Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.13 no.2 Lisboa jun. 2017
CASO CLÍNICO
Sindrome de may-thurner associado a um sindrome de nutcracker: caso clinico e revisão da literatura
May-thurner syndrome associated with nutcracker syndrome: clinical case and literature review
Miguel Machado1, Rui Machado1,2, Daniel Mendes2, Rui de Almeida1,2
1Instituto de Ciências Biomédicas Abel Salazar — Universidade do Porto;
2Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar Universitário do Porto
RESUMO
Introdução:
A Síndrome de May Thurner (SMT) resulta da compressão da veia ilíaca comum esquerda (VICE), entre a quinta vértebra lombar, posteriormente, e a artéria ilíaca comum direita (AICD), anteriormente. Este fenómeno pode causar estase venosa na pélvis e no membro inferior esquerdo. A Síndrome de Nutcracker (SNC) resulta da compressão da veia renal esquerda (VRE), entre a artéria mesentérica superior e a aorta, chamada SNC anterior, ou mais raramente pela compressão da VRE, entre a aorta e as vértebras lombares, quando a veia passa posteriormente à aorta, chamada SNC posterior. A associação das duas anomalias pode ocorrer quando existem veias renais circun-aórticas, chamado de SNC misto. Este fenómeno pode causar estase no rim e na pélvis. O SMTe o SNC são entidades clínicas raras e a associação das duas patologias é ainda mais rara.
Caso clínico:
Uma mulher de 29 anos recorre à consulta com dor nas pernas, predominantemente à esquerda, edema maleolar esquerda, com agravamento vespertino e dispaneuria. Estas queixas interferiam severamente com a sua qualidade de vida. O exame físico revelou varizes colaterais na face posterior esquerda, variz vulvar direita e edema maleolar esquerdo discreto. Realizou flebografia do sistema ilio-cava e da veia ovária, observando-se compressão da VICE pela AICD com extensa colateralidade, comunicando o sistema venoso ilíaco esquerdo e direito, origem da veia vulvar direita em ramo da artéria ilíaca interna direita e compressão da veia renal esquerda posterior pela aorta. Uma angioplastia transluminal percutânea com dilatação sequencial com balões de diâmetro 12, 14 e 16 mm foi efectuada, com posterior colocação de um stent optimed 16/100 mm na VICE. Aos 3 meses de follow-up, a doente informou que estava grávida, tendo suspendido a hipocoagulação com rivaroxabane, mantendo o uso de meia elástica. A gravidez e o pós-parto ocorreram sem intercorrências. Aos 12 meses de follow-up, foi realizado um TC que mostrou o stent em boa posição e patente e, posteriormente, foi submetida a fleboextração de varizes da coxa esquerda. Aos 18 meses de follow-up, a doente está clinicamente assimtomática.
Discussão/Conclusão:
Um insuficiente conhecimento da história natural da SNC e da SMT resulta de uma indefinição sobre os critérios de diagnóstico e indicação terapêutica, particularmente na rara associação destas duas síndromes. Esta pode ser responsável pela amplificação dos sintomas da obstrução venosa. No nosso caso clínico, observámos a resolução das queixas da doente, apenas com o tratamento da obstrução da VICE e não observámos nenhum efeito na estrutura e patência do stent iliocava com a gravidez.
Palavras-chave: Síndrome de Nutcracker, Síndrome de May-Thurner
ABSTRACT
Introduction
May Thurner syndrome (MTS), is a condition in which the left common iliac vein (LCIV) is compressed between the fifth lumbar vertebra, posteriorly, and the right common iliac artery (RCIA), anteriorly. This phenomenon can cause venous stasis in pelvis and in left lower limb. Nutcracker syndrome (NCS) is caused by compression of the left renal vein (LRV) between the superior mesenteric artery and the aorta, called Anterior NCS, or more rarely by compression of the LRV between the aorta and the lumbar vertebra, when the vein passes behind the aorta, called posterior NCS. The association of the two anomalies can occur when a circunaortic renal vein exists. This phenomenon can cause stasis in the kidney and in the pelvis. The MTS and NCS are rare clinical entities and the association of the two pathologies is extremely rare.
