente, esta abordagem é defendida para todos os doentes com PAES, à exceção de estádios da doença mais precoces, com doença arterial confinada à sua adventícia.
Em conclusão, a PAES é uma síndrome mais prevalente que previamente reportado, sendo essencial um alto índice de suspeição para o seu diagnóstico em doentes jovens.
Palavras-chave: Entrapment; popliteu; poplíteo; isquemia do membro inferior; PAES;
Introduction
The popliteal artery entrapment syndrome (PAES) is a major cause of claudication and acute ischemia of the lower limbs in the younger population(1). This syndrome is often observed in athletes, with muscular hypertrophy, and without risk factors for atherosclerosis(1).
The present paper reports the case of a woman with popliteal entrapment syndrome observed primarily in the emergency setting.
Clinical Case
A previously healthy 39-years-old female was referred to our emergency department with a thirty-day history of disabling claudication and paresthesia of the right foot. At clinical examination, a decreased temperature of the foot with no motor compromise was observed. The right femoral pulse was normal with no palpable popliteal, tibialis and dorsalis pedis pulses. All contralateral pulses were normal. Duplex ultrasound revealed a retrogeniculate popliteal artery occlusion with monophasic flow in the infragenicular popliteal artery and leg arteries.
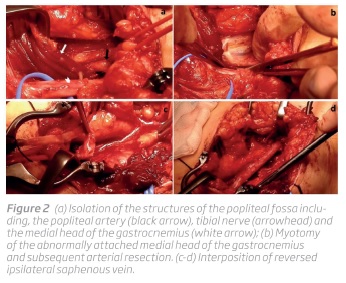
Given the complaints of the patient and the findings on clinical examination and duplex ultrasound, the patient was diagnosed with sub-acute ischemia of the right limb caused by popliteal artery thrombosis. Due to the absence of risk factors for atherosclerosis, a computed tomography angiography (CTA) was performed confirming a type II popliteal entrapment syndrome (Figure 1).
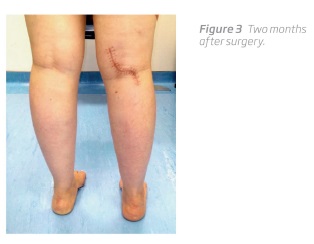
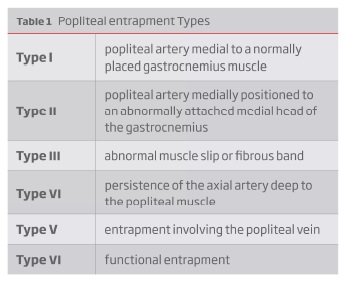
The patient was submitted to surgery, through a posterior approach, that consisted in myotomy of the medial head of the gastrocnemius muscle, division of the anomalous fibrous band, resection of the diseased popliteal artery and interposition of reverse ipsilateral saphenous vein (Figure 2 e 3). The procedure was uneventful, distal pulses were recovered on the right foot with no evidence of peripheral nerve damage.
Discussion
Popliteal artery entrapment was first described in 1879 by Anderson Stuart, a medical student in Edinburgh, after dissection of a popliteal aneurysm in an amputated limb for gangrene(2). However, that was not until 1959 that Hamming firstly reported the popliteal artery entrapment syndrome(3).
Previously considered as a rare disease, the growing number of publications in medical literature show that it is not so uncommon(1,4). Little is known about the prevalence of PAES(5). Some studies in the decades of 1970s and 1980s reported a prevalence between 0.165 and 3.5 percent(6,7).
A recent systematic review revealed a predominance of this condition in males with a median of 83% (22-100%) and a median age of 32 years (20.7-41 years)(8). Di Marzo et al reported that almost 60% of patients have bilateral popliteal entrapment(9).
