Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.12 no.3 Coimbra set. 2018
ISSUE IMAGE/IMAGEM DO TRIMESTRE
Adnexal masses: a true challenge
Massas anexiais: um verdadeiro desafio
Joana Lopes Pereira*, Maria Júlia Pereira**, Manuel Morim**
Centro Hospitalar S. João, Porto, Portugal
Centro Hospitalar Póvoa de Varzim e Vila do Conde, Póvoa de Varzim, Portugal
*Interna de Formação Específica de Ginecologia e Obstetrícia
**Assistente Hospitalar Graduado
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Preoperative diagnosis of adnexal masses is still one of the greatest challenges for gynaecologists. Even though the majority of adnexal neoformations are benign, a careful evaluation to exclude malignancy is mandatory. The rapid evolution in the field of ultrasonography increased diagnostic accuracy and magnetic resonance imaging provides a valid contribution, but still, sometimes, the distinction between malignant and benign is difficult. We report a case of a premenopausal women who presented with a large and painful abdominal mass four months after an emergent caesarean delivery.
Keywords: Adnexal masses; Ultrasound; MRI.
Description
Adnexal masses concern lesions of the ovary, tube and ligaments. Ovarian neoplasms arise from the surface epithelium, germ cells, or sex-cord-stromal tissue and may be benign, malignant or borderline.1 The prevalence of ovarian cysts is 6.6% 2 and the majority are benign. Clinical presentation is variable with masses often identified during routine evaluations. Ultrasound is an important tool to assess adnexal masses. In fact, in 90% of cases a correct characterization is possible based on ultrasound features.3 When the diagnose is challenging, such as in complex masses, magnetic resonance imaging (MRI) is a valuable resource and should be considered when ultrasound is not conclusive.4 We present a case that illustrates the difficulty of pre-dicting the risk of malignancy of an adnexal mass pre-operatively and how important the collaboration of a multidisciplinary team is in the management of these cases.
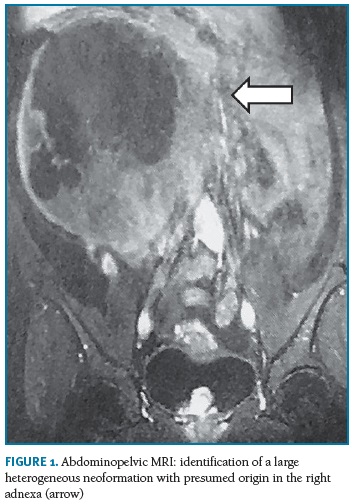
A 33-year-old primiparous woman, healthy, was complained to her assistant physician of pelvic discomfort. She had had an emergency caesarean four months before due to an intrapartum nonreasurring fetal heart rate, which was uneventful. On physical examination, she had a palpable, large mass on the right hypochondrium and was referred to our institution for further assessment. The abdominal ultrasound performed described a heterogeneous mass, predominantly solid, with a diameter of 17 cm, apparently originating from the right adnexal area. CA 125 was elevated (345.9 U/L). An abdominopelvic MRI confirmed the findings and indicated right adnexal origin as the most likely origin. During evaluation, the mass increased its volume and became symptomatic, with two hospitalizations for pain control. Given the high suspicion of malignancy, surgical excision with extemporaneous examination was proposed and accepted. The surgical team performed a right oophorectomy by laparotomy and the extemporaneous examination of the specimen revealed a “… stromal neoplasm without malignancy – probable fibroid…”. This was later confirmed by definite histological examination of the whole ovary. There were no further complications and the patient was referred to her assistant physician.
This case illustrates how difficult and misleading pre-operative diagnosis of adnexal masses may be. Ultrasound accurately assesses most ovarian cysts but when doubts remain MRI may be helpful. There are some characteristics and imaging features which may trigger malignancy suspicion.5 The heterogenous solid appearance and rapid growth were in favour of a non-benign etiology; the elevated CA 125 must be interpreted with caution, since it as low specificity and false positives are frequent when other gynaecological diseases are present. In these cases, surgery must be not only therapeutic but also diagnostic – it should include and extemporaneous examination and, if necessary, staging surgery. Therefore, a careful discussion with the patient is important and written informed consent is necessary. Of course, fertility related issues are important, and when possible, in younger women, conservative surgery should be considered.
When managing adnexal masses, imaging features, risk factors and predictive models should guide our decisions but very often we are surprised by the definitive findings. Hence, high clinical suspicion and follow-up with a multidisciplinary team are key to success.
REFERENCES
1. Oncology FCoG. FIGO's staging classification for cancer of the ovary, fallopian tube, and peritoneum: abridged republication. J Gynecol Oncol. 2015;26(2):87-89. [ Links ]
2. Borgfeldt C, Andolf E. Transvaginal sonographic ovarian findings in a random sample of women 25-40 years old. Ultrasound Obstet Gynecol. 1999;13(5):345-350. [ Links ]
3. Valentin L, Ameye L, Jurkovic D, Metzger U, Lecuru F, Van Huffel S, Timmerman D. Which extrauterine pelvic masses are difficult to correctly classify as benign or malignant on the basis of ultrasound findings and is there a way of making a correct diagnosis? Ultrasound Obstet Gynecol. 2006;27(4):438-444. [ Links ]
4. Saini A, Dina R, McIndoe GA, Soutter WP, Gishen P, deSouza NM. Characterization of adnexal masses with MRI. AJR Am J Roentgenol. 2005;184(3):1004-1009. [ Links ]
5. Timmerman D, Testa AC, Bourne T, Ameye L, Jurkovic D, Van Holsbeke C, Paladini D, Van Calster B, Vergote I, Van Huffel, S, Valentin L. Simple ultrasound-based rules for the diagnosis of ovarian cancer. Ultrasound Obstet Gynecol. 2008;31(6):681-690. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Joana Lopes Pereira
Centro Hospitalar de Sao João EPE
Portugal
E-Mail: joanaslopespereira@gmail.com
Recebido em: 27/11/2017
Aceite para publicação: 10/04/2018