Clinical Case
A 29-year-old female, complaints of bilateral leg pain, predominantly on the left side, left malleolar edema which increases in the end of the day, and dyspaneuria. This complaint leads to severe quality of life deterioration. Physical examination reveals collateral varices in the posterior aspect of the left tight, a right side vulvar varicose vein and mild left malleolar edema. Phlebography of the ilio-cava system and the ovarian vein was performed revealing a compression of the LCIV by RCIA with an extensive collateral pathway communicating the left and right iliac vein system, the origin of a right side vulvar varicose vein in the right internal iliac vein and compression of a posterior LRV by the aorta. A transluminal angioplasty with sequential dilatation with 12, 14 and 16 mm balloon was done and an Optimed® sinus vein stent 16/100 mm was implanted in the LCIV. At 3 months of follow up, the patient became pregnant, so she stopped the rivaroxabane treatment and maintained the elastic therapy with compression stockings. The pregnancy and the childbirth had no intercurrences. An abdomino-pelvic control CT at 12 months follow-up was done, confirming the correct position and patency of the. Posteriorly, the patient was submitted to stab avulsion of varicose veins in the left thigh. At 18 months follow-up, the patient was clinically asymptomatic.
Discussion/Conclusion
Insufficient knowledge about the natural history of NCS and MTS results from the uncertainty in the diagnostic criteria and treatment selection, particularly in the rare association of both. This association can be responsible for the amplification of the symptomatology of the venous obstruction.
In our case, we have seen the resolution of the complaints by treating only one of the obstructive lesion (MTS) and we haven't seen any effect of the pregnancy in the structure and patency of the ilio-caval stent.
Keywords: Nutcracker Syndrome, May-Thurner Syndrome
INTRODUCTION
May Thurner syndrome (MTS), also known as Cockett syndrome or non-thrombotic iliac vein obstruction, is caused by compression of left common iliac vein (LCIV) between the fifth lumbar vertebra, posteriorly, and the right common iliac artery (RCIA), anteriorly. This phenomenon can cause stasis in the pelvis and in the left lower limb and is responsible from the increased incidence of deep venous thrombose (DVT) in this limb.(1) May and Thuner, in autopsy specimen studies, found intraluminal spurs in the mouth of LCIV in 22% of the subjects analyzed and proposed that they arosed from chronic intimal damage of the
LCIV secondary to the pulsatility of the RCIA. These lesions, as stated by McMurrich et al,(2) are acquired as he observed the absence of spurs in fetal autopsies. Nutcracker syndrome (NCS) can result from the left renal vein (LRV) compression between the superior mesenteric artery and the aorta, called Anterior NCS, or more rarely by compression of the LRV between the aorta and the lumbar vertebra, when the vein passes behind the aorta, called posterior NCS. The association of the two anomalies can occur when a circunaortic renal vein exists.
The MTS and NCS are rare clinical entities and the association of the two pathologies is extremely rare.(3) Depending on specific manifestations, MTS and NCS may be diagnosed by different medical specialists. We describe a clinical case of a patient with this two forms of venous entrapment.
CLINICAL CASE
A 29 year old woman, with two Childs, came to the vascular surgery appointment with complaints of bilateral leg predominantly on the left side, left malleolar edema which get worse at the end of the day, and dyspaneuria. This complaint leads to severe quality of life deterioration.
The patient had no history of varices in family, previous surgery or other medical comorbidities.
The physical examination reveals collateral varices in the posterior aspect of the left tight, a right side vulvar varicose vein and mild left malleolar edema.
The Doppler ultrasonography of the lower limbs was normal.
The patient was proposed to a phlebography of the ilio-cava system and ovarian vein.