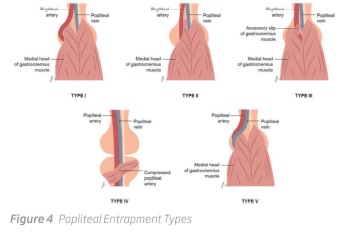
The popliteal entrapment is a complex pathological entity with multiple syndrome classification systems dispersed in the literature(10,11). Currently, the best accepted one is based on the embryological development of the popliteal region and, with some adaptations from the original classification, we can categorize PAES in 6 types (Table 1 and Figure 4)(12).
Popliteal entrapment classically manifests with intermittent claudication in young patients without risk factors for atherosclerosis(5). The presentation also includes symptoms such as leg cramps and tingling and decreased feet temperature(5). Usually, the patients are athletes, with muscular hypertrophy, being symptomatic after intense physical effort. A large pulse at rest and diminished or absent during the passive dorsiflexion or active plantar flexion of the foot is typical of this condition(5). Duplex ultrasound with dynamic maneuvers seems to be the commonest used initial exam, however with an unacceptable high false-positive rate (72%)(13). Although CT scan and MRI has been particularly useful to investigate popliteal entrapment (i.e., to study anatomic relationship of the artery with adjacent tissue, especially when the artery is occluded), angiography remains the mainstay test at many centers(12,14).
The pathophysiological process of the popliteal entrapment is different from atherosclerosis. The arterial wall injury processes in a centripetal way with fibrosis and collagen healing scar evolving from the adventitia (Stage I), subsequently the media (Stage II) and finally the intima (Stage III)(15). This explains why arterial thrombosis in these patients have poor prognosis with thrombolysis, angioplasty or thromboendarterectomy with patching(1,12,14). When the popliteal artery is occluded, the arterial wall is already so diseased that it should be replaced by a graft, preferably venous, instead of local reconstruction techniques.(1,12,14) Currently, this approach is advocated in all patients with entrapment and popliteal arterial wall disease(1,14). In early stages with minor arterial disease, confined to adventitia (i.e. Stage I), a more conservative approach is advised and simple muscular division is enough to correct the entrapment mechanism(1,14). This procedure usually involves the medial head of the gastrocnemius and/or the resection of abnormal muscle slips or tendinous bands. Stages II and III shall be managed not only by a surgical resolution of the entrapment mechanism, but also by the replacement of the diseased popliteal arterial segment(1,14).
In the clinical case discussed herein, although young, the patient is a female without sport or significant physical activity, that presented with sub-acute symptoms of intermittent claudication and a stage III of PAES with arterial thrombosis. The patient was managed through correction of the muscular defect and vein graft replacement of the popliteal artery via a posterior approach.
Levien et al described a success rate of 100% in 15 lower limbs subjected to replacement of the occluded segment with reversed saphenous vein with a median follow-up of 4.2 years (range 1 to 10)(1). The dichotomy between medial and posterior surgical approach has also been widely discussed in the literature(5,14,16) with the first being advocated by many as less invasive, enabling rapid recovery for patients usually young and athletics who value a fast return to full activity(5,14,16). Furthermore, this approach is more suitable for longer reconstruction segments. Posterior approach enable the exposure of all structures in the popliteal region, turning the procedure faster(5,14,16. It also allows the placement of shorter vein segments in an anatomic position and may allow a simpler, less extensive and more anatomic correction of the entrapment. One significant limitation of the posterior approach is a limited access to the distal popliteal artery and its branches what may be a problem in acute cases, with thrombosis and where an adequate thrombectomy is warranted.
Conclusion
The popliteal entrapment syndrome is not as rare as previously admitted among the medical community. PAES is a major cause of claudication and acute ischemia of the lower limbs in young people. Therefore, it is important to maintain a high index of suspicion in these age group to avoid to treat PAES as an atherosclerotic occlusive disease or an embolic acute ischemia of the lower limb.
