Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Obstétrica e Ginecológica Portuguesa
versión impresa ISSN 1646-5830
Acta Obstet Ginecol Port vol.13 no.3 Coimbra oct. 2019
ISSUE IMAGE/IMAGEM DO TRIMESTRE
Pararretal hematoma after delivery
Hematoma pararetal pós-parto
Mariline Oliveira1, Nuno Vasco Costa2, Olga Alves3
Hospital de Santarém EPE , Centro Hospitalar Lisboa Central
1. Interna de Ginecologia e Obstetrícia
2. Interno de Radiologia
3. Assistente de Ginecologia e Obstetricia
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
A puerperal vulvovaginal hematoma is not an unusual finding after vaginal deliveries. However, most of them are small and self-limited. Even though there are multiple risk factors identified, the majority of cases happen in low risk settings. We here report a case of a nulliparous young woman who developed a massive pararretal hematoma after an uncomplicated vaginal delivery. Surgical intervention was useful but selective embolization was required. Our goal is to highlight the importance of being aware of this potential complication of a vaginal delivery and the need of an early diagnosis in order to offer the most suitable treatment and prevent severe damages.
Keywords: Hematoma; Postpartum period; Therapeutic embolization.
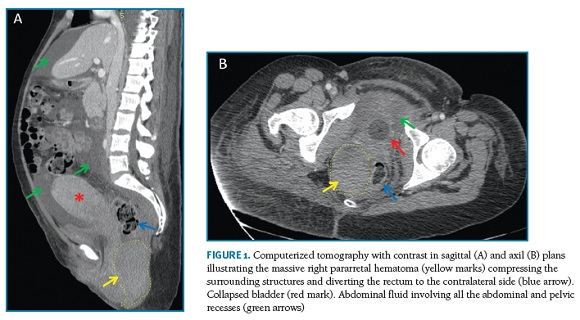
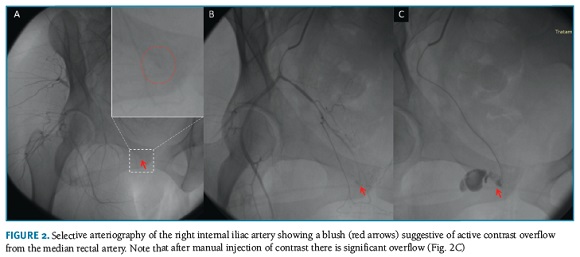
Vulvovaginal hematomas are frequent findings which usually develop spontaneously or after a vascular trauma1. There are multiple established risk factors such as nulliparity, great multiparity, macrossomy, instrumented delivery or coagulation disturbances1,2-5. The diagnosis is mainly clinical1,3. The most common symptoms are intense and spontaneous pain associated with a genital lump and rectal pressure1,3. Due to the epidural analgesic effect the diagnosis could be delayed3. Radiology exams are not essential but they give us a better definition of margins1. Most of vulvovaginal hematomas are self-limited. However, if the hematoma continues to grow, leading to hemodynamic compromise, surgical intervention may be required1-3. The authors report a case of a nulliparous young woman who had a vacum assisted delivery of a 3230g newborn. The right lateral episiotomy was sutured and no other genital lesions were identified. No incidents were reported. A few hours later the woman developed an extensive and painful genital lump on the right side with approximately 8 cm length. After surgical procedure (drainage and coagulation) the hemorrhage was controlled and the patient was home well. Seven days later the genital pain returned associated by an intense retal pressure. On gynecological exam we found a genital lump and a discreet bulging on the right side on rectal examination. The level of hemoglobin drops to 6g/dL. A CT scan was performed and showed an extensive right pararretal hematoma (130x80x65 mm) with compression of the surrounding structures (Figure 1). The patient was referred to a central hospital to perform an angiography which showed an active hemorrhage on a distal branch of the median retal artery (Figure 2). The bleeding was controlled after selective embolization. One week later she went home asymptomatic.
This report presents a rare evolution of a vaginal hematoma resolved only with a selective embolization.
REFERENCES
1. Bienstman-Pailleux J, Huissoud C, Dubernard G, Rudigoz RC. [Management of puerperal hematomas]. J Gynecol Obstet Biol Reprod (Paris). 2009;38(3):203-8 [ Links ]
2. Lee SL, Kim YH, Lee HJ. Selective angiographic embolisation of an infralevator vulvovaginal haematoma after birth: case report. J Obstet Gynaecol. 2015;35(6):639-40 [ Links ]
3. Iskender C, Topcu HO, Timur H, Oskovi A, Goksu G, Sucak A, et al. Evaluation of risk factors in women with puerperal genital hematomas. J Matern Fetal Neonatal Med. 2016;29(9):1435-9 [ Links ]
4. Fargeaudou Y, Soyer P, Morel O, Sirol M, le Dref O, Boudiaf M, et al. Severe primary postpartum hemorrhage due to genital tract laceration after operative vaginal delivery: successful treatment with transcatheter arterial embolization. Eur Radiol. 2009;19(9):2197-203 [ Links ]
5. Rani S, Verma M, Pandher DK, Takkar N, Huria A. Risk Factors and Incidence of Puerperal Genital Haematomas. J Clin Diagn Res. 2017;11(5):QC01-QC3 [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Mariline Oliveira
Hospital Santarém EPE, Portugal
E-mail: m.eudora@gmail.com
Recebido em: 31/01/2019
Aceite para publicação: 19/02/2019