Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.14 no.3 Coimbra set. 2020
CASE REPORT/CASO CLÍNICO
A very unusual presentation of endometrial cancer relapse
Uma apresentação muito rara de metastização de carcinoma do endométrio
Catarina Vieira1, Bárbara Ribeiro2, Catarina Pardal2, Carla Monteiro2, Paula Serrano3
Hospital de Braga
1 Interna de Formação Específica de Ginecologia e Obstetrícia, Departamento de Ginecologia e Obstetrícia, Hospital de Braga
2 Assistente Hospitalar de Ginecologia e Obstetrícia, Departamento de Ginecologia e Obstetrícia, Hospital de Braga
3 Assistente Hospitalar Graduada de Ginecologia e Obstetrícia, Departamento de Ginecologia e Obstetrícia, Hospital de Braga
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Endometrial cancer is a frequent gynaecological malignancy, generally associated with good prognosis. Common metastasis sites include lungs, liver and lymph nodes, but not the abdominal wall.
A 51-year-old patient, with endometrioid endometrial adenocarcinoma was submitted to hysterectomy and bilateral adnexectomy. Histopathology confirmed FIGO stage IA and absence of lymphovascular invasion. A year later, a suspicious lesion ’s biopsy in the abdominal wall revealed a metastasis of the primary cancer, which was removed.
In spite of low risk factors for relapse, the patient developed a rare metastasis site. This emphasises the necessity of close surveillance and high level of suspicion for diagnosis.
Keywords: Neoplasm metastasis, Endometrial neoplasms, Early detection of cancer.
Introduction
Endometrial cancer is the most common gynaecological cancer. There are several histological subtypes, being the endometrioid the most frequent and the one associated with better prognosis. Most cases present in post-menopausal women, with abnormal uterine bleeding, and thus can be diagnosed at an early stage and, consequently, have a more favourable prognosis, with high survival rates1,2.
About 21% may present with spread to regional organs and lymph nodes and 8% with distant metastasis2. Others can develop metastasis after the primary treatment, which is more common in the first years of follow-up2. The most common recurrence sites are the vagina, pelvic and para-aortic lymph nodes, peritoneum and lungs. Abdominal wall metastasis of endometrial cancer are not typical.
Given the rare presentation of endometrial cancer metastasis and the challenges it can present in its management, it is of the uttermost importance to share this clinical case with the scientific community.
An informed consent was obtained from the patient prior to the elaboration of this article.
Clinical case
A 51-year-old post-menopausal female patient, with dyslipidaemia and heterozygous Factor V Leiden mutation and hyperhomocystenemia, refered to the gynaecologic department for persistent vaginal bleeding, was submitted to an histeroscopic endometrial biopsy that revealed an endometrioid adenocarcinoma. The initial workup (transvaginal ultrasound, pelvic magnetic resonance imaging and thoracic radiography) excluded advanced or metastatic disease; CA 125 was normal (18,10 U/mL).
The patient was submitted to an abdominal hysterectomy and bilateral adnexectomy (infra-umbilical medial section and no drain left in the pelvis) with frozen section of the uterus and adnexa confirming FIGO stage IA. Therefore, the pelvic and para-aortic lymphadenectomy were not performed. The surgical specimen revealed absence of lymphovascular invasion, classifying the neoplasia as a ESGO/ESMO/ESTRO low risk endometrial cancer, and no adjuvant treatment were performed. She maintained clinical surveillance in Gynaecologic Oncology consultation in our hospital since then, and a year after the diagnosis the patient developed abdominal wall pain and went to the emergency room, having been diagnosed with an infected abdominal rectus sheath hematoma, with 120 x 71mm, which was drained. In the hospital admission, she later developed a bilateral pulmonary thromboembolism, thus having been medicated with anticoagulants. Two months later, she kept complaining of persistent abdominal pain .