REFERENCES
1. Levien LJ, Veller MG. Popliteal artery entrapment syndrome: More common than previously recognized. J Vasc Surg. 1999;30(4):587-598. DOI: 10.1016/S0741-5214(99)70098-4. [ Links ]
2. Stuart TP. Note on a Variation in the Course of the Popliteal Artery. J Anat Physiol. 1879;13(Pt 2):162. [ Links ]
3. Hamming JJ. Intermittent claudication at an early age, due to an anomalous course of the popliteal artery. Angiology. 1959;10:369-371. DOI: 10.1177/000331975901000505. [ Links ]
4. Di Marzo L, Cavallaro A, Sciacca V, Mingoli A, Stipa S. Natural history of entrapment of the popliteal artery. J Am Coll Surg. 1994;178(6):553-556. [ Links ]
5. Levien L. Popliteal artery entrapment syndrome. Semin Vasc Surg. 2003;16(3):223-231.http://www.sciencedirect.com/science/article/pii/S0895796703000280. [ Links ]
6. Gibson M, Mills J, Johnson G, Downs A. Popliteal Entrapment Syndrome. Ann Surg. 1977;185(3):341-348. [ Links ]
7. Bouhoutsos J, Daskalakis E. Muscular abnormalities affecting the popliteal vessels. Br J Surg. 1981;68(7):501-506. DOI: 10.1002/bjs.1800680720. [ Links ]
8. Sinha S, Houghton J, Holt PJ, Thompson MM, Loftus IM, Hinchliffe RJ. Popliteal entrapment syndrome. J Vasc Surg. 2012;55(1):252-262.e30. DOI: 10.1016/j.jvs.2011.08.050. [ Links ]
9. Di Marzo L, Cavallaro A. Popliteal vascular entrapment. World J Surg. 2005;29(SUPPL. 1):43-45. DOI: 10.1007/s00268-004-2058-y. [ Links ]
10. Kim HK, Shin MJ, Kim SM, Lee SH, Hong HJ. Popliteal artery entrapment syndrome: Morphological classification utilizing MR imaging. Skeletal Radiol. 2006;35(9):648-658. DOI: 10.1007/s00256-006-0158-5. [ Links ]
11. Hai Z, Guangrui S, Yuan Z, et al. CT angiography and MRI in patients with popliteal artery entrapment syndrome. Am J Roentgenol. 2008;191(6):1760-1766. DOI: 10.2214/AJR.07.4012. [ Links ]
12. Cronenwett JL, Johnston KW. Rutherfords Vascular Surgery. 8th ed. Philadelphia: Saunders Elsevier; 2014. [ Links ]
13. Akkersdijk WL, de Ruyter JW, Lapham R, Mali W, Eikelboom BC. Colour duplex ultrasonographic imaging and provocation of popliteal artery compression. Eur J Vasc Endovasc Surg. 1995;10(3):342-345. DOI: 10.1016/S1078-5884(05)80054-1. [ Links ]
14. Henry MF, Wilkins DC, Lambert AW. Popliteal artery entrapment syndrome. Curr Treat Options Cardiovasc Med. 2004;6(2):113-120. DOI: 10.1007/s11936-004-0039-y. [ Links ]
15. Levien L. Popliteal artery thrombosis caused by popliteal entrapment syndrome. In: Greenhalgh R, Powell J, eds. Inflammatory and Thrombotic Problems in Vascular Surgery. London: W. B. Saunders Co Ltd; 1997:159-168. [ Links ]
16. Hoelting T, Schuermann G, Allenberg JR. Entrapment of the popliteal artery and its surgical management in a 20-year period. Br J Surg. 1997;84(3):338-341. DOI: 10.1002/bjs.1800840321. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: tony.ramos.soares@gmail.com (T. Soares).
Acknowledgments
The authors thank designer Lucy Soares for the illustrations.
Ethical disclousures
Conflicts of interest: The authors declare that there is no conflict of interest regarding the publication of this article.
Protection of human and animal subjects: The authors declare that no experiments were performed on humans and animals for this study.
Confidentiality of data: The authors declare that no patient data appear in this article.
Right to privacy and informed consent: The authors declare that no patient data appear in this article.
Recebido a 28 de maio de 2017
Aceite a 15 de julho de 2018