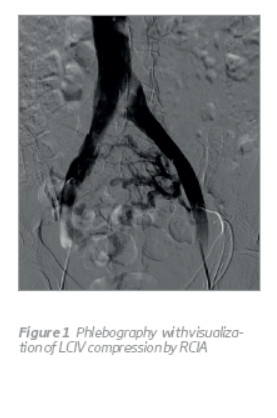
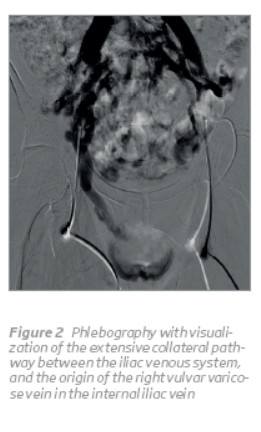
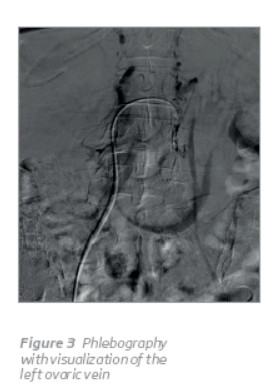
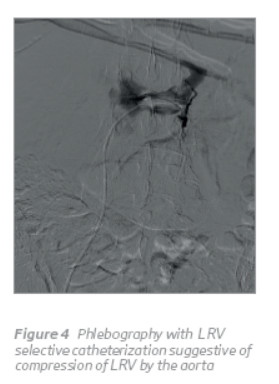
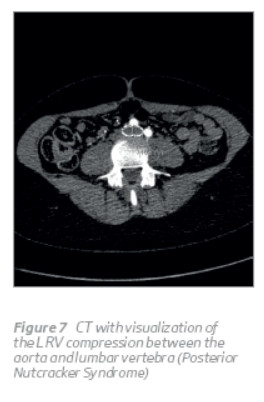
After informed consent, phlebography was performed under local anesthesia. Using the Seldinger technique, a 5-Fr vascular sheath was inserted in both common femoral veins. It reveals compression of LCIV by the RCIA (Figure 1) with an extensive collateral pathway communicating the left and right iliac vein system (Figures 1 e 2), the origin of a right side vulvar varicose vein in the right internal iliac vein (Figure 2) and the compression of a posterior LRV by the aorta (Figure 4). It was not possible a selective catheterization of the left ovarian vein (Figure 3).
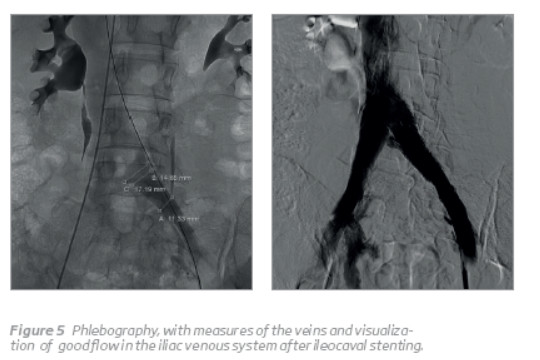
A Terumo® guide-wire and 5F cobra catheter were used to cross the compressed segment of the LCIV. After ensuring that the catheter was in the inferior vena cava, the patient was hypocoagulated with 5000-UI of unfractioned heparine and the Terumo® guide wire and the sheat were exchanged by a steef wire and a 10Fr sheat. A transluminal angioplasty (ATL) with sequential dilatation with 12, 14 and 16mm diameter balloon was done and, posteriorly, an Optimed® sinus vein stent 16/100 mm was inserted in the LCIV(Figure 5).
After the procedure, the patient remained with elastic stockings and sub cutaneous Low Molecular Weight Heparine and, in the following day, goes home with rivaroxabane 15mg bid and posteriorly 20mg daily. The patient was reexamined at 1 month, the vulvar varice had disappeared and had no complaints. At 3 months of follow up, the patient called and informed that she was pregnant, so she stopped the rivaroxabane and maintained the elastic stockings. The pregnancy and the childbirth had no intercurrences.
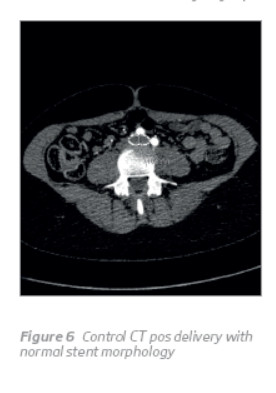
She was reexamined 6 months later and complained about aesthetical problems reguarding collateral varices in the left thigh. An abdomino-pelvic control CT at 12 months follow-up was done, confirming the correct position and patency of the stent, without impact of the pregnancy on stent (Figure 6), and confirmed the posterior NCS (Figure 7). She was submitted to stab avulsion of the varices in the left thigh posteriorly. At 18 months follow-up, the patient was clinically asymptomatic.
