Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Obstétrica e Ginecológica Portuguesa
versión impresa ISSN 1646-5830
Acta Obstet Ginecol Port vol.13 no.4 Coimbra dic. 2019
CASE REPORT/CASO CLÍNICO
Pseudoangiomatous stromal hyperplasia of the breast: an unusual indication for mastectomy
Hiperplasia estromal pseudo-angiomatosa da mama: uma indicação rara para mastectomia
José Alberto Fonseca-Moutinho1, Bárbara Bizzo Castelo2, Ramona Carvalho Barros3, Helena Garcia4
Maternidade Daniel de Matos
Centro Hospitalar e Universitário de Coimbra
1 Auxiliary Professor of Health Sciences Faculty of Beira Interior University and Medical staff of Cova da Beira University hospitalar Center, Portugal
2 Medicine Student at Health Sciences Faculty of Beira Interior University, Portugal and Medicine Student of Pará University, Brasil
3 Medicine Student at Health Sciences Faculty of Beira Interior University, Portugal and Medicine Student of Juiz de Fora Federal University, Brasil
4 Medical staff of Pathology Department of Coimbra University Hospitalar Center, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Pseudoangiomatous Stromal Hyperplasia (PASH) is a benign proliferation of the mammary stromal tissue. We present a clinical case of a 74-years-old patient presenting a fast-growing PASH, treated through mastectomy, with no recurrence or breast cancer after a 11-years follow up. The patient’s clinical history, imaging, histopathologic examinations, treatment, and follow up were reviewed, along with 9 other cases described in literature. Considering that PASH is a condition that needs removal through an excision with safe margins, in case of fast-growing or large lesions, mastectomy seems to be a safe long-term treatment, with low risk of relapses or contralateral breast pathology.
Keywords: Breast, Pseudoangiomatous Stromal Hyperplasia, Mastectomy.
Introduction
Pseudoangiomatous stromal hyperplasia (PASH) is a breast proliferative lesion, with benign development and it was first described in 1986 by Vuitch et al1. PASH is usually a slow-growing mass and appears like a solitary, firm, painless, palpable, well-circumscribed and freely mobile breast mass and occasionally has a diffuse presentation2. These tumors are classified into either simple or fascicular/proliferative subtypes. Generally, PASH can be recognized on ultrasonography as a well-defined, homogenous, hypoechoic mass. On radiology PASH does not show specific features and can mimic fibroadenomas, hamartomas or angiosarcomas, besides largest tumors can be mistaken for Phyllodes tumor3,4. Definite diagnosis of PASH requires histopathologic evaluation. The etiology of this condition is not well understood, though some authors have suggested a hormonal cause1,5,6. Many of the patients diagnosed are premenopausal, and some evidences show an association with the use of hormones for contraception or as hormonal replacement therapy3,6. Several lesions show positive progesterone receptor status and this evidence may support the hormonal theory. Pruthi et al. reported a case of one patient treated with Tamoxifen, with good results7. In case of large tumorous PASH or when there is not a definite verdict from the biopsy, the recommended treatment is a wide local excision1. When the lesion is larger, fast-growing, or when it recurs, it may require mastectomy8.
PASH is not an uncommon finding: up to 23% of the specimens show little foci of PASH, in both benign and malignant breast lesions2. Nevertheless, we seldom have a discrete mass with the histopathologic features of PASH: only a few more than a hundred cases are reported in literature, usually with a benign clinical course and good long-term prognosis, with rare malignant progression. However, some authors believe that malignant lesions (myofibroblastoma or even sarcoma) might develop from PASH9. Literature reports also some cases of PASH in male patients10
Case Report
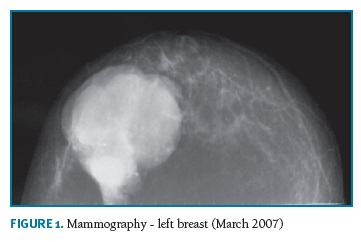
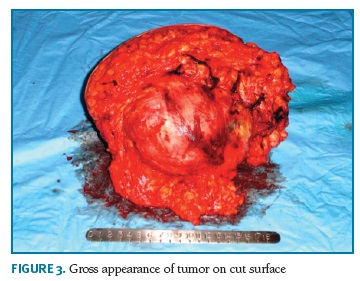
A 74-years-old woman, who has provided her written informed consent, caucasian, menopause at 50 years and was never treated with hormone replacement therapy or contraceptive pills, with past history of myocardial infarction, hypertension and obesity, in March 2007 noticed a tumor in the left breast with 4 cm in largest diameter. At that time, she recurred to Obstetrics and Gynecology Department in Cova da Beira University Hospital Center. Mammographic findings suggested benignity of the lesion (Fig. 1) and a biopsy was performed. Pathologic diagnosis was not definite, suggesting the diagnosis of fibroadenoma or phylloides tumor. The patient refused any further biopsy or surgical treatment. In November 2007, she returned to the same Department with a large 20 cm breast tumor (Fig. 2). A new breast core-biopsy was performed and a pathologic diagnosis of malignancy was excluded. Then, the patient accepted left total mastectomy as the best treatment (Fig. 3).