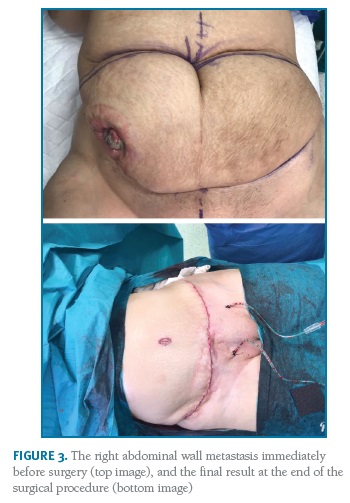
To evaluate the persistent abdominal pain, an abdomino-pelvic computed tomography (CT) scan was done. It showed a suspicious lesion in the muscular planes of the right abdominal wall, with 83 x 56 mm, with heterogenous central hypodense areas and local contrast captation in the periphery (Figure 1).
(clique para ampliar ! click to enlarge)
Given the oncological history of the patient, it was necessary to obtain a sample tissue for histological evaluation to exclude a metastasis. The lesion was submitted to biopsy, which revealed a metastasis of an adenocarcinoma, compatible with the previously diagnosed primary endometrial cancer.
The persistent abdominal pain could translate another possible haemorrhagic complication (hematoma), since the patient was under anticoagulants, or an infectious one. It was also necessary to exclude early metastasis of endometrial adenocarcinoma, given the patient’s history. An abdomino-pelvic CT-scan is useful in the evaluation of these differential diagnoses, including common possible sites of metastasis, for instance liver or lymph nodes.
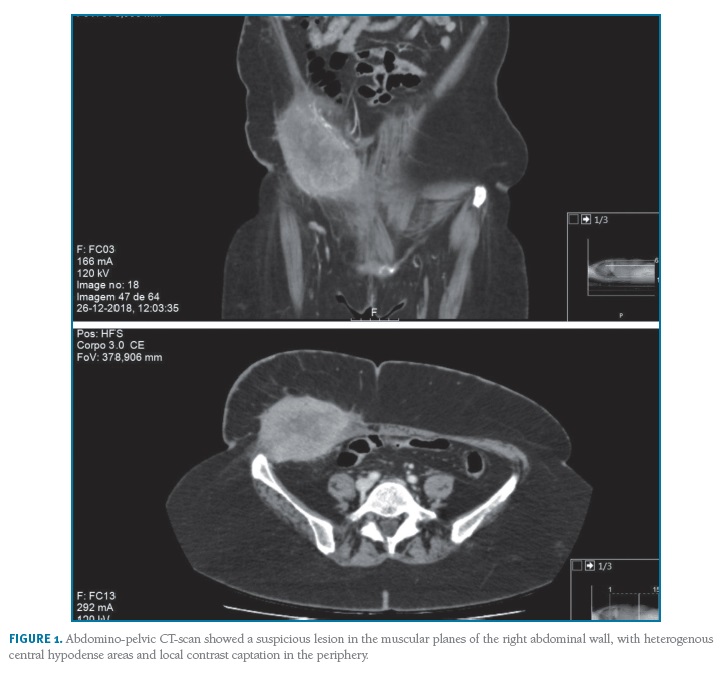
The patient was evaluated by a multidisciplinary team (oncologic gynaecologist, medical oncologist, radiologist, radiotherapist and plastic surgeon) and a radical surgical approach was decided. It was performed an arciform suprapubic and supraumbilical incisions, detachment of the subcutaneous cellular tissue on the left, and bloc removal of the peritoneum, aponeurosis, rectus and external oblique muscles, iliac crest on the right, and subcutaneous cellular tissue and skin bilaterally. There was no evidence of macroscopic disease elsewhere in the abdominal cavity.
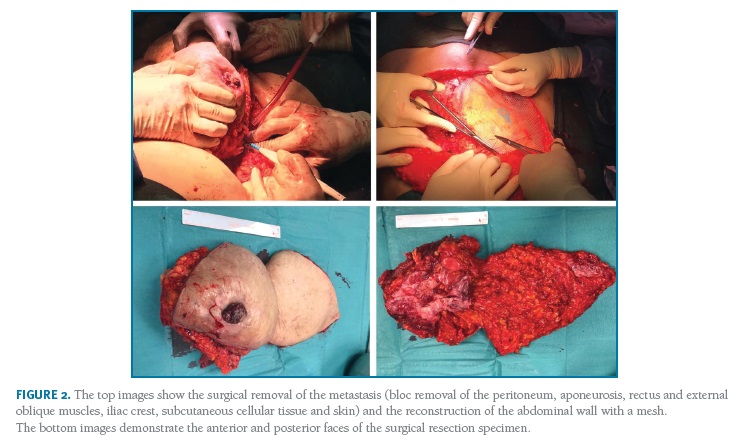
The abdominal wall was reconstructed with a doubled-face monofilament polyester composit mesh and an umbilical transposition was performed (Figures 2 and 3).