DISCUSSION
MTS and NCS are rare individual clinical entities and their coexistence is even rarer.(3)
In a literature review, Quevedo H C et al(4) found 297 citations of NTS/NTP, 285 of them were based on single case reports. The prevalence of NCS is unknown but it appears to be under-diagnosed. It can be more frequent in females and the diagnoses can be made at any age, particularly in the second and third decades of life. The compression of the LRV causes renal venous hypertension and development of collateral pathways with venous congestion in the affected areas. The common clinical manifestations were micro or macro haematuria, proteinuria, flank or abdominal pain, pelvic congestion syndrome (with dyspaneuria, dysmenorrhoea, post coital ache and lower abdominal pain) and a chronic fatigue syndro
A lower BMI has also been associated with NCS. The diagnosis of NCS can be done by ultrasonography who has a sensivity of 78% and a specifity of 100%,(5) but both computed tomography (CT) and magnetic nuclear resonance (MRA) are becoming the diagnostic tools of choice.
(6) The phlebography, which is the gold standard, can show the image of compression, the collateral venous circulation and allows measure the pressure gradient between the renal vein and the vena cava.(7) However, there are not, at the moment, credible tests to confirm the hemodynamic significance of a venous stenosis. The treatment of NCS remains controversial, with various options. Some authors refer a high rate of spontaneous remission, particularly in young patients, so surveillance during two years can be a good option in mild symptomatic patients. A great variety of surgical options are available to decrease the pressure in the renal vein. In the open surgery, the transposition of the renal vein further down in the IVC is the first option(8) (9) but auto transplantation of the affected kidney into the iliac fossa can be a good alternative.(6) (10) (11) This technic has been done by Stocker et al with positive results(12) and is general used as last alternative to nephrectomy when, after LRV transposition, the hematuria persists. The transposition of the superior mesenteric artery caudally in the aorta is rarely done since the consequences of thrombosis can be devastating.(13) Gonadal caval bypass has been described and can be especially interesting in patients with congestion pelvic syndrome and extensive pelvic varices, however the results are discouraging.(13) The development of endovascular surgery as minimal invasive alternative can be a great solution but the results at long term follow up are missing. The first case of stenting of the LRV was done by Neste MG et al,(14) in 1996. Chen S et al has published the biggest study about stenting of NCS (61 patients) and had a success rate of 96,7%. The only major complication was solved by conventional surgery (1,6%) and this treatment has gained popularity.(15)
The MTS typically affects young and middle age women(16) and the compression of the LCIV causes venous hypertension in the left lower limb and in the pelvis. Clinically, the syndrome can be diagnosed in the non-complicated fase (compression of the LCIV only) and in the complicated fase (acute ilio-femoral venous thrombosis or later as a pos-thrombotic syndrome) Common clinical manifestations of non-complicated MTS are limb swelling, pain, venous claudication, varicose veins, hiperpigmentation, ulceration and, rarely, as a clinical manifestation of a pelvic congestion syndrome. The non complicated phase is the ideal moment to diagnose the syndrome, as we can avoid the development of deep venous thrombosis and the acute risk of pulmonary embolism and later development of pos-thrombotic syndrome in the obstructive or refluxive form. In the diagnosis of MTS, the Doppler ultrasonography has great interest in the exclusion of infra-inguinal venous pathologies (the most frequent illness) but the capability to study the venous iliac system is limited, with 20% of the studies being non diagnostic in the best vascular laboratories. Computed tomography (CT) and magnetic resonance nuclear (MRN) are becoming the imaging modalities of choice and can show the direct compression of the LCIV by the RCIA and the venous collateral circulation. It can also exclude other extrinsic compressions of the veins by tumors, hematomas or retroperitoneal fibrosis. A study of 36 patients with confirmed MTS on CT or MRN found a 23% mean change in LCIV compression within six months (12% decreased — to 69% increase) due to patient hidratation and positioning.(17) Despite the implicated role of extrinsic compression of the iliac veins in this disease, Meisner R J et al, comparing asymptomatic and advanced MTS, did not find statistically significant area reduction of the LCIV between the two groups.(18) The intra vascular ultrasonography (IVUS) is becoming increasingly useful in the clarification of the characteristics of the venous lesions. Forauer et al(19) referred that IVUS interferes with his vascular practice in 50% of the patients treated and IVUS has revealed an increasing utility in the diagnosis of MTS.(20) Multiple surgical approaches have been described when medical therapy fails to control symptoms of MTS. The Palma crossover bypass, the reposition of the RCIA behind the LCIV and vein patch angioplasty with intraluminal band excision can be done with a success rate between 40 and 80%. The development of endovascular surgery as minimal invasive alternative has become very popular in the latest years in the treatment of the venous ilio-cava obstruction and made a great revolution in the treatment of venous disease. With this approach, primary patency rates of 66% with a mean follow up of 3 years, complication rates inferior to 2%(21) (22) (23) (24) and better patency in the non complicated MTS were reported, with stenting occlusion occurring only in the pos-thrombotic syndrome. Kaichuang Ye et al(25) reported a serie of 205 patients with MTS treated by stenting with a technical success rate of 100%, a primary and assisted primary cumulative patency rates, at a means of 4 years, of 98,7 and 100%, respectively, edema relief of 89,1% and a healing rate of active ulcers of 82,3%. Osman Ahmed et al,(26) in a recent review about stenting in MTS, published a technical success rate of 100%, no major complications, 5% of minor complications and a positive correlation between the female gender and congestive pelvic symptoms.