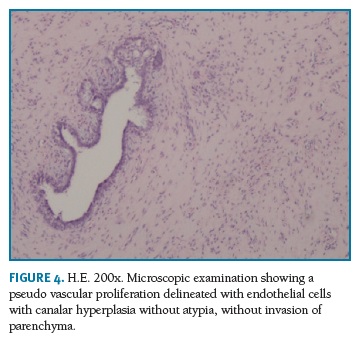
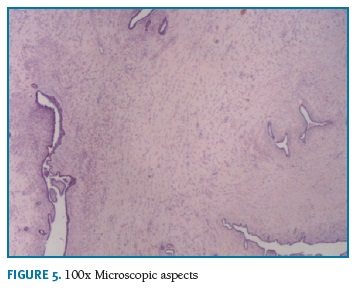
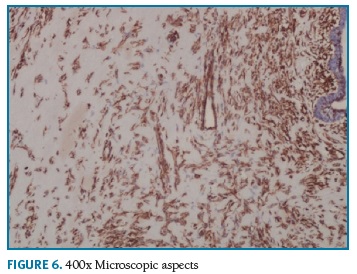
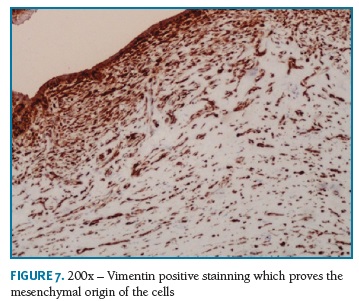
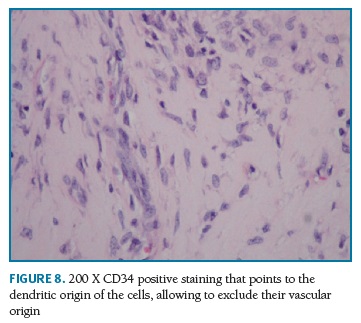
Definitive pathologic diagnosis of Pseudoangiomatous Stromal Hyperplasia (Fig. 4-5-6-7-8) was made on surgical specimen of mastectomy. The patient had regular follow-up at our department. Last visit was in May 2018, and no signs recurrence or contralateral breast cancer were diagnosed in those 11 years of follow-up.
Discussion
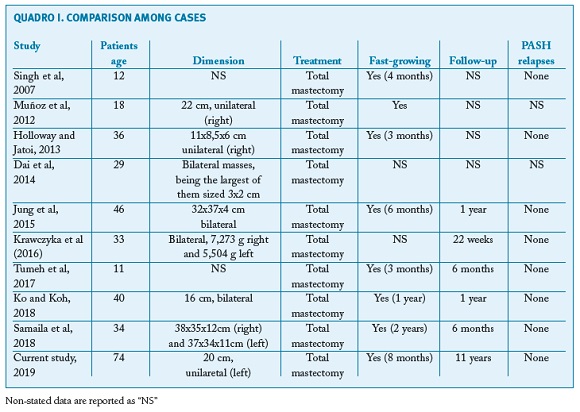
In reviewing literature, we found 9 other cases of PASH treated through mastectomy (Table 1).
Ko and Koh (2018)11 reported the case of a 40-year-old woman who developed a progressive bilateral breast enlargement for approximately 1 year. Mammography was inconclusive, but breast ultrasonography (US) showed a heterogenous, hypoechoic, and circumscribed mass measuring approximately 16 cm at the largest diameter in each breast. A bilateral mastectomy was performed because of the extent of the lesions and pain symptoms. The microscopic of surgical specimens led to the diagnosis of PASH, supported by immunohistochemical studies. The postoperative period was uneventful for 1 year of following-up.