(clique para ampliar ! click to enlarge)
In the post-operative period, the patient developed an operative wound infection, with isolation of multiple bacteria (Corynebacterium amycolatum, pseudomonas aeruginosa, staphylococcus epidermidis), having been medicated with intravenous antibiotics. She had a good recovery and was discharged after 23 days. She then maintained surveillance in the outpatient consult, with regular wound dressing care. The wound is currently completely closed.
The final histological result of the surgery showed skin, subcutaneous cellular tissue and muscular neoplastic involvement, with the same characteristics as the primary tumour.
The multidisciplinary oncologic group decided to perform radiotherapy. It included a total dose of 45 Gray (Gy) in 14 daily 1,8Gy fractions, and an additional boost of 5,4Gy in 3 daily 1,8Gy fractions.
The patient has 14 months of follow-up since the abdominal wall metastasis with no sign of recurrence/persistence of disease to date.
Discussion
Endometrial cancer is the most common gynaecological cancer. Most of the cases present in an early stage, especially the endometrioid histological subtype. The clinical case reported here supports this, since our patient was diagnosed with a FIGO IA, grade 2, endometrioid endometrial cancer1,2. The surgery, which consisted of an abdominal hysterectomy and bilateral adnexectomy, was performed with a curative purpose.
Given the low risk of lymph node involvement (<5%), lymphadenectomy is not recommended for patients with low-risk endometrial cancer3,4.
Sentinel lymph node dissection is not yet recommended by international guidelines remaining experimental, therefore is not done in our institution3.
The American College of Obstetricians and Gynaecologists (ACOG) affirm that several randomized trials have demonstrated that adjuvant radiation for certain stage I or stage II endometrial carcinomas reduces the local recurrence rate but does not affect overall survival5. National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology 2018 recommends observation or vaginal brachytherapy after surgery in IA with less than 50% myometrium invasion with no additional risk factors of recurrence6. The American Society of Clinical Oncology (ASCO) states that surveillance is a reasonable option for women without residual disease in the hysterectomy specimen and for women with grade 1 or 2 cancer and < 50% myometrial invasion, especially when no other high-risk features are present7.
Factors that could increase the risk of relapse include age (more than 60 years old), serous, clear-cell, carcinosarcoma or carcinofibroma histological types, grade 3, invasion of the outer myometrium, tumoral extension beyond the uterine body, lymphovascular invasion, lymph node metastasis and tumour with more than 2cm in size1. Our patient did not present any of these risk factors, and still had an early (1 year) relap se8.
The information in the literature about abdominal wall metastasis of endometrial cancer is sparse. Saudi Arabian authors have published in 2017 a case report about a metastatic endometrial carcinoma at the repair site of an abdominal wall incisional hernia in a 55-year-old woman 4 years after surgical treatment of endometrioid adenocarcinoma of the endometrium. The lesion was surgically removed and the patient remained without metastatic recurrence at 12-month follow-up9. In our case, the recurrence was not located in the incision site but lateral to the abdominal rectus muscle, and no drain was left in the pelvis when abdominal hysterectomy and bilateral adnexectomy was performed.
A Chinese study focused on the FDG PET/CT findings of an isolated abdominal wall metastasis of endometrial adenocarcinoma 4 years after primary surgery in a 51-year-old woman10. Another case report from the United States of America hypothesized a possible role of laparoscopic surgery port-sites in endometrial cancer metastasis, after a 78-year-old patient developed a metastasis in the former port-sites 1 year after surgical treatment for a IB grade 3 endometrial adenocarcinoma11. A slightly different 2018 case report from Turkish authors showed a chest wall metastasis in a 57-year-old woman with endometrioid-type adenocarcinoma of the endometrium 8 years after the initial diagnosis, which was excised without complications 12.