One of the major problems of stenting vein pathology is the frequent young age of the patients and the uncertainty of the durability of this kind of devices. In our clinical case, the severity of the clinical symptomatology can be increased by the simultaneous compression of the LRV by the Aorta and the compression of the LCIV by the RCIA. The therapeutic option to stenting the LCIV compression is based in our long and positive experience in the endovascular treatment(27) of MTS. Unfortunately, we haven´t measured the ilio-caval and reno-caval pressure gradient. To our concern, the patient got pregnant and had to suspend hypocoagulation. The birth was uneventful and the patient remained asymptomatic at 18 months of follow up. In the control CT, we confirmed that no adverse effects occurs in stent by the pregnant uterus. The rarity of the clinical case, NCS associated with MTS, was confirmed by the fact that we only found one case published in the literature.(3)
CONCLUSION
Insufficient knowledge about the natural history of NCS and MTS results from the uncertainty in the diagnostic criteria and treatment selection, particularly in the rare association of both. This association can be responsible for the amplification of the symptomatology of the venous obstruction. In our case, we have seen the resolution of the complaints by treating only one of the obstructive lesion (MTS) and we haven't seen any effect of the pregnancy in the structure and patency of the ilio-caval stent.
REFERENCES
Virchow, R. Uber die Erweiterung kleiner Gefasse. Arch Path Anat. 1851, Bd. 3, S. 427. [ Links ]
McMurrich, JP. The occurrence of congenital adhesions in the common iliac veins and their relation to thrombosis of the femoral and iliac veins. Am J Med Sci. 1908, Bd. 135, S. 342–6. [ Links ]
Kurklinsky, A und Shepherd, A. A case of combined nutcracker and May-Thurner syndormes in an adult with resolution of hemodynamic findings. Presented at XVI World Meeting of the International Union of Phlebology. August31-September4, 2009, Bd. GE3, S. 7–10. [ Links ]
Quevedo, Henry C., Arain, Salman A und Tafeh, Nidal Abi. Systematic review of endovascular therapy for nutcracker syndrome and case presentation. Cardiovascular Revascularization Medicine. 2014, Bd. 15, S. 305–307. [ Links ]
Takebayashai, E, et al. Diagnosis of nutcraker syndrome with colour doppler sonography: correlation with flow patterns on retrograde left renal venography. Am J Roentenol. 1999, Bd. 172(1), S. 39–43. [ Links ]
Shokeir, AA, El-Diasty, TA und Ghoneim, MA. The nutcraker syndrome: new methods of diagnosis and treatment. Br J Urol. 1994, Bd. 74(2), S. 139–43. [ Links ]
Beinart, C, et al. Left renal to inferior vena cava relationship in humans. J Urol. 1982, Bd. 127, S. 1070–1. [ Links ]
Hohenfellner, M, et al. Nutcraker syndrome: a review of aspects of pathophysiology, diagnosis and treatment. J Urol. 1991, Bd. 146, S. 685–8. [ Links ]
Pastershank, SP. Left renal vein obstruction by a superior mesenteric artery. J Can Assoc Radiol. 1974, Bd. 25, S. 52–4. [ Links ]
Correio eletrónico: miguelvbmachado@gmail.com (M. Machado).