Additionally, Samaila et al (2018)12 reports the case of a 34-year-old woman with a 2 year history of rapid progressive painless bilateral enlargement of the breasts. The examination revealed bilateral nontender giant breasts extending to the umbilical area with masses which were not attached to overlying skin and Grade 2 pressure ulcers on the lateral posterior breast aspects bilaterally. A bilateral mastectomy was performed and it revealed giant PASH which was confirmed by the positive immunohistochemical reactivity for CD34 and vimentin. No other breast pathologies were seen with extensive sectioning.
According to Tumeh et al (2017)13, a 11-years old patient presented a history of excessive breast growth in 3 months. She was assessed by the mastology team and released for a reduction surgery, however, during the intraoperative period it was observed that the breast tissue presented an anomalous appearance, diffusely infiltrated, white-grayish and fibroelastic, without cleavage planes. It was decided to perform a total mastectomy. The anatomopathological study showed absence of malignancy and the immunohistochemical study showed a profile compatible with bilateral PASH.
Krawczyka et al (2016)14 shows a case of a 33-year-old woman at 14 weeks of her first pregnancy, presenting a massive bilateral breast enlargement. Bilateral diagnostic biopsies showed diffuse PASH of both breasts, plus an ultrasound revealed increased breast density with pronounced lymphoedema, without local lymphadenopathy. Due to rapid progression of the macromastia, a bilateral skin-sparing mastectomy with immediate reconstruction was performed at 16 weeks of pregnancy. Bilateral mastectomy specimens were removed. Histological tissue examination revealed typical characteristics of PASH-like stromal hyperplasia The further course of pregnancy was uneventful.
The fifth case analyzed, published by Jung et al (2015)15, presents a patient with a bilateral diffuse lesion, in which the histologic examination of the specimens after mastectomy showed characteristic features of diffuse PASH. After a 12-month follow-up the patient didn’t have any relapses.
Similarly, the case reported by Dai et al (2014)16 presents a rare case of diffuse tumorous PASH involving bilateral breasts, clinically similar to a malignant lesion. The patient presented a one-year history of bilateral breast enlargement and asymmetry. Physical examination revealed multiple palpable nodule in bilateral breasts. Biopsy of the breast nodules demonstrated a diagnosis consistent with PASH. The stromal cells were positive, at the immunohistochemical staining, for estrogen receptor (ER) and progesterone receptor (PR) and negative for CD31, supporting the diagnosis of PASH. A bilateral mastectomy was performed, with immediate reconstruction.
Holloway and Jatoi (2013)17 reported the case of a 3-month history of progressive, rapid enlargement of the right breast. The diagnosis was PASH, with no evidence of malignancy. Besides, the growth was very rapid. The patient underwent a total mastectomy and immediate breast reconstruction. The patient had an excellent clinical and cosmetic outcome.
Muñoz et al (2012)18 presents two case reports: two adolescents (13 and 18 years old) in which rapidly growing masses demonstrated a histopathological result of PASH. Both masses were rapidly growing so they needed to be removed: in the former case through an excision, in the latter through a mastectomy. The study doesn’t refer relapses.
The oldest case within our literature research, reported by Singh et al (2007)8, corresponds to a 12-year-old girl with a 4-month history of bilateral breast enlargement. Right breast biopsy revealed PASH. Initially, surgical excision was performed. However, the lesion was resistant to surgical excision and it required bilateral mastectomies.
The current study reports the case of the oldest patient so far, suggesting that even in menopause PASH should be a differential diagnosis in women with breast tumor. Menopause seems not to change PASH behavior, since the speed of growth was similar to the cases of younger women. Furthermore, a long follow-up (11 years), without recurrence or other breast pathoogy suggests that PASH probably does not have breast cancer risk even in menopausal women.
REFERENCES
1. Vuitch MF, Rosen PP, Erlandson RA. Pseudoangiomatous hyperplasia of mammary stroma. Hum Pathol. 1986;17:185-191. [ Links ]
2. Virk RK, Khan A. Pseudoangiomatous stromal hyperplasia: an overview. Arch Pathol Lab Med. 2010;134:1070-1074. [ Links ]
3. M. Ferreira, C. T. Albarracin, and E. Resetkova, Pseudoangiomatous stromal hyperplasia tumor: a clinical, radiologic and pathologic study of 26 cases, Modern Pathology, vol. 21, no. 2, pp. 201-207, 2008.