Thus, abdominal wall metastases of endometrial cancer are rare, and there is not a sufficient number of cases published in the literature, which makes the treatment and orientation of these patients more challenging.
In this particular case, it was crucial to involve multidisciplinary collaboration (Gynaecology and Plastic Surgery), to achieve a good esthetical result and improve the patient’s prognosis, since it was possible to remove the single metastasis in its entirety. This case also emphasises the importance of keeping close surveillance on these patients and a high level of suspicion for early diagnosis of rare metastasis sites.
REFERENCES
1. Sociedade Portuguesa de Ginecologia. Cancro ginecológico - Consensos Nacionais 2016. Lisboa: Sociedade Portuguesa de Ginecologia; 2017 [ Links ]
2. Plaxe S, Mundt A. Overview of endometrial carcinoma [internet]. [Updated April 2019]. Available from: https://carcinoma?search=overview%20endometrial%20cancer&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. [ Links ]
3. Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J et al. ESMOESGO-ESTRO Consensus Conference on Endometrial Cancer: diagnosis, treatment and follow-up. Annals of Oncology 27: 16-41, 2016 DOI: 10.1093/annonc/mdv484.
4. Cohn D. Endometrial carcinoma: Staging and surgical treatment [internet]. [Updated August 2019]. Available from: https://carcinoma-staging-and-surgicaltreatment?search=endometrial%20cancer%20lymph%20node%20metastasis&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2#H1524131402 [ Links ]
5. American College of Obstetricians and Gynecologists. Endometrial cancer. Practice Bulletin No.149. Obstet Gynecol 2015;125:1006-1026. [ Links ]
6. Koh W, Abu-Rustum NR, Bean S, Bradley K, Campos S, Cho KR et al. Uterine Neoplasms, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology. Journal of the Comprehensive Cancer Network. 2018; DOI: 10.6004/jnccn.2018.0006.
7. Meyer LA, Bohlke K, Powell MA, Fader NA, Franklin GE, Lee J et al. Postoperative radiation Therapy for Endometrial Cancer: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Society for Radiation Oncology EvidenceBased Guideline. 2015 Sep 10;33(26):2908-13. Published Online First: 6 July 2015. DOI: 10.1200/JCO.2015.62.5459.
8. Colombo N, Creutzberg C, Amant F, Bosse T, Gonzáles-Martín A, Ledermann J et al. ESMOESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, treatment and followup. Ann Oncol. 2016;27(1):16-41. [ Links ]
9. Meshikhes AN, Al-Badr SH, Sulais EA. Late metastatic endometrial carcinoma at the repair site of an abdominal wall incisional hernia. Saudi Med J. 2017;38(5):546-548. DOI: 10.15537/smj.2017.5.17395. [ Links ]
10. Shen G, Ma H, Wan Y, Su M, Kuang A. FDG PET/CT findings of an Isolated Abdominal Wall Metastasis of Endometrial Carcinoma 4 Years After Primary Surgery. Clin Nucl Med. 2017;42(6):473-474. DOI: 10.1097/RLU.0000000000001600. [ Links ]
11. Nguyen ML, Friedman J, Pradhan TS, Pua TL, Tedjarati SS. Abdominal wall port site metastasis after robotically staged endometrial carcinoma: A case report. Int J Surg Case Rep. 2013;4(7):613-5.DOI: 10.1016/j.ijscr.2013.04.006. [ Links ][publishedOnline First:18April2013].
12. Dilek ON, Gür EÖ, Acar T, Aydoğmu. Chest wall metastasis of endometrial cancer: case report and review of the literature. Acta Chir Belg. Published Online First: 12 February 2018. DOI: 10.1080/00015458.2018.1438557.
Endereço para correspondência | Dirección para correspondencia | Correspondence
Catarina Vieira
E-Mail: catarina.cv.16@gmail.com
Recebido em: 28/05/2020. Aceite para publicação: 22/06/2020.