4. K. Yoo, O. H.Woo, H. S. Yong et al., Fast-growing pseudoangiomatous stromal hyperplasia of the breast: report of a case, Surgery Today, vol. 37, no. 11, pp. 967-970, 2007.
5. Y. Sasaki, S. Kamata, K. Saito, Y. Nishikawa, and J. I. Ogawa, Pseudoangiomatous stromal hyperplasia (PASH) of the mammary gland: report of a case, Surgery Today, vol. 38, no. 4, pp. 340-343, 2008.
6. C. Anderson, A. Ricci, C. A. Pedersen, and R. W. Cartun, Immunocytochemical analysis of estrogen and progesterone receptors in benign stromal lesions of the breast: evidence for hormonal etiology in pseudoangiomatous hyperplasia of mammary stroma,” American Journal of Surgical Pathology, vol. 15, no. 2, pp. 145-149, 1991
7. S. Pruthi, C. Reynolds, R. E. Johnson, and J. J. Gisvold, Tamoxifen in the management of pseudoangiomatous stromal Hyperplasia,” Breast Journal, vol. 7, no. 6, pp. 434-439, 2001.
8. Singh KA, Lewis MM, Runge RL, Carlson GW, Pseudoangiomatous stromal hyperplasia. A case for bilateral mastectomy in a 12-year-old girl, Breast J. 2007 Nov-Dec;13(6):603-606
9. Badr Abdull Gaffar (2009) Pseudoangiomatous Stromal Hyperplasia of the Breast. Archives of Pathology & Laboratory Medicine: August 2009, Vol. 133, No. 8, pp. 1335-1338.
10. Mizutou A, Nakashima K, Moriya T, Large pseudoangiomatous stromal hyperplasia complicated with gynecomastia and lobular differentiation in a male breast, Springerplus, 2015 Jun 19; 4:282. doi: 10.1186/s40064-015-1083-7 . eCollection 2015
11. Ko SY, Koh MJ. Bilateral diffuse tumorous pseudoangiomatous stromal hyperplasia treated with bilateral mastectomy in a 40-year-old woman. Radiol Case Rep. 2018 Sep 25; 13(6):1271-1275.
12. Samaila MO, Aliyu HO, Yusufu LM, Abdullahi S. Concurrent giant tumoral pseudoangiomatous stromal hyperplasia necessitating bilateral mastectomy. Ann Afr Med. 2018;17(2):82-85. [ Links ]
13. Tumeh RA, Sabino Neto M, Cunha AL, Silva MMA, Paula HR, Ferreira LM. Pseudoangiomatous stromal hyperplasia: rare case in an 11-year-old girl. Rev. Bras. Cir. Plást.2017;32(2):295-298 [ Links ]
14. Krawczyka N; Fehma T; Ruckhäberlea E; Mohrmanna S; Riemerb J; Braunsteinb S; Hoffmanna J. Bilateral Diffuse Pseudoangiomatous Stromal Hyperplasia (PASH) Causing Gigantomastia in a 33-YearOld Pregnant Woman: Case Report. Breast Care 2016;11:356-358 DOI: 10.1159/000450867. [ Links ]
15. Jung BK, Nahm JH, Lew DH, Lee DW. Treatment of Pseudoangiomatous Stromal Hyperplasia of the Breast: Implant-Based Reconstruction with a Vascularized Dermal Sling, Arch Plast Surg. 2015 Sep
16. Dai H, Connor C, Cui W, Gatewood J, Fan F, Bilateral diffuse tumorous pseudoangiomatous stromal hyperplasia: a case of bilateral mastectomy in a 29-year-old woman, Case Rep Pathol. 2014;2014:250608. doi: 10.1155/2014/250608. [ Links ] Epub 2014 Dec 2
17. Travis L. Holloway, MD, and Ismail Jatoi, MD, PhD, Tumorous PASH Presenting as Rapid Unilateral Breast Enlargement, Mayo Clin Proc., July 2013;88(7):e75
18. Muñoz G., Povedano J.L.R., Romero A.L.S. Hiperplasia estromal seudoangiomatosa nodular de mama en dos adolescentes, Radiología. 2012;54(6):549-552. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Bárbara Castelo
Universidade Federal de Juiz de Fora Faculdade de Medicina
Juiz de Fora, Brasil
E-mail: bbcastelo@hotmail.com
Recebido em: 20/02/2019
Aceite para publicação: 06/09/2019